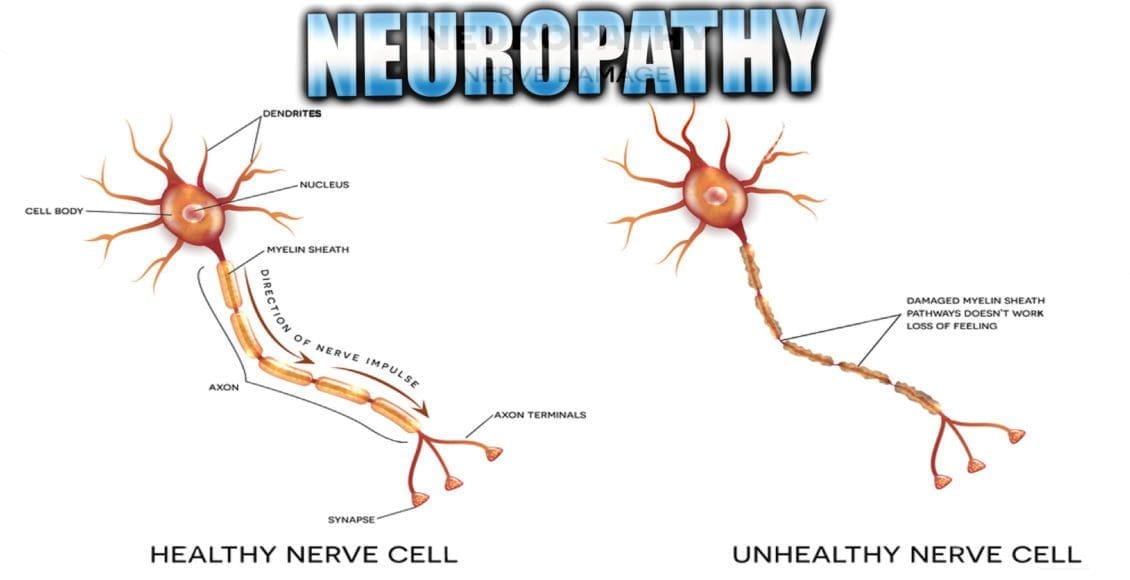
Neuropathy Presentation: El Paso, TX. Chiropractor, Dr. Alexander Jimenez presents an overview of neuropathy. These are the most common neuropathies to be seen in practice. Neuropathy is a medical term used to characterize damage or injury to the nerves, which refers to the peripheral nerves as opposed to the central nervous system. The complications which follow neuropathy depends largely on the type of nerves that are affected. According to Dr. Alex Jimenez, different neuropathies can cause numbness and tingling sensations, increased pain or the loss of ability to feel pain, muscle weakness along with twitching and cramps, even dizziness and/or loss of control over bladder function.
Table of Contents
Neuropathy
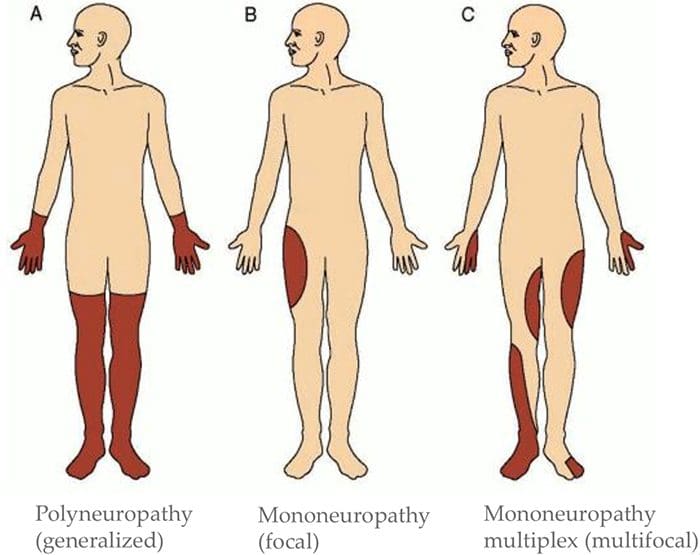
Three primary classifications based on location of symptoms:
- Mononeuropathy (focal)
- Mononeuropathy multiplex (multifocal)
- Polyneuropathy (generalized)
- Can involve CNS and/or PNS
- Can affect large and/or small diameter fibers
- Can affect both sensory and motor fibers
- Sometimes one more than the other, but often both
- May be permanent or reversible
*https://neupsykey.com/muscle-weakness-cramps-and-stiffness/
Assessment Of Neuropathy
Sensory Exam:
-
Determine What Sensory Modalities Are Involved
- If sensory disruption is limited to certain modalities, it implies CNS is involved
- If all sensation is affected in the area, implies PNS is involved
-
Determine Pattern Of Symptoms
- Mononeuropathy (focal)?
- Mononeuropathy multiplex (multifocal)?
- Polyneuropathy (generalized)?
-
Motor Exam
- Determine if there is change to muscle strength
- Determine if there is a change in muscle tone
- Determine which muscles are affected
- Determine if there has been a change in reflexes
- This information can help determine the level(s) of involvement
-
Check For Autonomic Signs
- Auscultate heart
- Palpate palms
- Auscultate abdomen
- Assess autonomic history
- For example, is patient complaining about sweating more on one side than another? Complaining of stress levels?
- Suggest ANS involvement
Exams: Merck Manual Professional Version
How To Test Reflexes
How To Do The Sensory Exam
How To Do The Motor Examination
Classification Of Nerve Injuries Resulting In Neuropathy
- Neurapraxia – This is a transient episode of motor paralysis with little or no sensory or autonomic dysfunction; no disruption of the nerve or its sheath occurs; with removal of the compressing force, recovery should be complete
- Axonotmesis – This is a more severe nerve injury, in which the axon is disrupted but the Schwann sheath is maintained; motor, sensory, and autonomic paralysis results; recovery can occur if the compressing force is removed in a timely fashion and if the axon regenerates
- Neurotmesis – This is the most serious injury, in which both the nerve and its sheath are disrupted; although recovery may occur, it is always incomplete, secondary to loss of nerve continuity
Brachial Plexopathies
- Erb’s Palsy
- Klumke’s Palsy
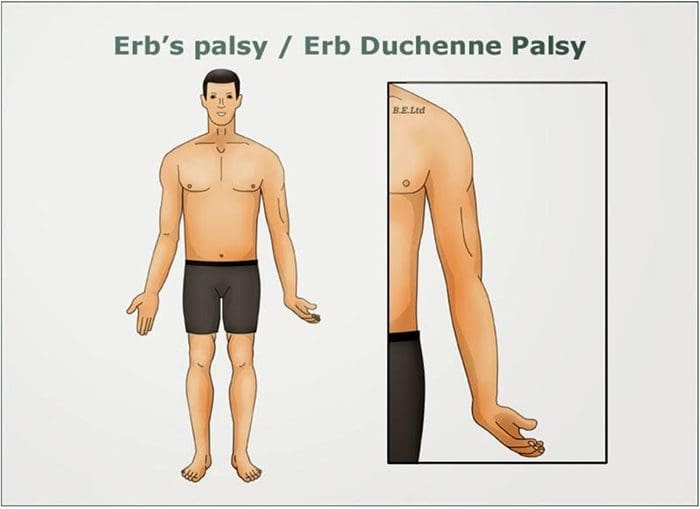
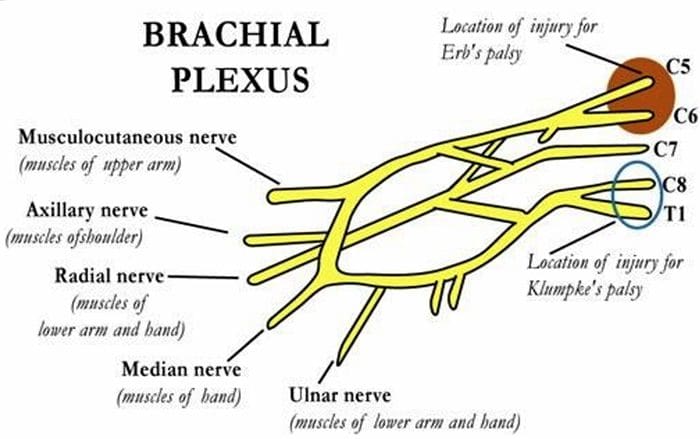 Erb’s Palsy
Erb’s Palsy
- AKA Erb–Duchenne palsy or Waiter’s tip palsy
- Most common mechanism of injury in adults is a patient who fall forward while holding onto something behind them
- Can also happen to an infant during childbirth ? Results from damage to C5-6 nerve roots in the brachial plexus
- Dermatomal distribution of sensory disruption
- Weakness or paralysis in deltoid, biceps, and brachialis muscles resulting in “waiter’s tip” position
 Klumke’s Palsy
Klumke’s Palsy
- AKA Dejerine–Klumpke palsy
- Happens to infants during childbirth if arm is pulled overhead
- Can also happen to adults with overhead traction injuries
- Results from damage to C8-T1 nerve roots in the brachial plexus
- Dermatomal distribution of sensory disruption
- Weakness or paralysis in wrist flexors and pronators as well as muscles of the hand
- May produce Horner’s syndrome due to T1 involvement
- Results in a “claw hand” appearance
- Forearm supinated with wrist hyperextended, with finger flexion
 Entrapment Neuropathies
Entrapment Neuropathies
- Thoracic Outlet Syndromes
- Median Nerve Entrapment
- Pronator Teres syndrome
- Carpal Tunnel syndrome
- Ulnar Nerve Entrapment
- Cubital Tunnel syndrome
- Tunnel of Guyon syndrome
- Radial Nerve Entrapment
- Spiral Groove Entrapment
- Supinator Syndrome
- Posterior Interosseous Syndrome (Radial Tunnel Syndrome)
- Sciatic Nerve Entrapment
- Piriformis syndrome
- Fibular head entrapment
- Tarsal tunnel syndrome
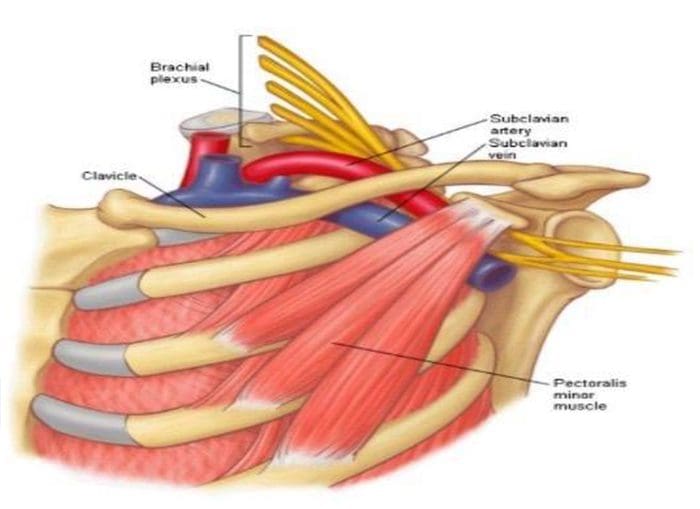
Thoracic Outlet Syndromes

-
Neurogenic thoracic outlet syndrome
- Compression of the brachial plexus
-
Vascular thoracic outlet syndrome
- Veins (venous thoracic outlet syndrome) or arteries (arterial thoracic outlet syndrome) are compressed
-
Nonspecific-type thoracic outlet syndrome
- Worsens with activity
- Idiopathic
Causes
- Cervical rib
- Subclavius muscle tension
- Postural – excessive thoracic kyphosis
- Trauma
- Repetitive activity
- Obesity
- Pregnancy
Tests
- Adsons test
- Allen maneuver
- Costoclavicular maneuver
- Halstead maneuver
- Reverse bakody maneuver
- Roos test
- Shoulder compression test
- Wright test
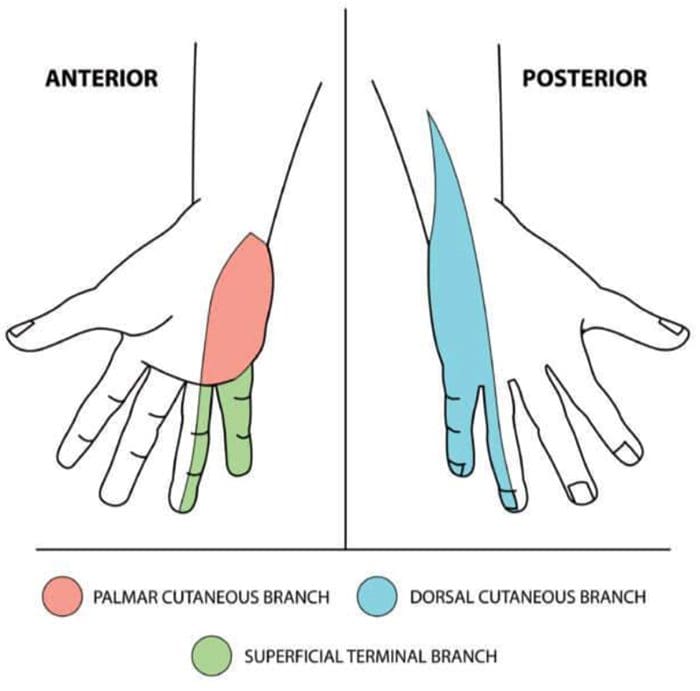
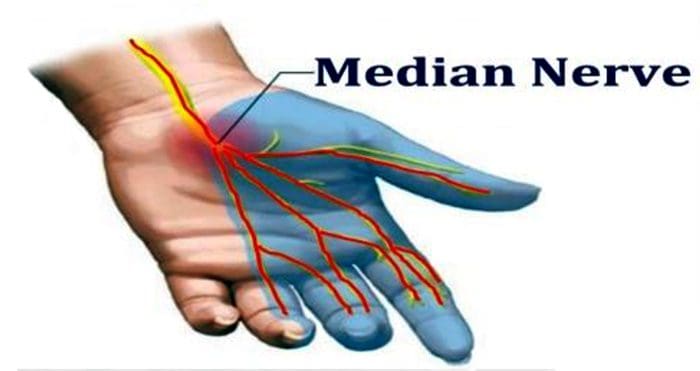
Median Nerve Entrapment
- Sensory disruption in the lateral portion (3.5 fingers) of the palmar aspect of the hand, and dorsal finger tips of the same fingers
- Motor fibers affected in forearm if applicable, muscles of the thenar eminence
- Abductor pollicis brevis
- Opponens pollicis
- Flexor pollicis brevis
 Median N. Pronator Teres Syndrome
Median N. Pronator Teres Syndrome
Etiology
- Compression of the median nerve at the elbow
Causes
- Repetitive movement
- Pronator teres muscle inflammation
- Thickened bicipital aponeurosis
Findings
- Tenderness with palpation of the pronator teres muscle
- Pain with resisted pronation of the arm
- Flexor pollicus longus and flexor digitorum profundus involvement
- Otherwise may appear similar to carpal tunnel syndrome in symptoms, but without positive wrist orthopedics
Median N. Carpal Tunnel Syndrome
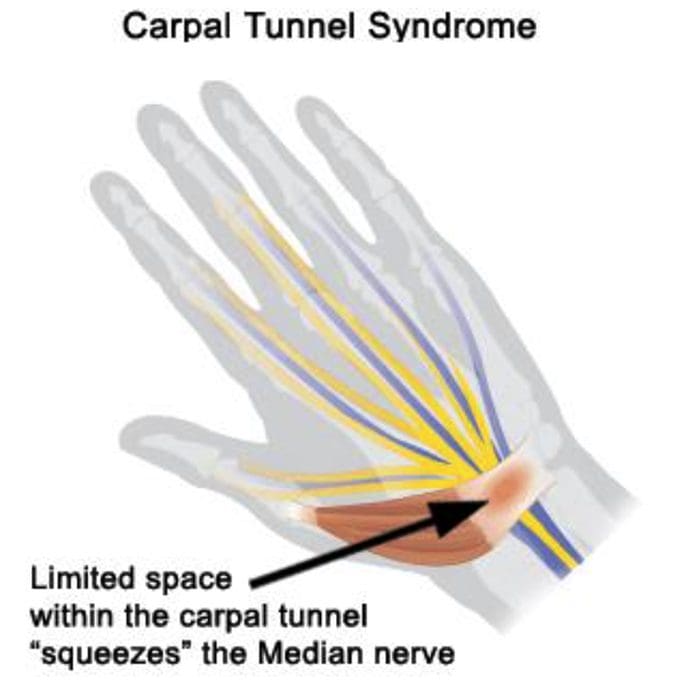
Etiology
- Compression of the median nerve at the wrist
Causes
- Repetitive motions
- Hypothyroidism
- Obesity
- Rheumatoid Arthritis
- Diabetes
- Pregnancy
Orthopedic Tests
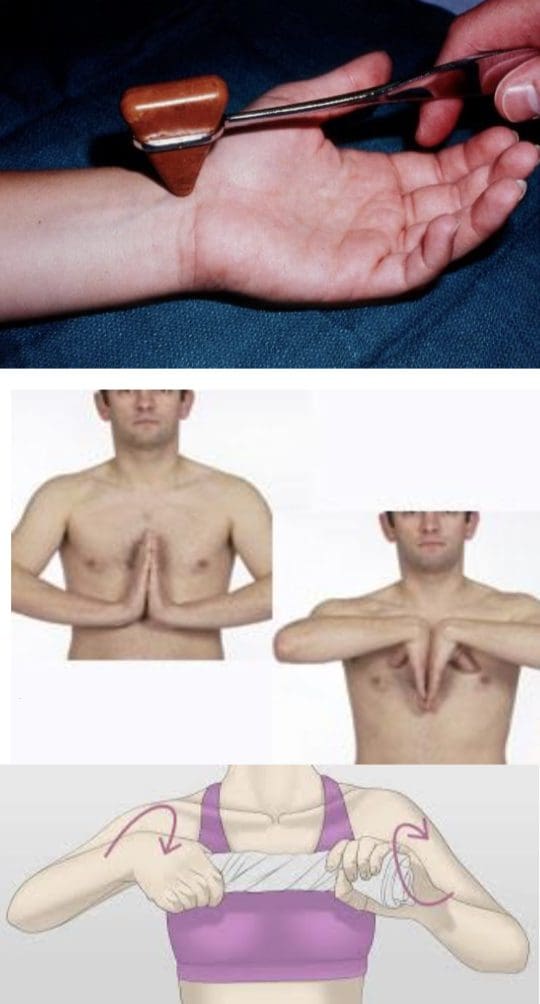 Tinel’s Sign
Tinel’s Sign
- Positive if tapping over the median nerve reproduces/exacerbates symptoms
Phalen’s Maneuver/Prayer Sign
- Hands together with wrists flexed
- Repeat in reverse with wrists extended
- Hold each for at least 60 seconds
- Positive if tests reproduce/exacerbate symptoms
Wringing Test
- Wringing a towel produces paresthesia
Ulnar Nerve Entrapment
- Sensory disruption in the medial two digits of the palmar & dorsal aspects of the hand
- Motor fibers affected in hand, all fingers besides the thumb weakened general hand weakness
Ulnar N. Cubital Tunnel Syndrome
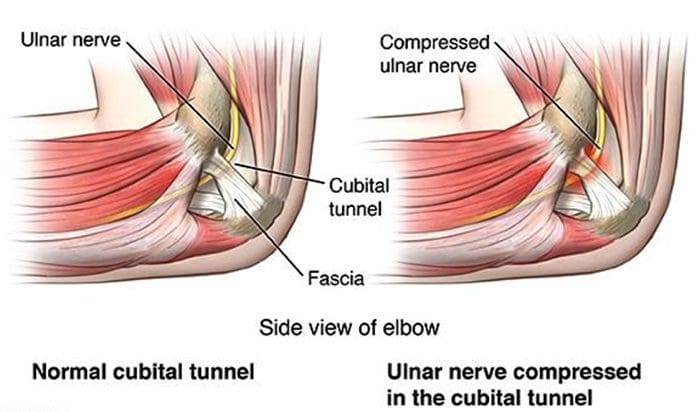 Etiology
Etiology
- Compression of the ulnar nerve at the elbow
Causes
- Repetitive motions
- Hypothyroidism
- Obesity
- Diabetes
- Trauma to the cubital tunnel
- Prolonged sitting with pressure on bent elbow
Ulnar N. Tunnel Of Guyon Syndrome
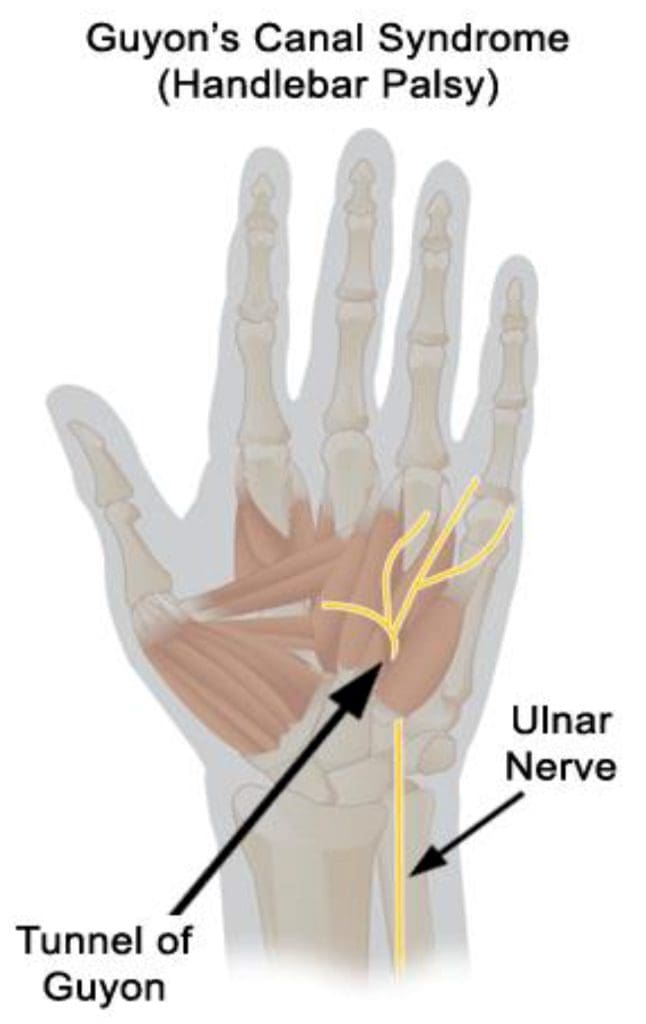
Etiology
- Compression of the ulnar nerve at the wrist
Causes
Repetitive motions
- Long term crutch use
- Break of the hamate
- Ganglion cyst
- Hypothyroidism
- Obesity
- RheumatoidArthritis
- Diabetes
Orthopedic Tests
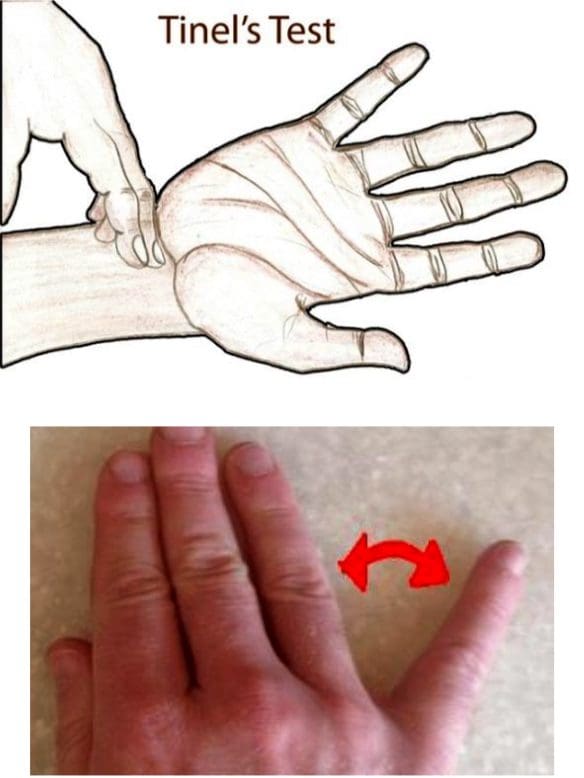
Tinel’s Sign
- Present if test over the ulnar nerve at the wrist elicits symptoms
Wartenberg Sign
- 5th digit abducts when patient performs hard grip strength test or attempts to squeeze fingers together
- Reduced two-point discrimination in the hand
Radial Nerve Entrapment
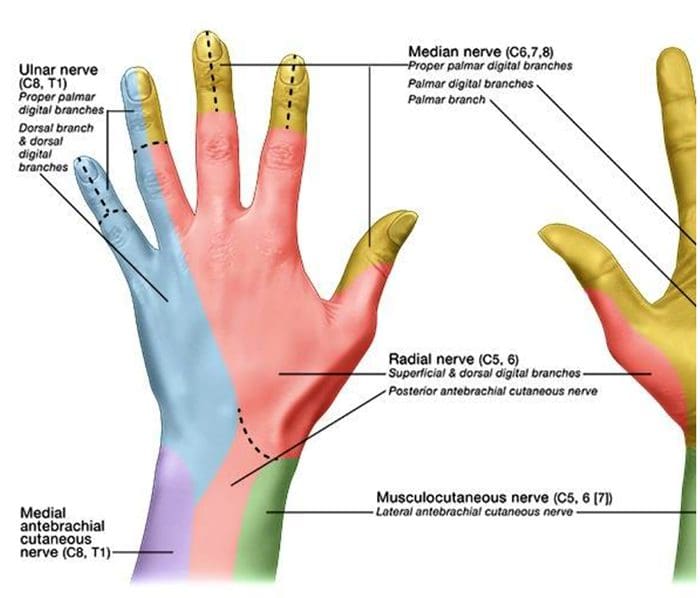
- Sensory disruption in the lateral 3.5 digits of the dorsal aspect of the hand
- Motor fibers affected in posterior arm and extensor compartment of the forearm
- Wrist drop may be seen
Spiral Groove Entrapment
- All radial nerve innervated muscles below entrapment are affected
- “Saturday night palsy” (from sleeping on own arm)
- Brachioradialis & triceps reflexes both diminished
Supinator Syndrome
- Compression at the arcade of Frohse
- No change in reflexes
Posterior Interosseous Syndrome (Radial Tunnel Syndrome)
- No change in reflexes
By Rachel Klein, ND, DC, DACNB
National University of Health Sciences Master of Science (MS) – Advanced Clinical Practice (ACP) MS ACP 551: Clinical Neurology © 2018
Sources
Blumenfeld, Hal. Neuroanatomy through Clinical Cases. Sinauer, 2002.
Evans, Ronald C. Illustrated Orthopedic Physical Assessment. Mosby/Elsevier, 2009.
“Radial Nerve Entrapment: Background, Anatomy, Pathophysiology.” Medscape, 25 Oct. 2017, emedicine.medscape.com/article/1244110- overview#a8.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to Chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Masters in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card