Table of Contents
Introduction
Everyone around the world has dealt with pain that makes them feel uncomfortable and has them place their hands on the location where the pain is originating in their bodies. Many factors can become issues in the body, like a poor, unhealthy lifestyle that causes problems in the gut system and develop painful symptoms that affect the intestines. Stressful events that cause headaches that affect the neck and upper back muscles or gut issues that cause discomfort in the abdominal and back region. All these issues are known as referred pain, where a person feels pain in one part of their body, but it is caused by a different source of pain in a different location. An example would be an individual with back pain, but the pain is originating in their abdominal organs. Today’s article looks at various issues that mask low back pain in the body, how organ issues mimic low back pain, and how to alleviate these issues affecting the body. We refer patients to certified providers specializing in gastroenterology and chiropractic treatments that help those with issues that affect their back and gut system. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Different Issues Masking Low Back Pain
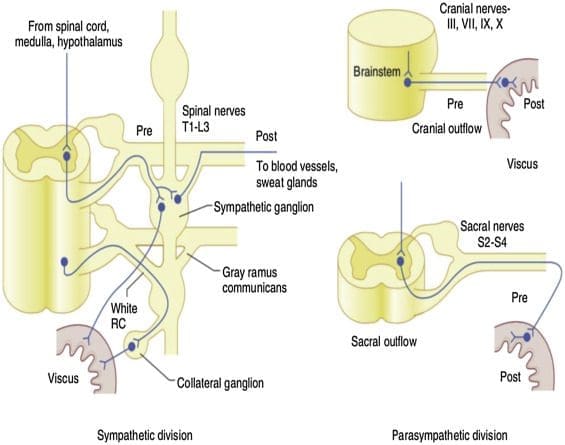
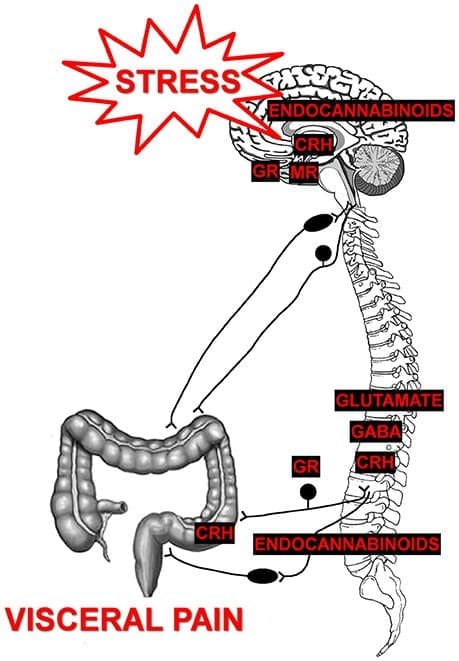
Have you experienced discomfort in your abdominal region causing pain in your lower back? How about pelvic issues that are causing bowel discomfort? Or constipation issues that are compressing the nerves in your lower back? These signs and symptoms correlate to visceral-somatic pain, defined as poorly localized pain characterized by irritated internal organs that cause muscle hypersensitivity from the same nerve. So what does this mean for a person experiencing back issues affecting their quality of life? Well, this might be an indication of the individual that might be suffering from gastrointestinal problems that are correlating to low back pain. Studies reveal any disturbances causing musculoskeletal or gastrointestinal complaints that could induce referred pain through the sympathetic nervous system. An example will be if the body suffers from infections from the kidneys that are associated with low back pain.
So how would the kidneys be associated with low back pain? What is the correlation? For example, a person is constantly eating foods with either a high salt content or a high protein in their system. These high food contents begin to form kidney stones in one or both organs, thus causing a sharp pain that triggers low back pain. As the kidney stones pass through the urinary tract, it administrates radiating pain to the body’s lower abdominal and pelvic region. Another example of issues that can mask low back is constipation in the abdominal area associated with pelvic dysfunction. How does this correlate to the lower back? Think of your abdominal organs overlapped by risk profiles associated with gut disorders. Signs like hypothyroidism, SIBO, celiac disease, or IBS can increase the risk associated with pelvic floor dysfunction, which causes bloating and constipation to the abdominal organs. These issues are co-morbidities to IBS as studies reveal that the pelvic floor and abdominal muscles are co-activated to increase spine stability and intra-abdominal pressure. Now it may seem not a bad thing to the body unless the individual is constantly standing for an extended period or is obese, thus becoming a mediator for the host to suffer from low back pain while being associated with pelvic dysfunction.
Organ Issues Mimicking Low Back Pain- Video
Have you been feeling muscle tenderness in the lower extremities of your body? How about gut issues that are associated with low back pain? Or are you feeling bowel dysfunction in your pelvic region? All these issues correlate to viscerosomatic pain, where the infected organ is causing issues to the muscle in a different location. The video above explains how various organ issues can mimic spinal and back pain in the body. One of the examples that the video explains is how kidney infections are associated with back pain. Studies reveal that visceral pain originating from the upper urinary tract coincidently correlates with the characteristics of referred pain and changes in the somatic tissues of the body.
Alleviating Issues Affecting The Body
Say an individual is suffering from low back pain issues; as they get their mandatory examination, they explain to their physician about their low back pain and what is happening. Once the suffering individual is situated, the physician begins to look over the body where the pain is located, either by physical examination or through the intake form they are looking over. So what does this implicates in the body? Well, studies have revealed that systemic pathologies of the visceral organs can mimic or mask musculoskeletal pain. An example would be someone who is experiencing gastrointestinal issues in their gut, and it’s triggering muscle spasms in the back. This causes the nerve roots to be hypersensitive to the visceral organs and increases the risk associated with low back pain.
Conclusion
Dealing with pain is no joke, primarily when the pain is located in a different body region. Sometimes the pain can be an organ issue that mimics muscle pain in the back. This is known as viscero-somatic pain, defined where infected organs are either mimicking or triggering muscle issues in different body locations. This causation is usually due to various factors like unhealthy lifestyle habits affecting the visceral organs and affecting the muscles that correspond to the organs, like IBS issues affecting the lower back. Available treatments are there to figure out what problems affect the body and provide a better understanding to alleviate them.
References
Basso, Francesca Lo, et al. “Manual Treatment for Kidney Mobility and Symptoms in Women with Nonspecific Low Back Pain and Urinary Infections.” De Gruyter, De Gruyter, 1 May 2021, https://www.degruyter.com/document/doi/10.1515/jom-2020-0288/html.
Bussey, Melanie Dawn, et al. “Is Pelvic Floor Dysfunction Associated with Development of Transient Low Back Pain during Prolonged Standing? A Protocol.” Clinical Medicine Insights. Women’s Health, SAGE Publications, 27 May 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6537301/.
J;, Stowell T;Cioffredi W;Greiner A;Cleland. “Abdominal Differential Diagnosis in a Patient Referred to a Physical Therapy Clinic for Low Back Pain.” The Journal of Orthopaedic and Sports Physical Therapy, U.S. National Library of Medicine, Nov. 2005, https://pubmed.ncbi.nlm.nih.gov/16355918/.
Lacy, Brian E, et al. “Management of Chronic Abdominal Distension and Bloating.” Clinical Gastroenterology and Hepatology : the Official Clinical Practice Journal of the American Gastroenterological Association, 1 Apr. 2020, https://www.cghjournal.org/article/S1542-3565(20)30433-X/fulltext.
PJ;, Pedersen KV;Drewes AM;Frimodt-Møller PC;Osther. “Visceral Pain Originating from the Upper Urinary Tract.” Urological Research, U.S. National Library of Medicine, 16 May 2010, https://pubmed.ncbi.nlm.nih.gov/20473661/.
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card