Anterior cervical discectomy and fusion (ACDF) is a procedure that treats chronic neck conditions and is the most common spinal surgery performed in the U.S. 30 percent of Americans a year experience neck pain, chronic neck pain and radiculopathy or pain that spreads out and radiates to other parts of the body, in this case down the arms.
It’s a procedure that can work wonders, but as many as two-thirds of patients continue to manage neck pain and dysfunction after ACDF. One of the best ways of managing neck pain and dysfunction is to exercise. Research shows that a prescribed exercise program right after surgery can help lessen the pain and create less dependence on medications. A 2020 study published in SPINE suggests that patients that began therapeutic exercises right away had better results than individuals that started an exercise program after the six-week checkup/examination.

Table of Contents
What Anterior Cervical Discectomy Fusion Treats
The procedure is performed on individuals with degenerative disc disease or a bulging or herniated disc. These conditions can cause the spinal disc to place pressure on the spinal cord and nerve roots that branch out, creating:
- Numbness
- Tingling
- Pain
- Weakness in one or both arms
Most individuals that are recommended to undergo the surgery experience symptoms that don’t respond to non-surgical therapies or medication/s. A significant symptom is hand/arm weakness and arm pain that’s worse than the neck pain.
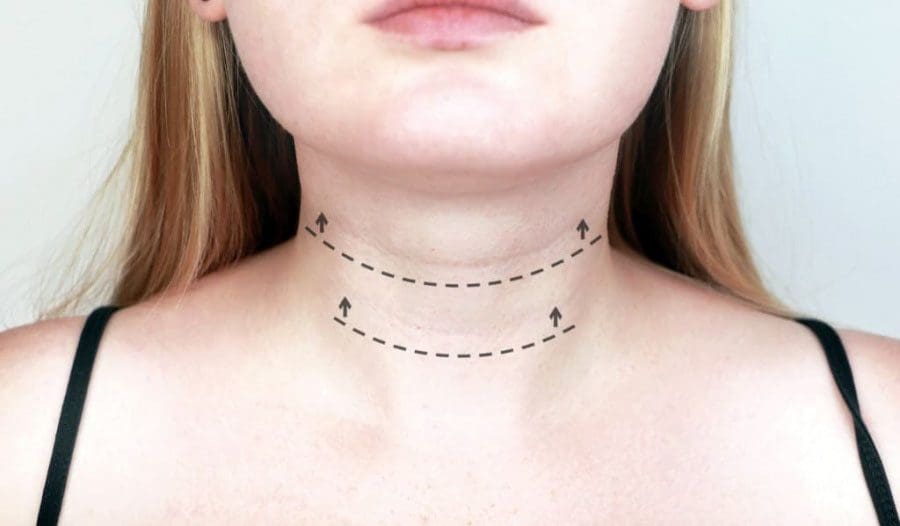
ACDF Surgery
The ACDF procedure is broken into two parts: a discectomy and a fusion. Anterior means in front and in this case it’s the front of the neck that the surgeon accesses the damaged discs. In a discectomy, the surgeon removes a portion/s or all of an intervertebral disc/s to release the pressure on the nerves. The fusion part fuses the two vertebrae together. This eliminates the painful movements. A bone graft is inserted between the vertebrae at the spot where the disc was removed. The bone graft serves as a structural scaffold that the body uses to build new tissue and cause the vertebrae to grow together.
The graft can come from three sources:
- Your own bone called an autograft, this is usually a piece of bone from the pelvis just above where the front jean pocket would be.
- Bone donation called an allograft that comes from a cadaver from a bone donor bank.
- Substitute material/s like man-made plastic, ceramic, or bioresorbable compounds.
Home Exercise Program
There are those that are of the opinion to hold off on physical therapy or exercise until about six weeks post-ACDF when recovery is established. However, the study suggests it is more effective to begin a home exercise program (HEP) as soon as possible. At this time telemedicine is the replacement for in-person physical therapy sessions but works just as well. The study examined 28 individuals’ outcomes over 12-months post-operation.
The participants were divided into two groups: Standard care and Early HEP. Both groups went through the standard postoperative care, along with medication, a cervical collar or neck brace, and restrictions of certain activities. The standard care group received physical therapy referral six weeks after surgery while the early HEP group was given a home exercise program to perform during the postoperative six-weeks.
This included walking and sleeping instructions and a range of motion/strengthening exercises. A cognitive-behavioral strategy was also given to help relax. The participants would phone-conference with a physical therapist on a weekly basis. Exercises increased in difficulty every two weeks, based on the therapists’ judgment. When compared to the standard care group, the early HEP group reported a reduction in short-term neck pain and were less likely to be using pain meds/opioids twelve months after their surgery.
Recovery Tips
Recovery time after ACDF surgery typically lasts about four to six weeks. If the bone graft was from the pelvis, there could be pain, soreness, and stiffness. To minimize discomfort, try not to sit or lie down for long periods. And remember to change position or take a quick short walk down the hall, to the kitchen, etc. every 20-30 minutes. If you are referred to physical therapy combine it with the home exercise program. The therapist will teach you exercises and proper form. Exercising ten minutes every day is far more effective than doing 45 minutes once a week.

Resuming normal activities gradually is crucial. No pain, no gain does not apply when recovering from ACDF surgery. Recovery exercises can feel great. However, pain and fatigue can sneak up the next day or the following week. Gradually easing back into daily activities can help avoid major setbacks. Work, shopping, house chores, childcare, and lawn care all fall into the activity category.
A recurrence of neck pain after recovery is normal. However, discomfort can be minimized by taking a few precautions.
- Use proper form when lifting
- Keep objects close to the body
- Keep the back flat as you lift
- Maintain neutral neck position
- Be aware of your posture when sitting, standing, walking, and sleeping
- Gradually increase the exercise program
- Don’t overdo it
- Address underlying fear/anxiety
- Fear of generating pain can cause tension and exacerbate or even create new pain symptoms
- Stop smoking, as it has shown to impede the fusion and heighten the risk for complications
ACDF surgery can improve quality of life. Your surgeon is responsible for performing the procedure, it’s up to the individual to follow through with an exercise program and proper ergonomics for optimal results.
Neck Pain Treatment
NCBI Resources
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


