Table of Contents
Bone Neoplasms Tumor-Like Conditions
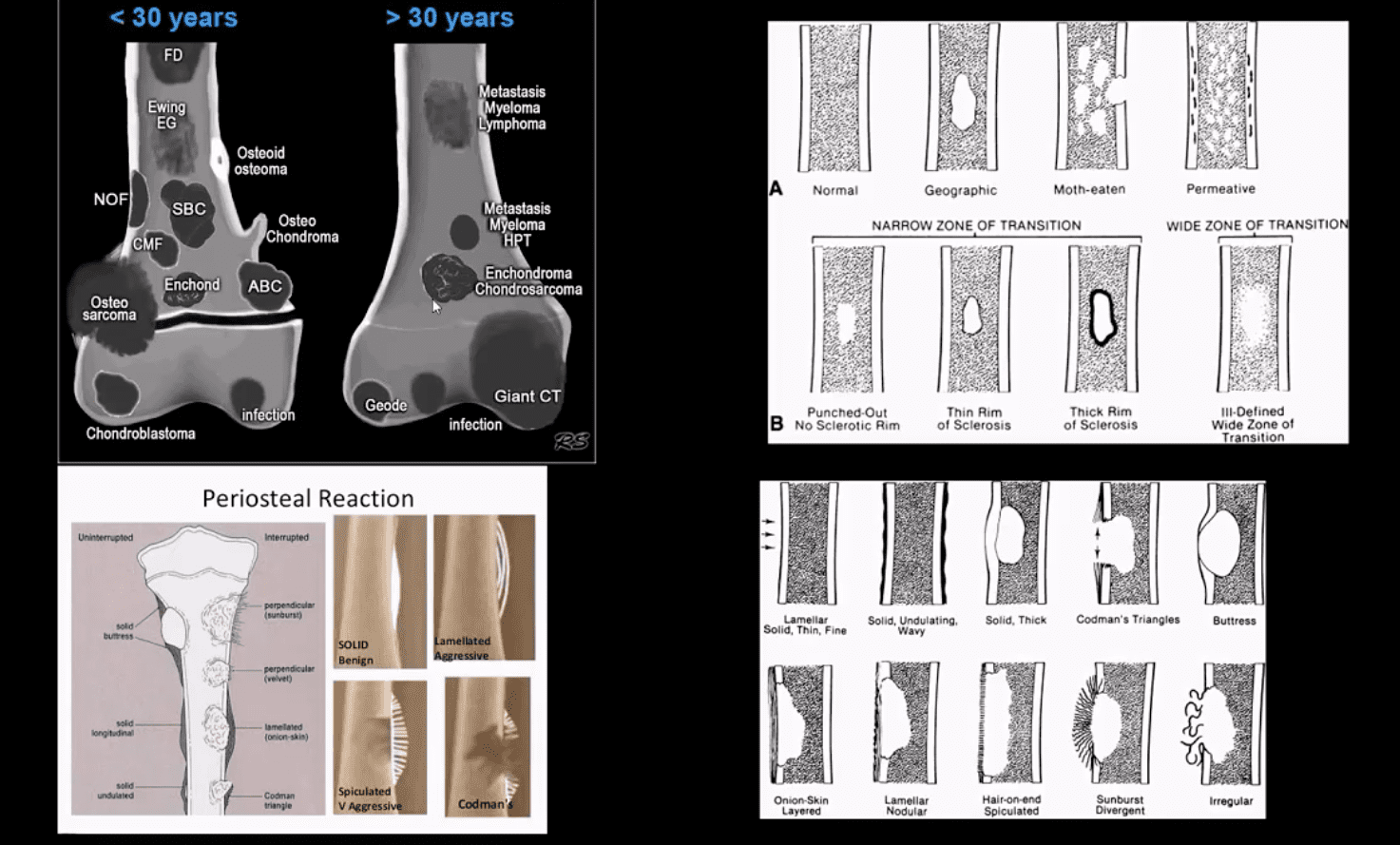
- Bone neoplasms and tumor-like conditions affecting the knee can be benign or malignant. Age at Dx is crucial for DDx
- In patients <40: Benign bone neoplasms: Osteochondroma, Enchondroma are relatively frequent
- Fibrous cortical defect (FCD) & Non-ossifying fibroma (NOF) are particularly frequent in children
- Giant cell tumor (GCT) is the m/c benign neoplasm of the knee in patients between 20-40 years of age
- Malignant bone neoplasms in <40: m/c Osteosarcoma and 2nd m/c Ewing sarcoma
- In patients >40: malignant neoplasms: m/c are secondaries d/t bone metastasis. Primary bone malignancy: the m/c
- Multiple Myeloma (MM). Less frequently:
2nd peak of Osteosarcoma (post-radiation or Paget’s), Fibrosarcoma or Malignant FibrousHisteocytoma (MFH) of bone. - Clinically: knee pain, pathological fracture
- Some tumor-like conditions like FCD/Non-ossifying fibroma are asymptomatic and may regress spontaneously.
Occasionally NOF may present with pathologic fracture. N.B. any knee/bone pain in a child/adolescents should be treated with clinical suspicion and properly investigated. - Imaging: 1st step: radiography
- MRI with T1+C is crucial for lesion characterization/regional extent, staging and pre-operative planning. CT may help with pathologic Fxs detection. If malignant bone neoplasms considered, CXR/CT, PET-CT to investigate metastatic spread and staging are important
Imaging Approach Bone Neoplasms
- Approach to imaging Dx of bone neoplasms includes: age, bone location (epiphysis vs metaphysis vs diaphysis), zone of transition surrounding the lesion, periosteal response, type of matrix, permeating or moth-eaten destruction vs. sclerotic, ground-glass, osteoid, cartilaginous matrix, soft tissue invasion etc.
- Key x-radiography features to DDx benign vs malignant bone neoplasm:
- Zone of transition: lesion is geographic with narrow zone of transition vs ill-defined wide zone of transition suggesting aggressive bone resorption
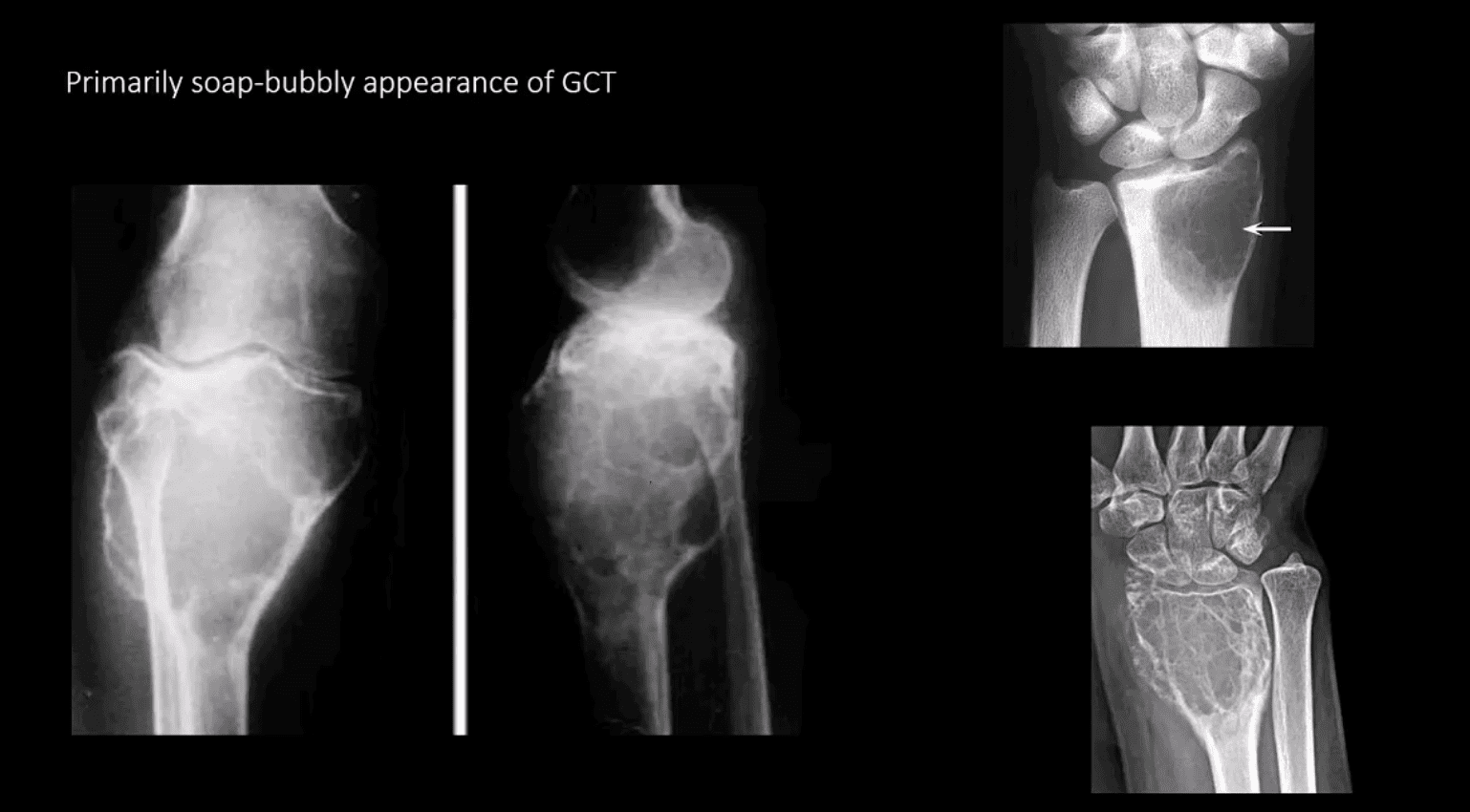
- What type of bone destruction occurred: soap-bubbly appearance vs. osteolytic vs. osteosclerotic changes
- Is there a round-glass matrix? Is there a well-defined rim of sclerotic border with septations potentially suggesting slow growth and encapsulation like most benign processes.
- Periosteal proliferation: solid vs. aggressive spiculated/sunburst/hair-on-end with local soft tissue invasion and Codman triangle (study next slide)
FCD & NOF

- FCD & NOF or more appropriately Fibroxanthoma of the bone are benign bone processes that m/c seen in children. DDx based on the size with FCD presenting as <3-cm and NOF >3cm lesion composed of
fibrous heterogeneous matrix. FCD are asymptomatic and may regress in many cases. Some may progress to NOF. Location: identified in the knee region aseccentric cortical based lesion. - FCD must be DDx from an avulsive irregularity d/t repeated stress along Linea
aspera by extensors muscles - Dx: radiography
- Management: leave-me-alone lesion. Occasionally NOF may progress and lead to pathologic fracture requiring
orthopedic consult
Osteochondroma
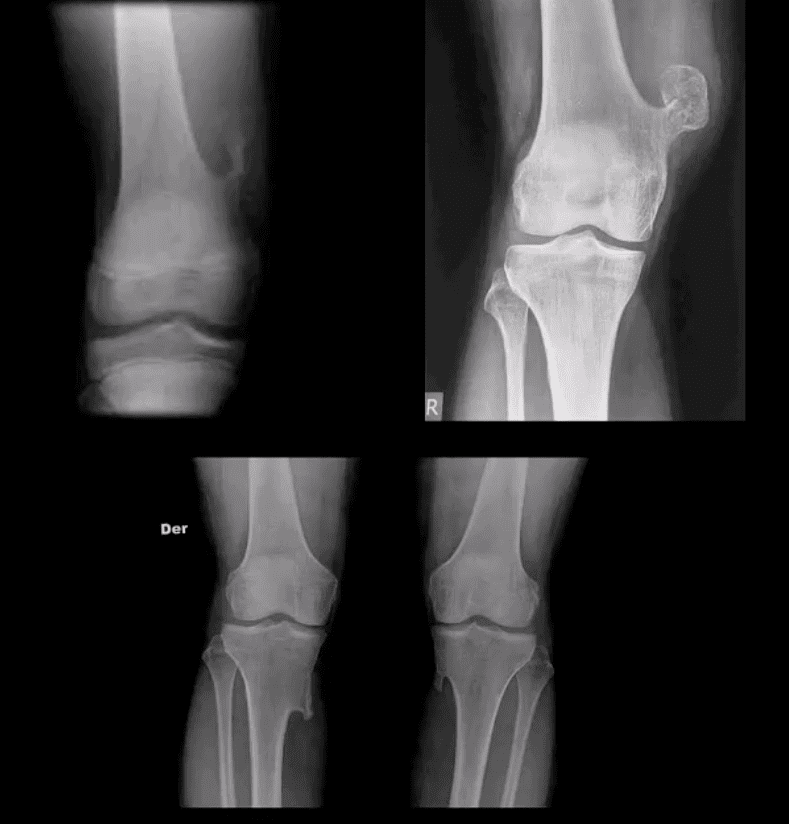
- Osteochondroma: m/c benign bone neoplasm.
Knee is the m/c location. Contains all bone elements withcartilaginous cap. Presented as pedunculated or sessile bone exostosis pointing away from the joint. - 1% malignant degeneration to chondrosarcoma if solitary lesion and 10-15% in cases of HME
- Other complications: fracture (top left image) pseudoaneurysm of
Popliteal artery, adventitious bursa formation - Hereditary Multiple Exostosis (HME)– autosomal dominant process. Presents with multiple osteochondromas (sessile-type dominates). May lead to limb deformities (Madelung deformity, coxa valga) reactive ST pressure, malignant degeneration
- Dx: radiography, MRI helps to Dx malignant degeneration to chondrosarcoma by changes in size and activity of cartilaginous cap (>2-cm in adults may manifest malignant degeneration). MRI will also help with Dx of regional complications
HME & Knee Pain
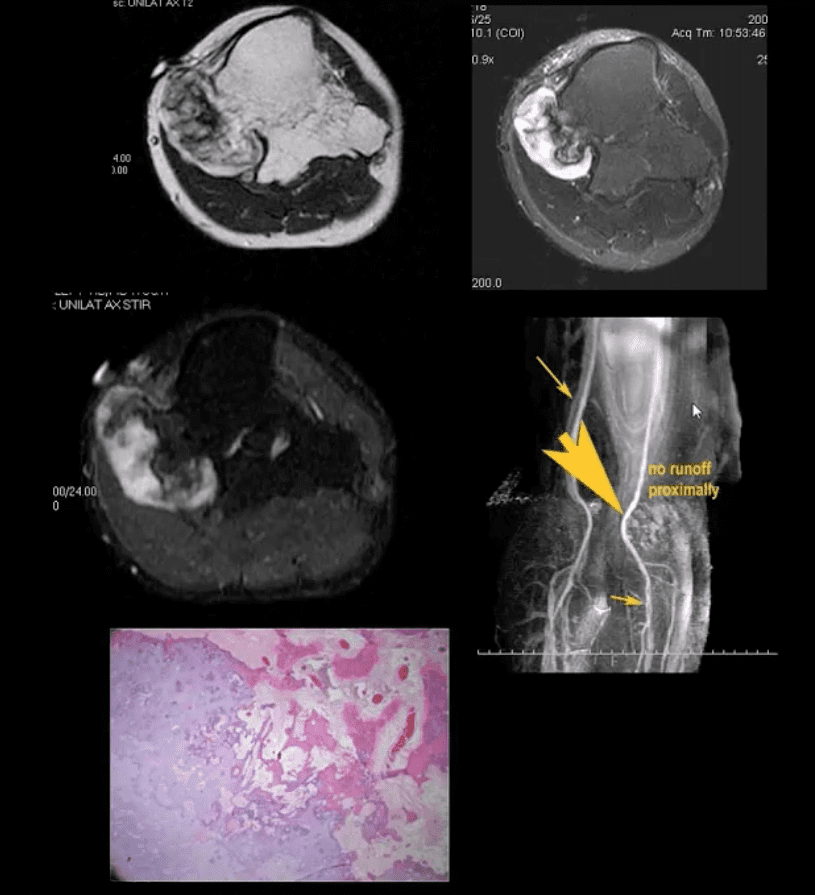
37-y.o male with HME and knee pain. Axial T1, T2 and STIR MRI slices at
Giant Cell Tumor (GCT) aka Osteoclastoma

- GCT- is a relatively common primary benign bone neoplasm. Age 25-40. M>F slightly.
- M/C location: Distal femur>proximal tibia>distal radius>sacrum
- GCT is the M/C benign sacral tumor. In 50
% cases GCT occurs about the knee. - GCT is histologically benign but lung
mets may develop esp. if in distal radius and hands, often termed Malignant GCT - <1% unresponsive/recurring GCTs may undergo malignant transformation to
high grade bone sarcoma - Pathology: histologically composed of osteoclasts-multinucleated giant cells with stromal cells derived from precursors
monocytemacrophage type. Produces cytokines and osteolytic enzymes. GCT may contain blood and associated with secondary Aneurysmal Bone Cyst (ABC) - Clinically: knee pain unresponsive to conservative care. Pathologic Fx may occur
- Imaging: always begins with radiography followed by MRI and surgical biopsy that are crucial to Dx.
- Rx: operative with curettage and cementing,
surgical appliance may be used if pathological fx present and cortical breach. In more severe cases other options available
Radiologic Pathologic Dx
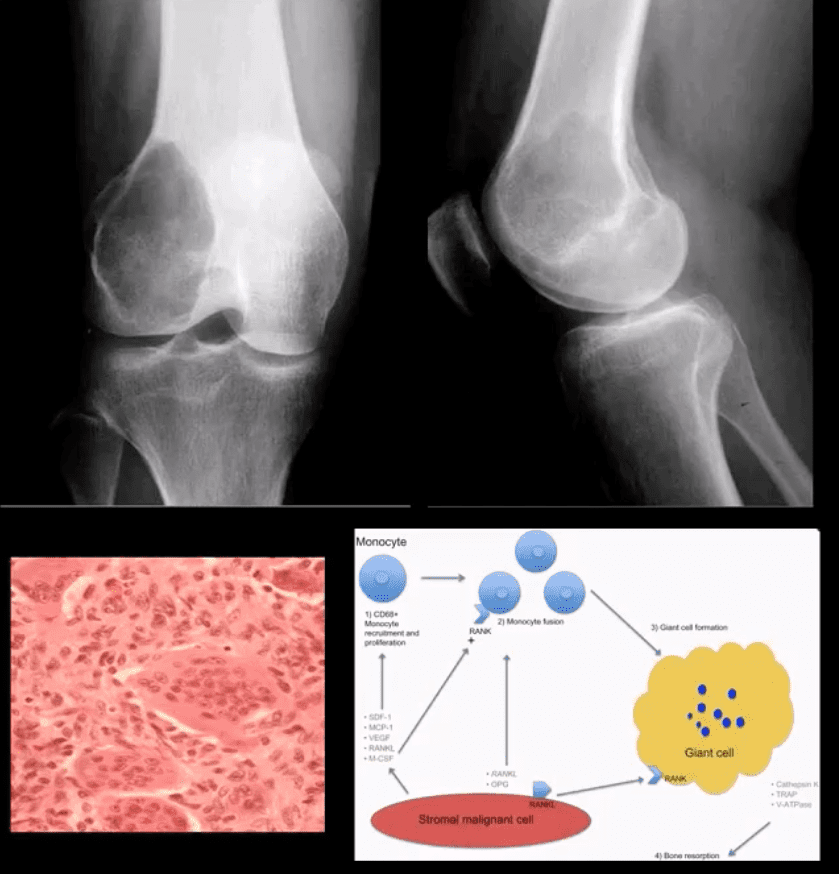
- Radiologic-pathologic Dx: osteolytic and/or soap-bubbly lesion typically involving metaphysis and into epiphysis (classic key feature) with subarticular extension. Zone of transition is typically narrow but occasionally in aggressive lesions wide zone of transition may be seen.
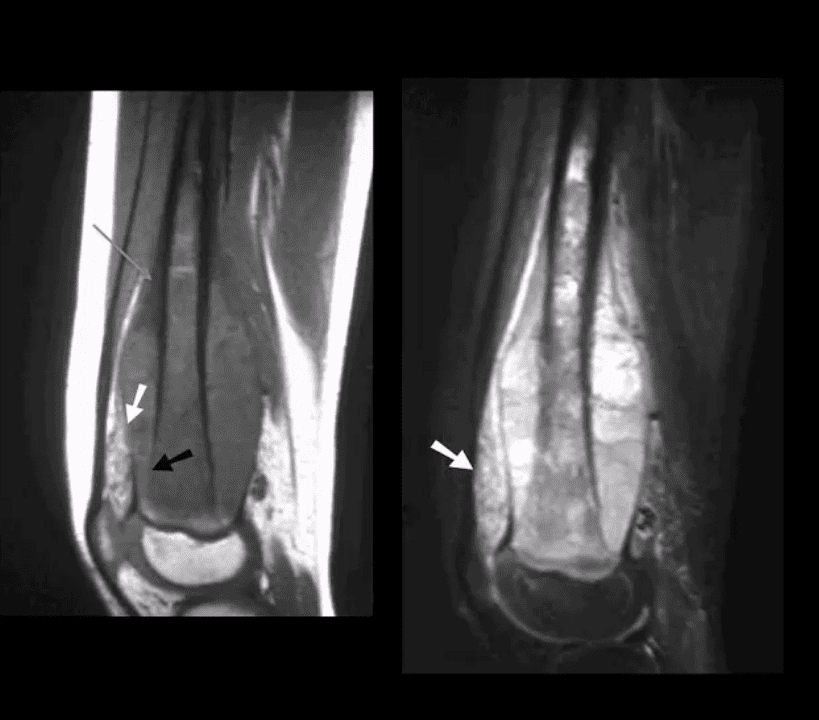
- MRI: low T1, highT2/STIR, characteristic fluid-fluid levels noted that are present in GCT and ABC. Histology is crucial to Dx.
- DDx: ABC, Brown cell tumor of HPT (osteoclastoma),
Telangectatic Osteosarcoma - Radiological rule: if
physeal growth plate is present Dx of GCT is taken off the list infavour of chondroblastoma and vice versa.
Primarily Soap-Bubbly Appearance of GCT
Coronal, Fat-Sat Sagittal & Axial MRI Slices of GCT
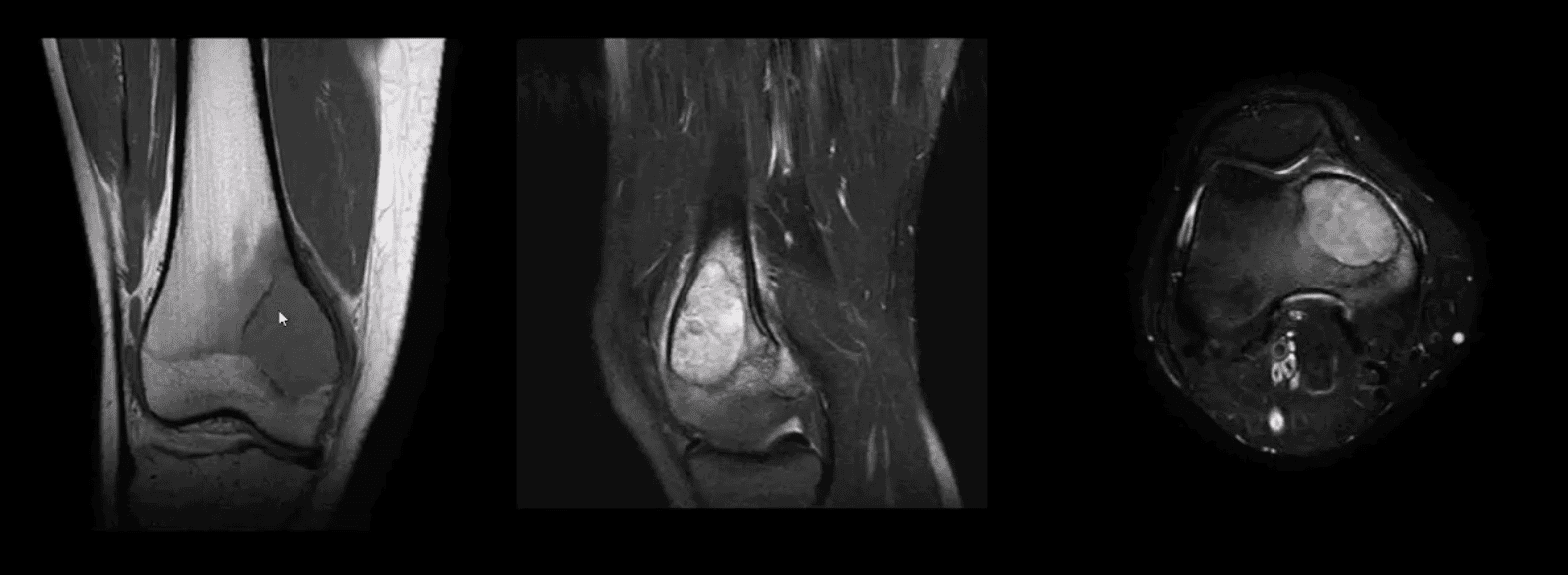
- T1 coronal, T2 fat-sat sagittal and T2 axial MRI slices of GCT. Typically: low T1, highT2/STIR and fluid-fluid levels
Characteristic MRI Appearance of GCT
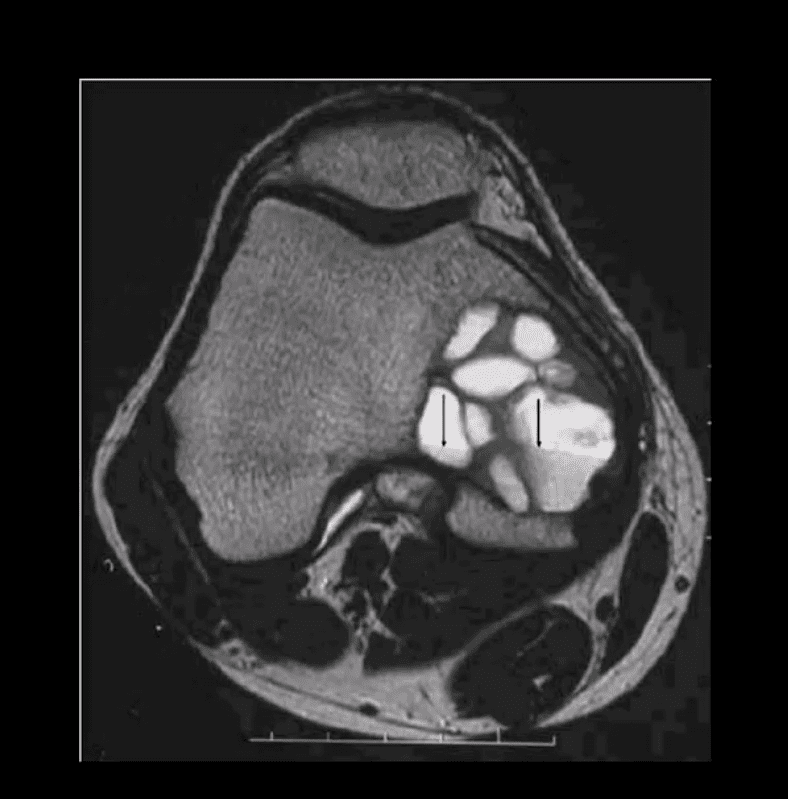
- Fluid-fluid levels d/t different composition of blood degradation products
- Important DDx: ABC
Malignant Neoplasms About the Knee
- In children and very young
adults m/c primary malignant neoplasm is central aka intramedullary (osteogenic) osteosarcoma (OSA). Second peak of OS: >70 y.o d/t Paget’s (1%) and/orpostradiation OSA. Knee is the m/c location of OSA (distal femur, prox. Tibia)2nd m/c malignant pediatric primary is Ewing sarcoma.- In adults >40 y.o. the m/c primary is Multiple Myeloma (MM) or Solitary Plasmacytoma
- Overall m/c bone neoplasms in adults d/t bone
mets from lung, breast, prostate, renal cell, thyroid (discussed) - Dx: clinical and radiological with surgical biopsy
- Imaging is crucial to Dx. 1st step x-radiography. MRI+ gad C is crucial
- CT scanning occasionally helps to evaluate pathological fracture
Central (Intramedullary) Osteosarcoma (OSA)

- m/c age: 10-20. m/c location: knee, males>females. Increased risk in some
- congenital syndromes and mutation of the retinoblastoma gene: Rothmund-Thompson AR syndrome.
- Early Dx is important d/t 10-20% present with Lung
mets at Dx. Prognosis depends on stages. Early stages with local bone invasion and no - mets 76% of survival.
- Rx: limb salvage procedures preferred with 8-12 weeks of chemo, amputation if encased neurovascular tissue, path Fx etc.
- Imaging: radiography and MRI.
- Clinically: bone pain,
inc . Alkaline Phosphatase - Chest CT if lung
mets considered
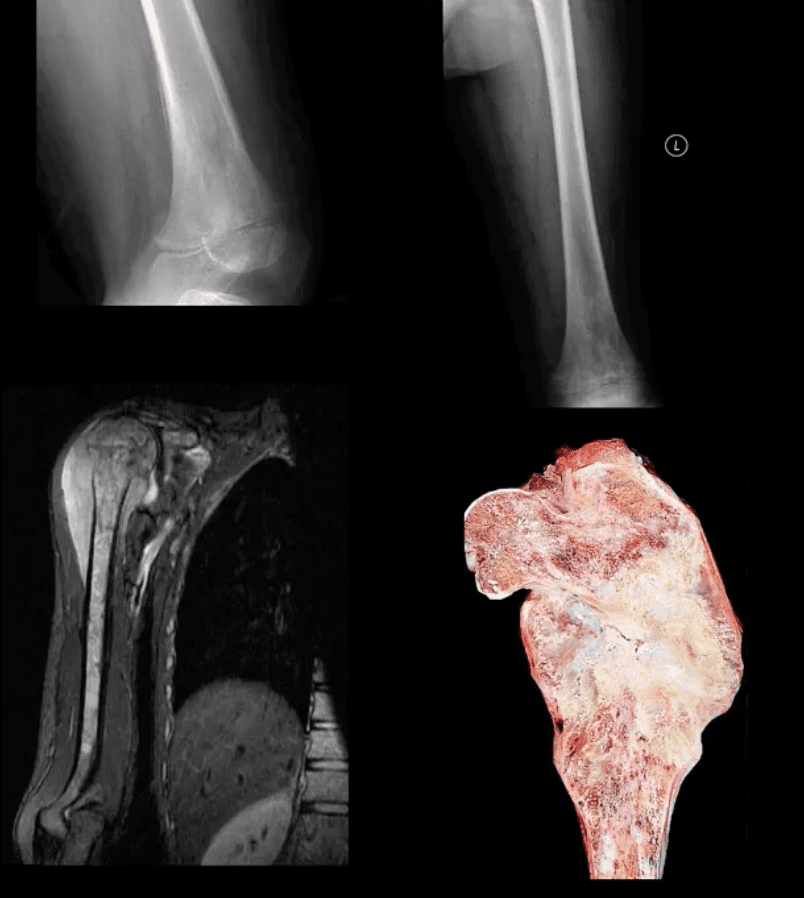
Classic Rad Features of OSA
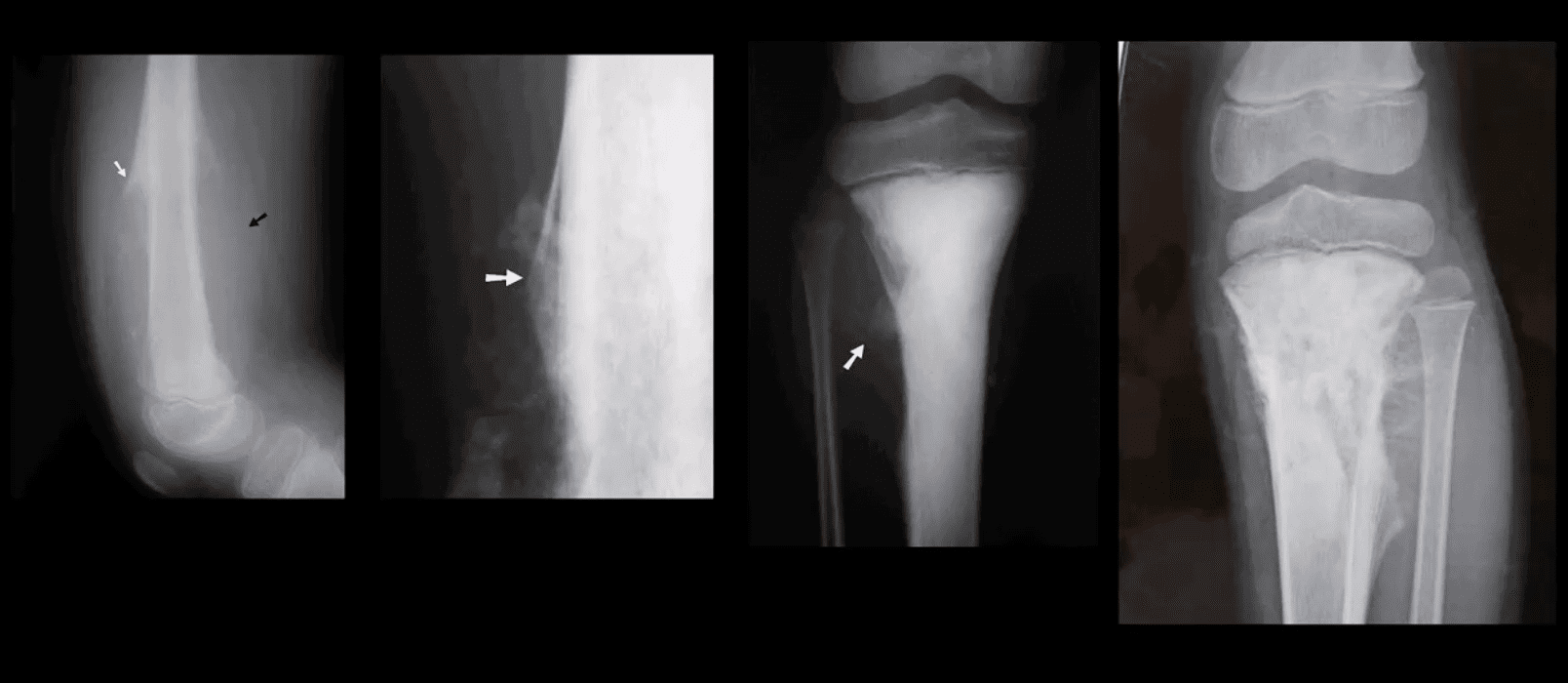
- Osteoid forming sclerotic mass with aggressive hair-on-end/speculated/sun-burst periosteal reaction, Codman’s trangle and soft tissue invasion. Order MRI for staging and extent. Chest CT is crucial for Lung Mets dx.
MRI is Crucial for Dx/Staging
- Note: sagittal T1 (left) and STIR (right) MR slices: large mass extending from distal femoral metaphysis to remaining shaft. Low signal on T1 and high on STIR d/t marrow invasion with edema,hemorrhaging and tumor invasion. Local ST invasion
seen (white arrows). Periosteal lifting and Codman’s triangle (green arrow) are additional signs of aggressive neoplasm. - Note an interesting feature that the epiphysis is spared d/t physeal plate serving temporarily as an additional barrier to the
tumour spread.
Ewing Sarcoma
Ewing sarcoma: age: 2-20, uncommon in black patients. 2nd m/c highly malignant bone neoplasm in children that typically arises from
Key Rad Dx: aggressive moth-eaten/permeative lucent lesions in the shaft of long bones with large soft tissue invasion/typical onion skin
periostitis. May produce
May affect flat bones. May appear as sclerotic in 33%. Early lung
Poor prognosis if delayed Dx. Imaging steps: 1st step x-rad, MRI is v. important followed by
Rx: combined rad-chemo, operative.
M/C Malignant Knee Neoplasms in Adults
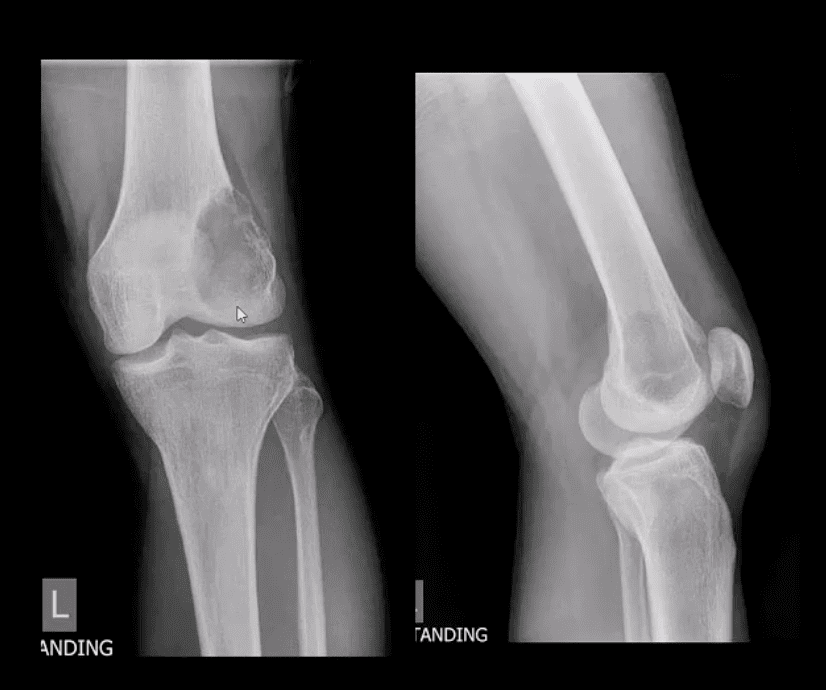
- 66-y.o. male with knee pain
- Note aggressive expansile osteolytic lesion in the distal femur metaphysis into epiphysis. No periosteal reaction present. Following further work up with abdominal and chest CT scanning, Dx of Renal cell carcinoma was established
- Distal
mets into lower extremity are more common with lung, renal cell, thyroid and breast CA. - Renal cell and Thyroid will typically present with aggressive osteolytic expansile mass aka “blowout
mets ” - In general, imaging approach should consist of Radiographic knee series, followed by MRI if
xrays are unrewarding - Tc99 Bone scintigraphy is the modality of choice to evaluate metastatic bone disease
Soft Tissue Neoplasms About the Knee
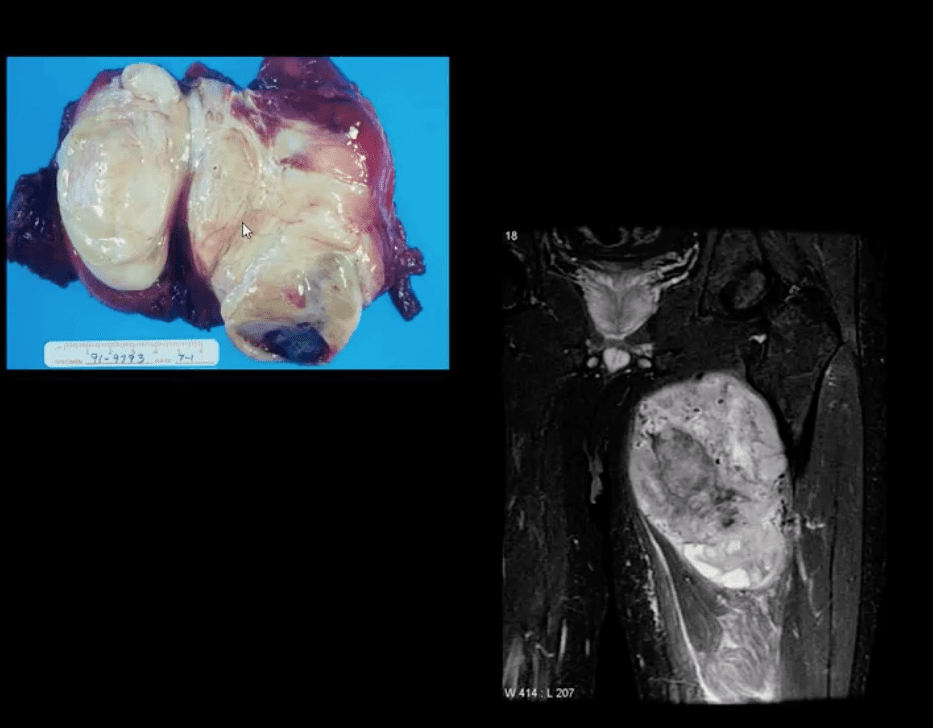
Malignant fibrous histiocytoma (MFH) reclassified as Pleomorphic Undifferentiated Sarcoma (PUS) is the m/c S.T. sarcoma. MFH is
aggressive biologically with poor prognosis
M>F (1.2:1) 30-80 with
Clinically: painful, hard mass typically about the knee or thigh. Histology: poorly differentiated/undifferentiated malignant fibroblasts, myofibroblasts
Imaging: MRI is the modality of choice with T1, T2, T1+C. Typically appears as
appear misleadingly encapsulated w/o true capsule
Management: operative with radiation and chemotherapy.
Synovial Sarcoma

Synovial sarcoma: common malignant ST neoplasm esp. in younger patients or older children/adolescents. M/C found in
Clinically: can present slowly as
Imaging is the key: radiography may reveal ST. density/mass. Some synovial sarcomas may show calcification and mistaken for Myositis Ossificanse or heterotopic bone formation
MRI with T1
DDx: MFH
Management: operative, chemo-radiation
Prognosis: variable depending on size, invasion, metastasis
For Complete List Of Bone & Soft Tissue Neoplasms
- http://bonetumor.org
- Further reading:
- https://emedicine.medscape.com/article/988516-differential
- https://www.ajronline.org/doi/10.2214/AJR.16.17434
- For further review of common childhood malignancies refer to:
- https://www.aafp.org/afp/2000/0401/p2144.html
Neoplasms of the Knee
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


