For women experiencing lower back and pelvic pain, could understanding symptoms help in the diagnostic process, treatment options, and prevention?
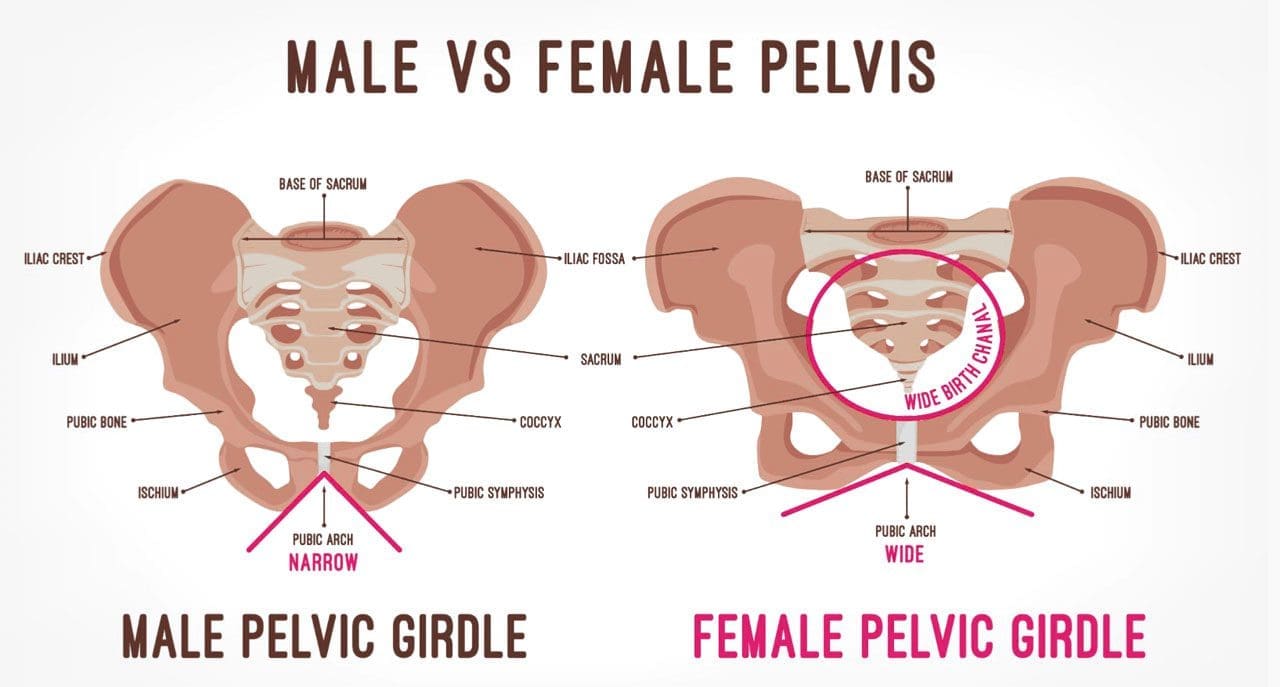
Table of Contents
Low Back and Pelvic Pain In Women
In women, lower back and hip pain that radiates to the front pelvis area can have a variety of causes. The pain can feel dull, sharp, or burning. The main causes of lower back and pelvic pain in women fall into two categories. (William S. Richardson, et al., 2009)
Musculoskeletal and nervous system
- Related causes of pain affect how your muscles, nerves, ligaments, joints, and bones move.
- Examples include sciatica, arthritis, and injury.
Other organ system-based
Causes may stem from the following:
- Acute/chronic conditions or infections
- Kidneys – stones, infection, and other ailments or conditions.
- Reproductive system – such as the ovaries.
- Gastrointestinal system – inguinal hernias or appendix.
Musculoskeletal and Nervous System Causes
Musculoskeletal and nervous system-related causes can be from injuries like a fall or practicing unhealthy posture.
Overuse Injuries and Trauma
Frequent use and repetitive movements can lead to overuse injuries to the muscles, ligaments, and joints. :
- Exercises, sports, and physical activities that require repetitive twisting and bending.
- Lifting, carrying, and placing objects that require movements that are repeated regularly.
- Trauma from vehicle collisions, accidents, falls, or sports accidents can inflict acute and chronic bodily injuries, like strained muscles or broken bones.
- Depending on the type of trauma, healing and recovery time and treatment vary.
- Both types of injuries can lead to numbness, tingling, pain, stiffness, popping sensations, and/or weakness in the legs.
Mobility Problems
Over time, a decreased range of motion and mobility in muscles and joints can cause discomfort and pain. Causes include:
- Long periods of time spent in the same position.
- Sitting for extended periods.
- The pain often feels dull, achy, and stiff.
- It can also lead to muscle spasms characterized by quick episodes of sharp and intense pain.
Posture
- Posture while sitting, standing, and walking affects the body’s range of motion.
- It can affect the nerves and blood circulation to the back and pelvic region.
- Prolonged unhealthy postures can contribute to lower back pain and muscle strain.
- Posture-related symptoms can feel achy and stiff and lead to quick episodes of severe or intense pain, depending on the position.
Sciatica and Nerve Compression
- A bulging or herniating vertebral disc most commonly causes sciatica and pinched or compressed nerves.
- The sensations can be sharp, burning, electrical, and/or radiating pain along the nerve pathway.
Arthritis
- Arthritis inflammation causes swelling, stiffness, pain, and the breakdown of cartilage that cushions the joints.
- Hip arthritis causes groin pain that can radiate to the back and becomes more intense when standing or walking.
- Thoracic and lumbar spine arthritis, or degenerative disc disease, are other common causes of back pain.
Sacroiliac Joint Dysfunction
- The sacroiliac joints connect the lower spine and pelvis.
When these joints move too much or too little, it can cause sacroiliac joint pain, leading to a burning sensation in the lower back and pelvic area. (Daisuke Kurosawa, Eiichi Murakami, Toshimi Aizawa. 2017)
Renal and Urinary Causes
Kidney Stones
- Kidney stones are the build-up of minerals and salts, which form into hard stones in the kidneys.
- When the kidney stone begins to move to the bladder, pain symptoms will present.
- It can trigger severe back and side pain that radiates to the pelvic region.
- Other symptoms include – a change in urine color, pain when urinating, nausea, and vomiting.
Kidney Infection and Urinary Tract Infections
- Urinary tract and kidney infections are also causes of lower back and pelvic pain in women.
- They cause fever, continued urge to urinate, and painful urination.
Gynecological Causes
Pelvic Inflammatory Disease
Infections, known as pelvic inflammatory disease, occur when sexually transmitted bacteria spread through the vagina, womb, fallopian tubes, or ovaries. Symptoms include:
- Pain during intercourse.
- Bleeding between periods.
- Vaginal discharge.
- Pain in the lower abdomen or groin.
- Fever.
Ovarian Cysts
- The cyst can be a solid or fluid-filled sac on the surface or within an ovary.
- Small ovarian cysts are unlikely to cause pain.
- Large cysts or those that rupture can cause mild to severe pain.
- The pain can occur during menstruation or intercourse and present acutely in the back, pelvis, or lower abdomen.
During Pregnancy
- Back pain and discomfort in the pelvis area are common.
- As the body adjusts, the bones and round ligaments in the pelvis move and stretch, which can cause discomfort.
- Symptoms are usually normal but should be discussed with a healthcare provider during check-ups.
- Pain in the lower back and groin can be a sign of miscarriage or labor – including preterm labor.
Sexually Transmitted Infection
- Sexually transmitted infections, like chlamydia or gonorrhea, can cause lower back and groin pain.
- Other symptoms can include – painful urination, vaginal discharge, intercourse pain, and bleeding between periods.
Yeast Infection
- A yeast infection – overgrowth of the fungus candidiasis.
- A common vaginal infection with symptoms including – itching, swelling, irritation, and pelvic pain.
Other Causes
Appendicitis
- When the appendix becomes blocked, infected, and inflamed.
- In most cases, a major symptom is pain that starts near or around the belly button.
- In other cases, it can start in the lower back and radiate to the right side of the pelvic area. (Johns Hopkins Medicine. 2023)
- Associated pain can worsen over time or when coughing, moving, or taking deep breaths.
Other symptoms include:
- Upset stomach
- Nausea
- Vomiting
- Loss of appetite
- Fever
- Chills
- Abnormal bowel movements – constipation and/or diarrhea. (Johns Hopkins Medicine. 2023)
Inguinal Hernia
- A groin hernia is referred to an inguinal hernia.
- It involves soft tissue and part of the intestine, pushing through weak groin muscles.
- Pain presents in the abdomen, lower back, or pelvis, especially when bending or lifting objects.
Pancreatitis
- Inflammation in the pancreas.
- Infection, bile stones, or alcohol can cause it.
- One symptom is abdominal pain that radiates to the back.
- The pain becomes worse during and after eating.
- Other symptoms include nausea, vomiting, and fever.
Enlarged Lymph Nodes
- Lymph nodes lie in the internal and external regions of the iliac artery in the pelvis.
- These can become enlarged by infection, injury, and, in rare cases, cancer.
- Symptoms include pain, swelling, redness, skin irritation, and fever.
Enlarged Spleen
- The spleen is located behind the left side of the rib cage.
- It filters the blood and supports new blood cell creation.
- Infections and diseases can cause the spleen to become enlarged.
- An enlarged spleen – a condition known as splenomegaly – causes pain in the upper left part of the belly and sometimes the left shoulder and upper back.
- However, some individuals with an enlarged spleen experience abdominal symptoms – not being able to eat without discomfort. (Mount Sinai. 2023)
Diagnosis
- Depending on the cause of your pain, a healthcare provider may be able to diagnose it with a physical exam and by asking questions about your condition.
- Other tests may be needed to find the cause, particularly blood work and imaging (X-ray or magnetic resonance imaging).
Treatment
- Treatment of symptoms depends on the cause.
- Once a diagnosis is made, an effective treatment plan will be developed and contain a combination of therapies:
Lifestyle Adjustments
- For injuries caused by muscle strains, joint sprains, overuse, and smaller traumas, pain can be resolved with:
- Rest
- Ice therapy
- Over-the-counter pain relievers – acetaminophen or ibuprofen.
- Braces or compression wraps can help support the body and alleviate symptoms during healing and recovery.
- Exercises to improve posture
- Paying attention to form when lifting objects
- Stretching can help ease the pain.
Medication
Medications can be used in a variety of ways to help in the treatment of lower back and pelvic pain. If an infection is the cause, medications will be prescribed to remove the infection and resolve the symptoms, which can include:
- Antibiotics
- Antifungals
- Antivirals
Medications may also be prescribed to help manage pain symptoms and may include:
- Medication to relieve nerve pain
- Muscle relaxants
- Steroids
Physical Therapy
A physical therapist can help to correct problems with:
- Posture
- Decreased mobility
- Walking gait
- Strengthening
- A physical therapist will provide exercises to help increase and maintain strength, range of motion, and flexibility.
Pelvic Floor Therapy
- This is physical therapy that focuses on the muscles, ligaments, and connective tissues in the pelvis.
- It helps with pain, weakness, and dysfunction in the pelvic area.
- A treatment plan will be developed to help with strength and range of motion in the pelvic muscles.
Chiropractic Care
- Chiropractors offer spinal and hip adjustments to realign the joints of the spine.
- Adjustments have been shown to help reduce back and hip pain. (Valter Santilli, Ettore Beghi, Stefano Finucci. 2006)
Surgery
- Some more severe conditions could require surgery.
- Ovarian cysts, hernias, and other infections sometimes require surgery to remove infected or unhealthy tissue – ruptured ovarian cysts or appendicitis.
Recommended surgeries can include:
- A hernia repair.
- Hip replacement.
- Gallbladder removal to prevent recurring pancreatitis.
Prevention
Not all conditions and diseases cause lower back and pelvic pain. Symptoms can be prevented and reduced by adopting lifestyle changes. Prevention recommendations can include:
- Staying hydrated.
- Using proper bending and lifting techniques.
- Eating healthy foods.
- Regularly engaging in some form of physical activity – walking, swimming, yoga, cycling, or strength training.
- Maintaining a healthy weight.
Pregnancy and Sciatica
References
Richardson, W. S., Jones, D. G., Winters, J. C., & McQueen, M. A. (2009). The treatment of inguinal pain. Ochsner journal, 9(1), 11–13.
Kurosawa, D., Murakami, E., & Aizawa, T. (2017). Groin pain associated with sacroiliac joint dysfunction and lumbar disorders. Clinical neurology and neurosurgery, 161, 104–109. https://doi.org/10.1016/j.clineuro.2017.08.018
Johns Hopkins Medicine. Appendicitis.
Mount Sinai. Splenomegaly.
Santilli, V., Beghi, E., & Finucci, S. (2006). Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. The spine journal : official journal of the North American Spine Society, 6(2), 131–137. https://doi.org/10.1016/j.spinee.2005.08.001
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


