Table of Contents
Core Anatomy
- Note generations of the tracheal-bronchial tree, lobes, segments,
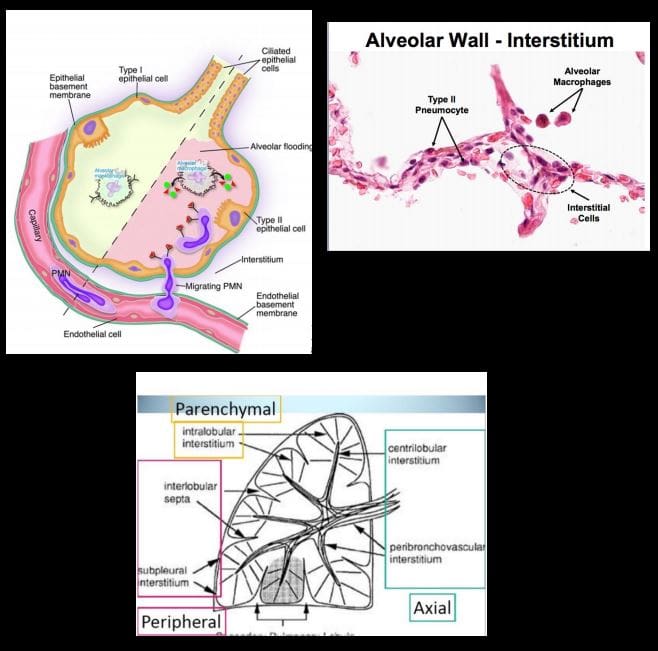
and fissures. Note secondary pulmonary lobule (1.5-2-cm)-the basic functional unit of lungs observed on HRCT. Note important structural organization of the alveolar spaces with communications in between (pores of Kohn & canals of Lambert) that permit air drift and by the same mechanism allow exudative ortransudative fluid to spread through the lung and stopped at the fissure. Note the anatomy of the pleura: parietal that is a part of theendothoracic fascia and the visceral that forms alung edge. Pleural space in between.
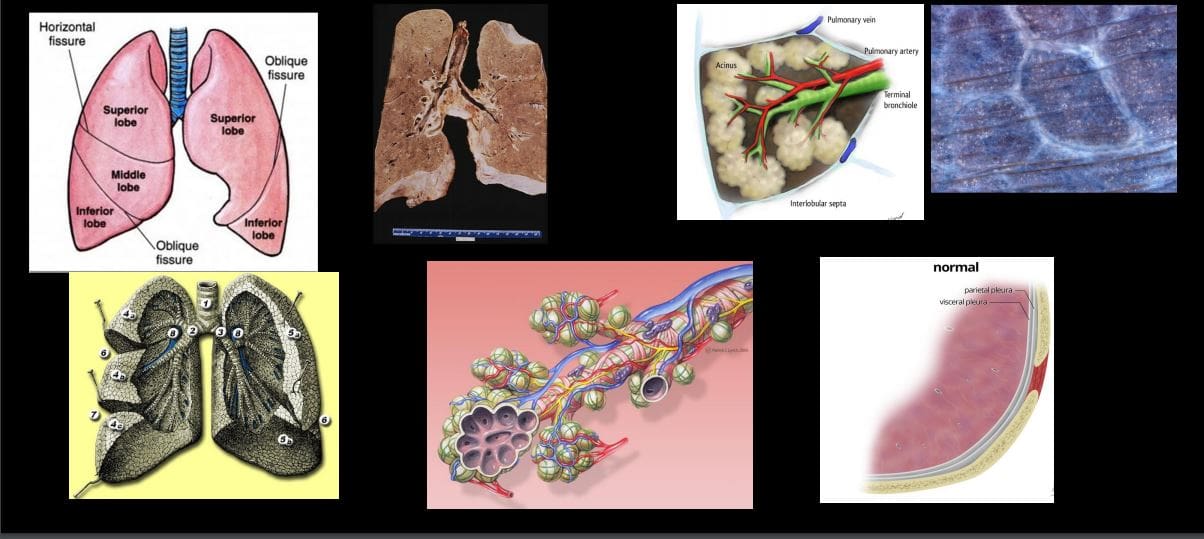
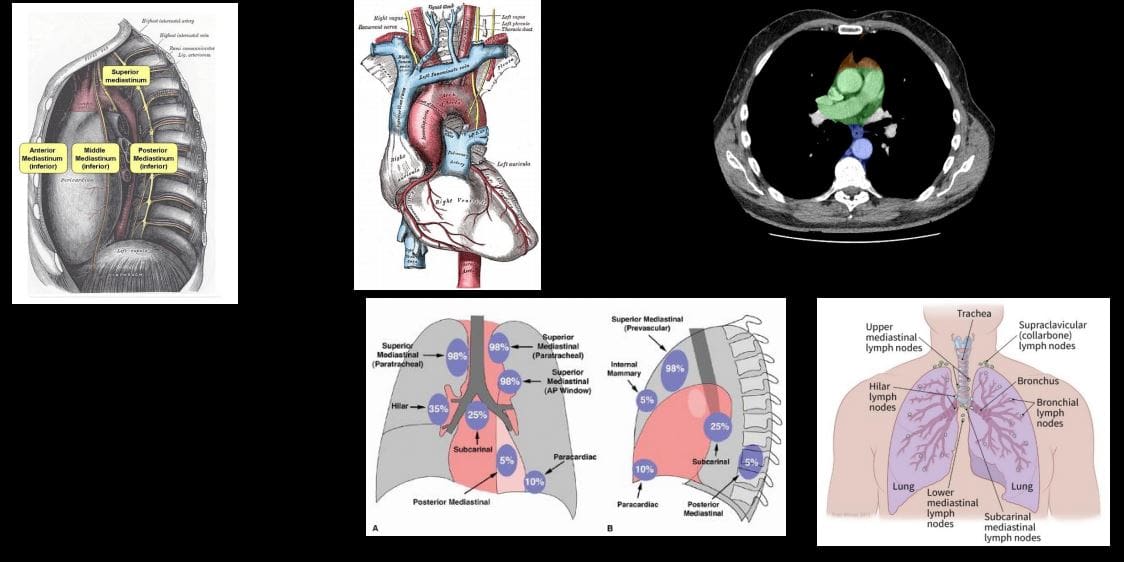
- Mediastinum: surrounded by the pleura and the lung. Accommodates major structures contains numerous lymph nodes (see diagramme showing mediastinal nodes and their involvement in Lymphoma
General Approach to Investigating Chest Complaints
- Radiographic examination (Chest X-ray CXR); excellent 1st step. Low cost, low radiation exposure, multiple clinical complaints evaluation
- CT scanning: chest CT, High-Resolution CT (HRCT)
- Chest pathology approach:
- Trauma
- Infection
- Neoplasms
- Pulmonary edema
- Pulmonary emphysema
- Atelectasis
- Pleural pathology
- Mediastinum
PA & Lateral CXR
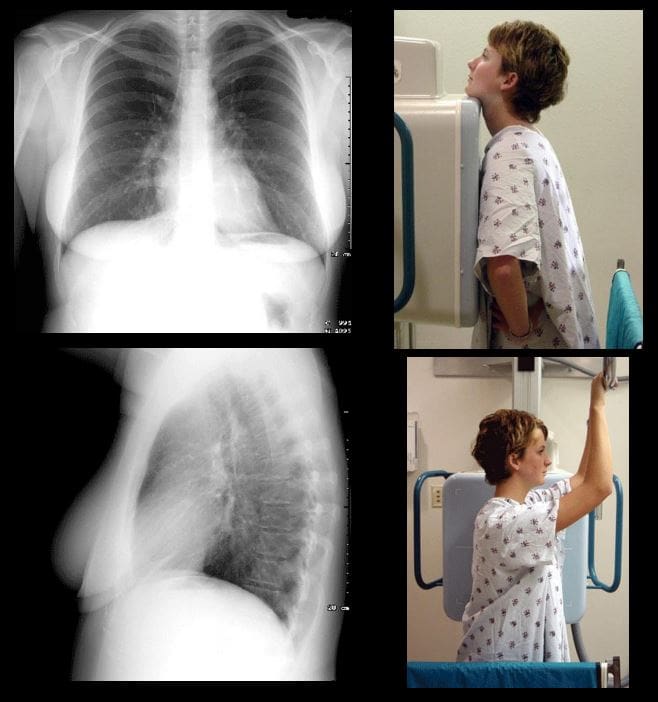
- Additional views may be used:
- Lordotic view: helps to evaluate apical regions
- Decubitus views right and left: help to evaluate subtle pleural effusion, pneumothorax and other pathology
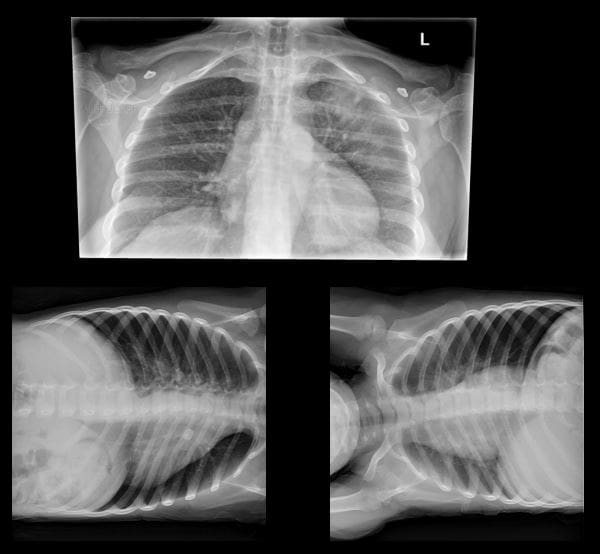
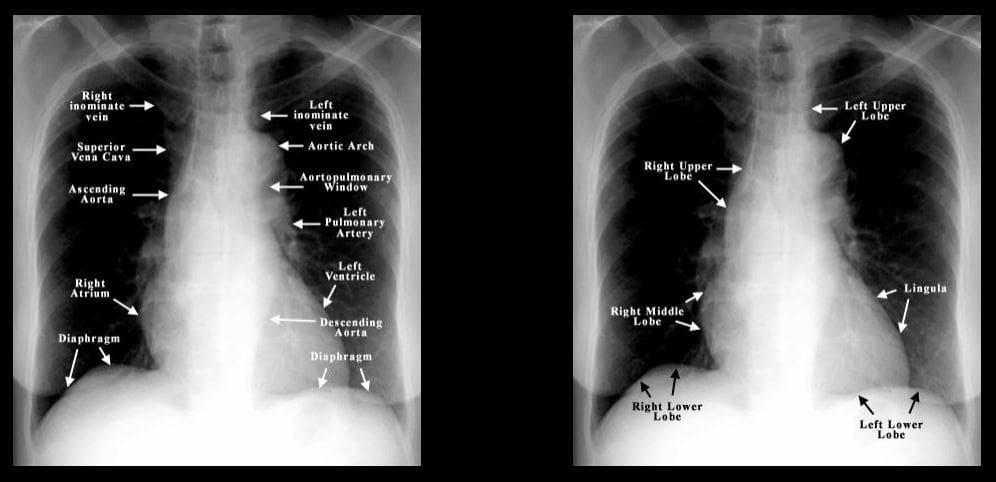
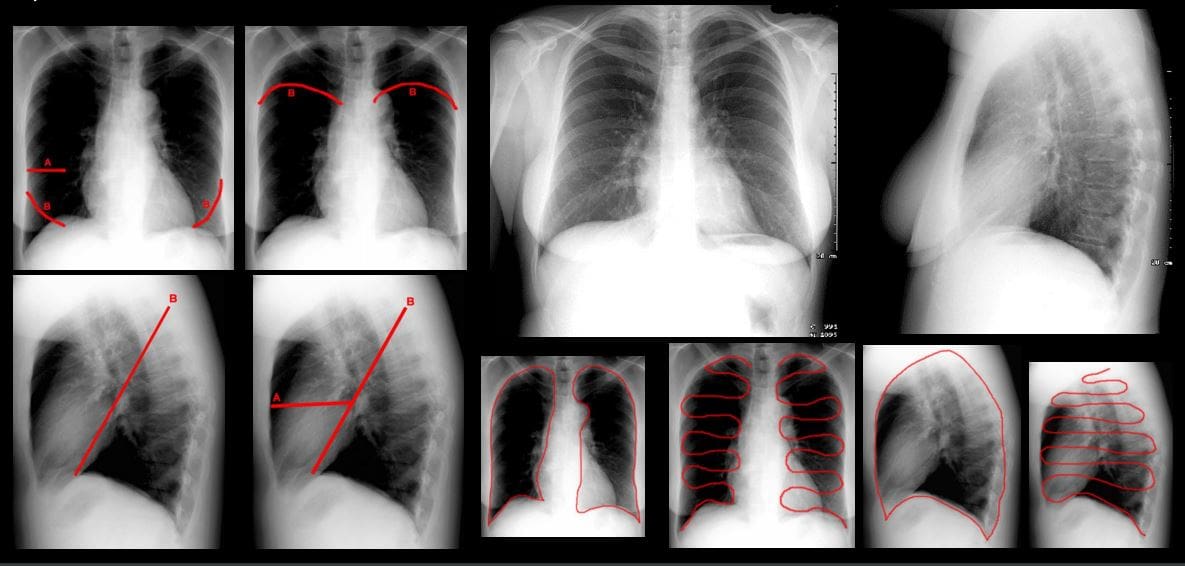
- Normal CXR PA & Lateral views. Ensure good exposure: T-spine discs and vessels through the heart are visualized on PA view. Count 9-10 right posterior ribs to confirm adequate inspiratory effort. Begin careful survey using the following approach: Are There Many Lung Lesions A-abdomen/diaphragm, T-thorax wall, M-mediastinum, L-lungs individually, Lungs-both. Develop a good search pattern
- 1)
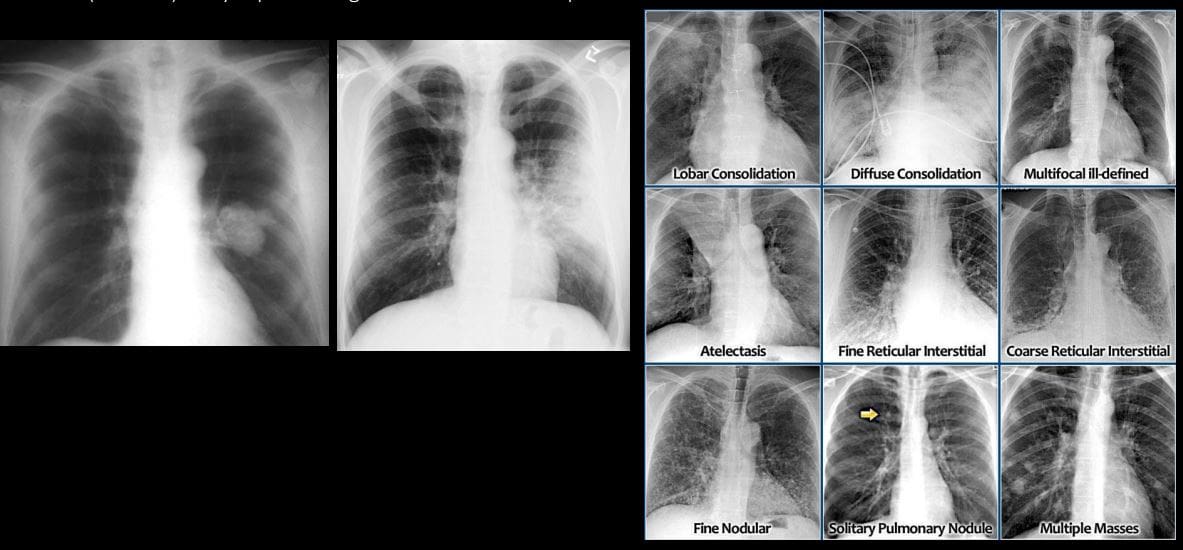
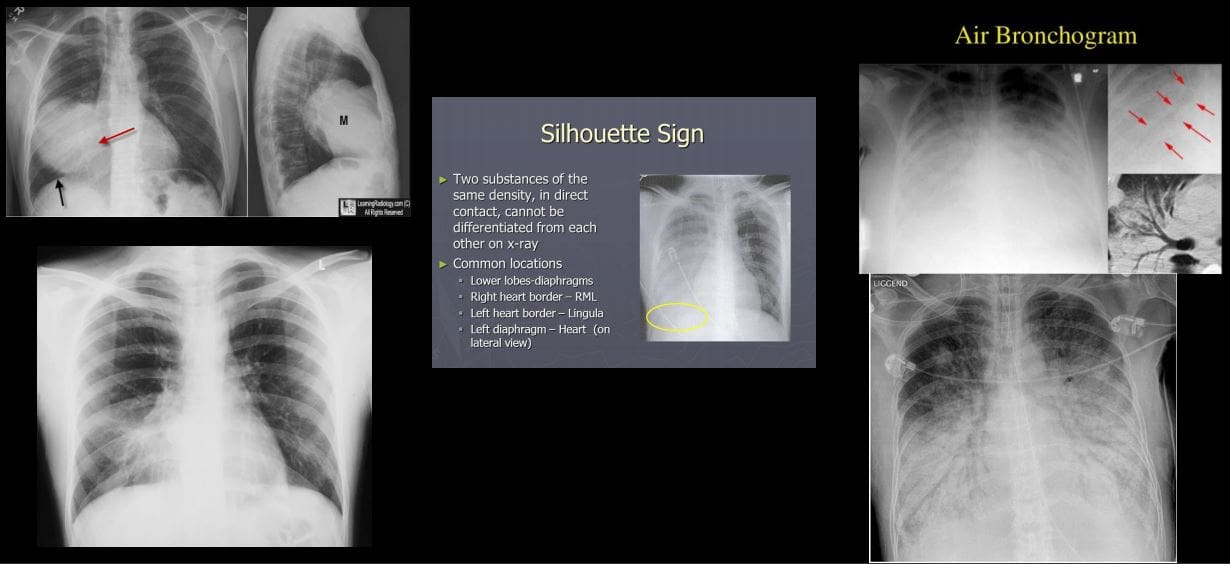
Air space disease aka alveolar lung disease? filling of the lung’s alveoli, acini and subsequently the entirelobe with fluid or substance of any composition (blood, pus, water,proteinacious material or even cells) Radiographically: lobar or segmental distribution, airspace nodules may be noted, tendency to coalesce, air bronchograms and silhouette sign present.Bat wing (butterfly) distribution noted as in (CHF). Rapidly changing over time i.e. increase or decrease (days) - 2) Interstitial disease: infiltration of pulmonary interstitium (alveoli septum, lung parenchyma, vessel walls etc.) by for example by viruses, small bacteria, protozoans. Also infiltration by cells such as inflammatory/malignant cells (e.g. lymphocytes) Presented as
accentuation of lung interstitium withreticular , nodular, mixedreticulo-nodular pattern. Different etiologies: inflammatory autoimmune diseases, fibrosing lung disease, occupational lung disease, viral/mycoplasma infection, TB, sarcoidosis lymphoma/leukemia and many other.
- Recognising different patterns of pulmonary disease can help with DDx. Mass vs Consolidation (left). Note different patterns of pulmonary disease: air space disease as lobar consolidation indicative of pneumonia, diffuse consolidation indicative of pulmonary edema. Atelectasis (collapse and volume loss). Interstitial patterns of pulmonary disease: reticular, nodular or mixed. SPN vs. Multiple focal consolidations (nodules) likely representing mets infiltrates vs. septic infiltrates
- A = intraparenchymal
- B = pleural
- C = extrapleura
- Recognize important location of chest lesions

- Important signs: Silhouette sign: help with localization and DDx. Example: Bottom left image: radiopacity in the right lung, where is it located? Right MM because the right heart border that is adjacent to right middle lobe is not seen (silhouetted) Air bronchograms: air containing bronchi/bronchioles surrounded by fluid
Chest Trauma
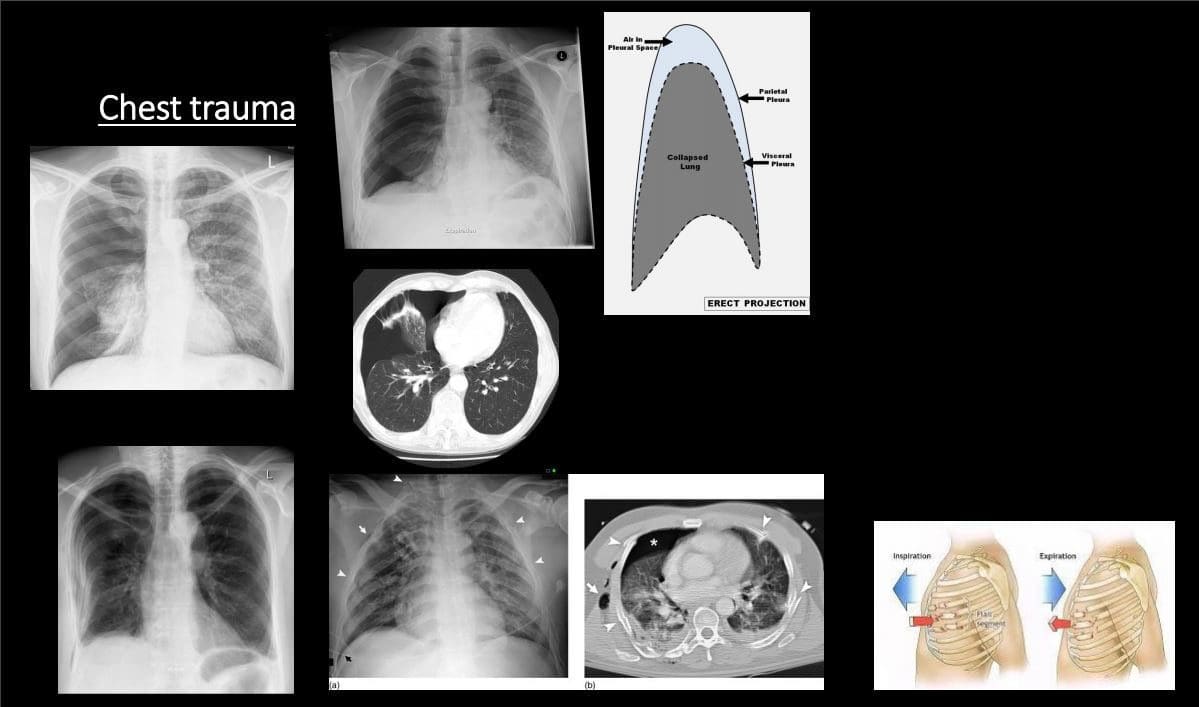
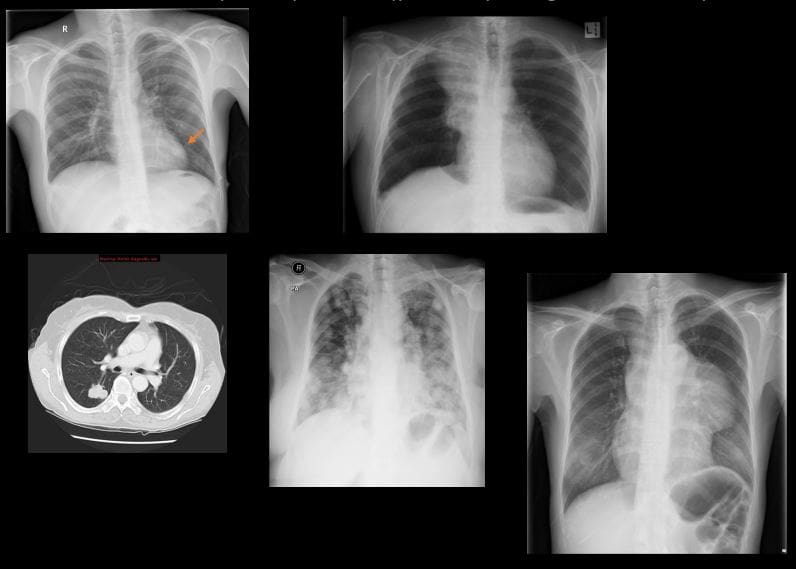
- Pneumothorax (PTX): air (gas) in the pleural space. Many causes. Complications:
- Tension PTX: continuous increase of air in the pleural space that rapidly compresses mediastinum and lung rapidly reducing venous return to the heart. It can be fatal if not treated rapidly
- Spontaneous PTX: primary (young adults (30 -40) especially tall, thin men. Additional causes: Marfan’s syndrome, EDS, Homocystinuria, a – 1 -antitrypsin deficiency. Secondary: older pts with parenchymal disease: neoplasms, abscess, emphysema, lung fibrosis and honeycombing, catamenial PTX d/t endometriosis and others.
- Traumatic pneumothorax: lung laceration, blunt trauma, iatrogenic (chest tubes etc.) acupuncture etc.
- CXR: note visceral pleural line aka lung edge. An Absence of pulmonary tissue/vessels beyond the visceral pleural line. Subtle pneumothorax can be missed. On erect position, air rises and PTX should be sought at the top.
- Rib fractures: v.common. Traumatic or pathological (e.g. mets, MM) Rib series x – rays are not very useful because CXR and/or CT scanning are more important to evaluate post -traumatic PTX (bottom left) lung laceration and other major path
Infection
- Pneumonia: bacterial vs. viral or fungal or in the immunocompromised host (e.g. Cryptococcus in HIV/AIDS) Pulmonary TB
- Pneumonia: community-acquired vs. hospital-acquired. Typical bacterial pneumonia or Lobar (non-segmental) pneumonia with purulent material filling the alveoli and spreading to the entire lobe. M/C organismStreptococcus Pneumonia or the Pneumococcus
- Others: (Staph, Pseudomonas, Klebsiella esp. in alcoholics potentially leading to necroSIS/lung gangrene) Mycoplasma (20-30s) aka walking pneumonia etc.
- Clinically: a productive cough, fever, pleuritic chest pain sometimes hemoptysis.
- CXR: confluent airspace opacity confined to the entire lobe. Air bronchograms. Silhouette sign help with location.
- Viral: Influenza, VZV, HSV, EBV, RSV etc. presents as interstitial lung disease that can be bilateral. May lead to respiratory compromise
- Atypical pneumonia and Fungal Pneumonia: Mycoplasma, Legionnaire’s disease, and some fungal/Cryptococcus pneumonia may present with interstitial lung disease.
- Pulmonary abscess: an infectious collection of purulent material in the lungs that often necrotizes. May lead to major pulmonary and system complications/life-threatening.
- On CXR or CT: round collection with thick borders and central necrosis containing air-fluid level. DDx from empyema that distorts the lung and pleural-based
- Rx: antibiotics, antifungal, antiviral agents.
- Pneumonia needs to be followed up with repeat CXR to ensure complete resolution
- Lack of radiographic improvement of pneumonia may represent declined immunity, antibiotic resistance, underlying lung carcinoma or other complicating factors
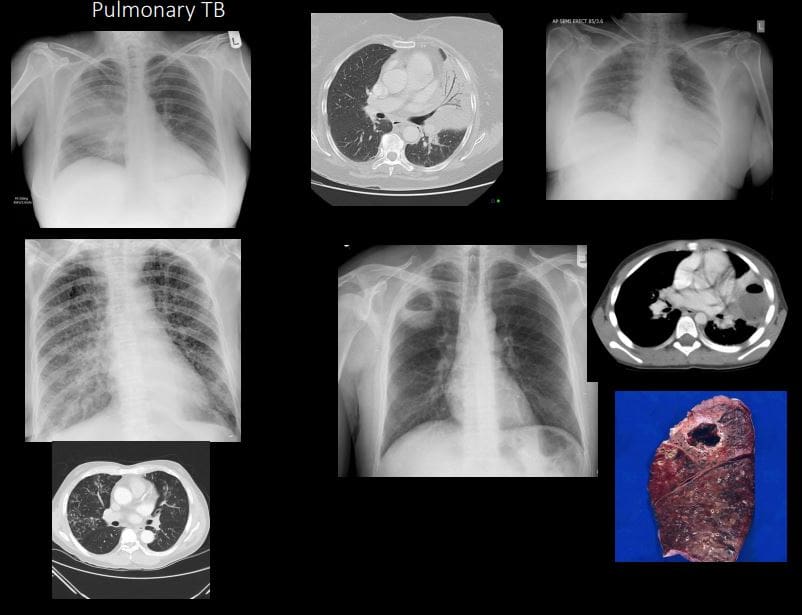
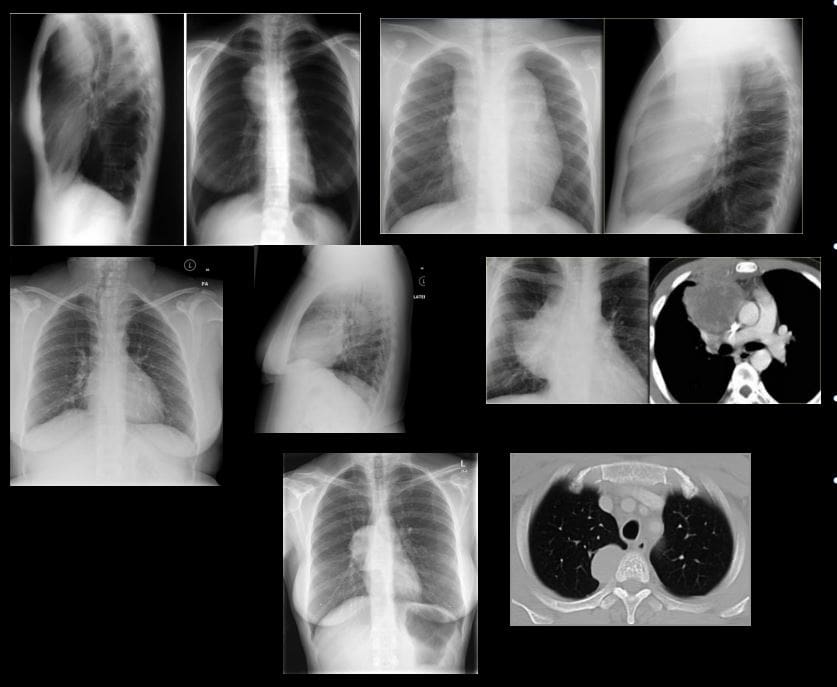
Pulmonary TB
- Common infection worldwide (3rd world countries). 1 in 3 persons worldwide is affected by TB. TB is caused by Mycobacterium TB or Mycobacterium Bovis. Intracellular bacillus. Macrophage plays a key role.
- Primary Pulmonary TB & Post-primary TB. Requires repeated exposure through inhalation. In most immunocompetent hosts, the active infection does not develop
- TB presents as 1) cleared by the host, 2) suppressed into Latent Tuberculosis Infection (LTBI) 3) cause active disease TB. Patients with LTBI are not spreading TB.
- Imaging: CXR, HRCT. Primary TB: pulmonary airspace consolidation (60%) lower lobes, lymphadenopathy (95%- hilar & paratracheal), pleural effusion (10%). The Spread of primary TB most likely in immunocompromised and children.
- Milliary TB: pulmonary and system complication dissemination that can be fatal
- Post-primary (secondary) or reactivation infection: Mostly in the Apices and posterior segments of the upper lobes )high PO2), 40%-cavitating lesions, patchy or confluent airspace disease, fibrocalcific. Latent features: nodal calcifications.
- Dx: Acid-fast bacilli (AFB) smear and culture (sputum). HIV serology in all patients with TB and unknown HIV status
- Rx: 4-drug regimen: isoniazid, rifampin, pyrazinamide, and either ethambutol or streptomycin.
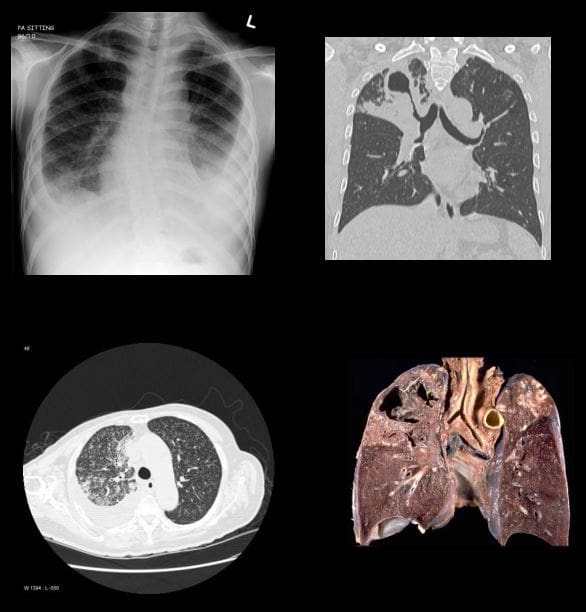
Pulmonary Neoplasms (primary lung cancer vs. pulmonary metastasis)
- Lung cancer: m/c cancer in men and 6th most frequent cancer in women. Strong association with carcinogens inhalation. Clinically: late discovery, depending on the location of the tumor. Pathology (types): Small cell (SCC) vs. Non-small cell carcinoma
- Small cell: (20%) develops from neuroendocrine aka Kultchitsky cell, thus may secrete biologically active substances presenting with paraneoplastic syndrome. Typically located centrally (95%) at or near the mainstem/lobar bronchus. Most show poor prognosis and unresectable.
- Non-small cell: Lung adenocarcinoma (40%) (M/C lung cancer), M/C in women and non-smokers. Others: Squamous cell (may present with cavitating lesion), Large cell and some others
- Plain film (CXR): new or enlarged focal lesion, widened mediastinum suggestive of lymph node involvement, pleural effusion, atelectasis, and consolidation. SPN-may represents potential lung cancer. especially if contains irregular borders, feeding vessels, thick wall, in upper lungs. Multiple lung nodules likely to represent metastasis.
- Best Modality: HRCT with contrast.
- Other chest neoplasms: Lymphoma is v. common in the chest especially in mediastinal and internal mammary notes.
- Overall M/C pulmonary neoplasms are metastasis. Some tumors show a higher predilection for lung mets e.g. Melanoma but any cancer can metastasize to the lungs. Some mets referred as “Cannonball” metastasis
- Rx: radiation, chemotherapy, resection
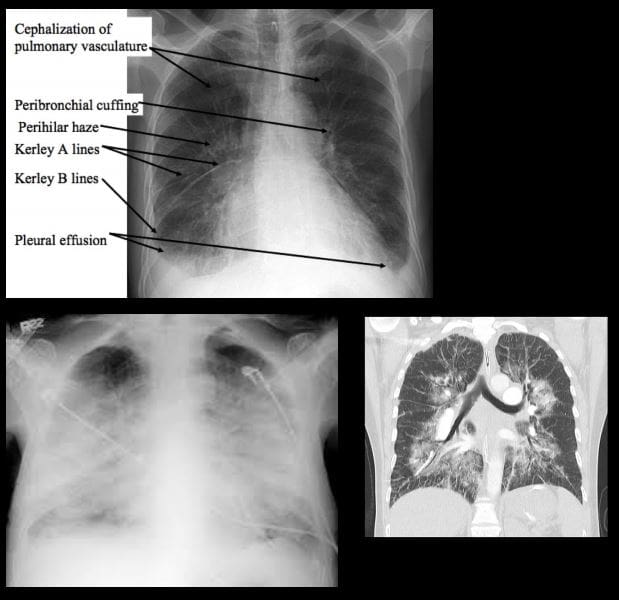
- Pulmonary edema:
general term defines abnormal fluid accumulation outside vascular structures. Broadly dividedinto: Cardiogenic (e.g. CHF, mitral regurgitation) and Non-cardiogenic withmultitude of causes (e.g. fluid overload, post-transfusion, neurological causes, ARDS, near drowning/asphyxiation, heroin overdose, and others) - Causes: increased in Hydrostatic pressure vs. decreased in oncotic pressure.
- Imaging: CXR and CT: 2-types Interstitial and Alveolar flooding. Imaging presentation depends on
stages - In CHF: Stage 1: redistribution of vascular flow (10- 18-mm Hg) noted as “cephalization” of
pulmonary vasculature. Stage 2: Interstitial edema (18-25-mm Hg) Interstitial edema: peribronchial cuffing, Kerley lines (lymphatics filled with fluid) A,B , C lines. Stage 3: Alveolar edema: airspace disease: patchy consolidations developing into diffuse airspace disease: Bat wing edema, air bronchograms - Rx: 3 main goals: Initial O2 to keep O2 at 90% saturation
- Next: (1) reduction of pulmonary venous return (preload reduction), (2) reduction of systemic vascular resistance (afterload reduction), and (3) inotropic support. Treat underlying causes (e.g. CHF)
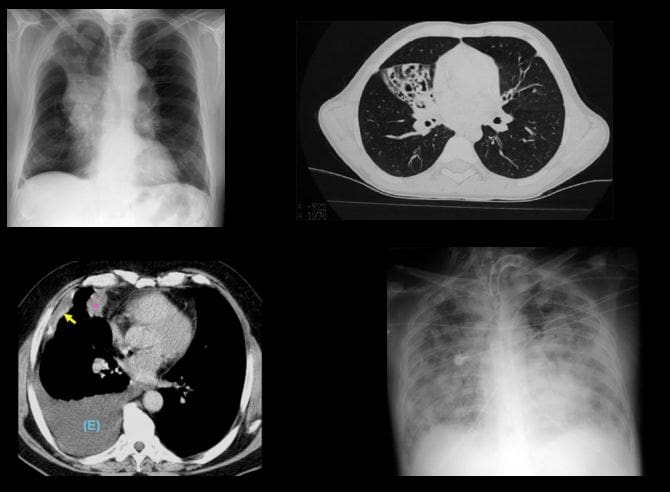
- Lung atelectasis: incomplete expansion of pulmonary parenchyma. The term “collapsed lung” is typically reserved for when the entire lung is totally collapsed
- 1) Resorptive (obstructive) atelectasis occurs as a result of complete obstruction of an airway (e.g. tumor, inhaled objects etc.)
- 2) Passive (relaxation) atelectasis occurs when contact between the parietal and visceral pleura is disrupted (pleural effusion & pneumothorax)
- 3) Compressive atelectasis occurs as a result of any thoracic space-occupying lesion compressing the lung and forcing air out of the alveoli
- 4) Cicatrical atelectasis: occur as a result of scarring or fibrosis that reduces lung expansion as in granulomatous disease, necrotizing pneumonia, and radiation fibrosis
- 5) Adhesive lung atelectasis occurs from surfactant deficiency and alveolar collapse
- 6) Plate-like or discoid often developed after following general anesthesia
- 7) Imaging features: lung collapse, migration of lung fissures, deviation of the
mediastinum , rising of the diaphragm, hyperinflation of adjacent unaffected lung
- Mediastinum: pathology can be divided into those that result in a focal mass or those that result in diffuse disease involving the mediastinum. Additionally, air may track into the mediastinum in pneumomediastinum. Knowledge of mediastinal anatomy helps the Dx.
- Anterior mediastinal masses: thyroid, thymus, teratoma/germ cell tumors, lymphoma, lymphadenopathy, ascending aortic aneurysms
- Middle mediastinal masses: lymphadenopathy, vascular, bronchial lesions etc.
- Posterior mediastinal masses: neurogenic tumours, aortic aneurysms, esophageal masses, spinal masses, aortic chain adenopathy
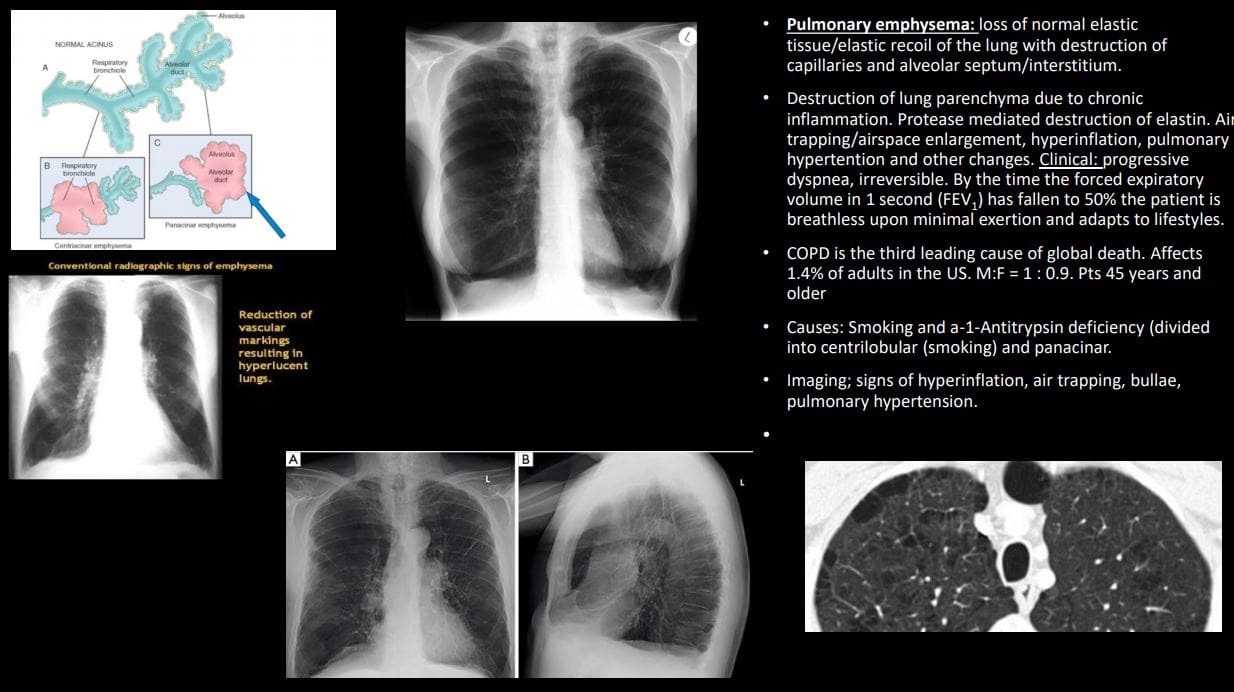
- Pulmonary emphysema: loss of normal elastic tissue/elastic recoil of the lung with the
destruction of capillaries and alveolar septum/interstitium. - Destruction of lung parenchyma due to chronic inflammation. Protease-mediated destruction of elastin. Air trapping/airspace enlargement, hyperinflation, pulmonary hypertension, and other changes. Clinical: progressive dyspnea, irreversible. By the time the forced expiratory volume in 1 second (FEV1 ) has fallen to 50% the patient is breathless upon minimal exertion and adapts to lifestyles.
- COPD is the third leading cause of global death. Affects 1.4% of adults in the US. M:F = 1 : 0.9. Pts 45 years and older
- Causes: Smoking and a-1-Antitrypsin deficiency (divided into centrilobular (smoking) and panacinar.
- Imaging; signs of hyperinflation, air trapping, bullae, pulmonary hypertension.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


