Can individuals with lumbar spinal stenosis utilize spinal decompression to reduce low back pain and restore mobility?
Table of Contents
Introduction
Many individuals worldwide have dealt with low back pain at some point in their lives that has affected their mobility and impacted their routine. Numerous environmental factors can lead to low back pain development, like improper heavy lifting, poor posture, traumatic injuries, and accidents that can affect the surrounding muscles, spinal cord, and nerve roots. When this happens, it can lead to lumbar spinal stenosis and cause overlapping risk profiles that are correlated with low back pain. When people are dealing with lumbar spinal stenosis, they could be thinking that their pain is in the lower extremities. To that point, many individuals seek treatment to not only reduce low back pain but also reduce the effects of lumbar spinal stenosis. Some treatments, like spinal decompression, which is a non-surgical treatment, can help restore mobility to the body. Today’s article looks at how lumbar spinal stenosis affects the lower back and its diagnosis while looking at how spinal decompression can provide relief to the individual and have positive benefits in restoring mobility. We talk with certified medical providers who consolidate our patients’ information to assess how lumbar spinal stenosis correlates with lower back pain, causing mobility issues. We also inform and guide patients on how spinal decompression is an excellent form of treatment that can be combined with other therapies. We encourage our patients to ask their associated medical providers intricate and important questions about incorporating decompression therapy to relieve the pain effects caused by lumbar stenosis while reducing the overlapping pain effects like lower back pain to regain a person’s mobility. Dr. Jimenez, D.C., includes this information as an academic service. Disclaimer.
How Lumbar Spinal Stenosis Affects the Lower Back
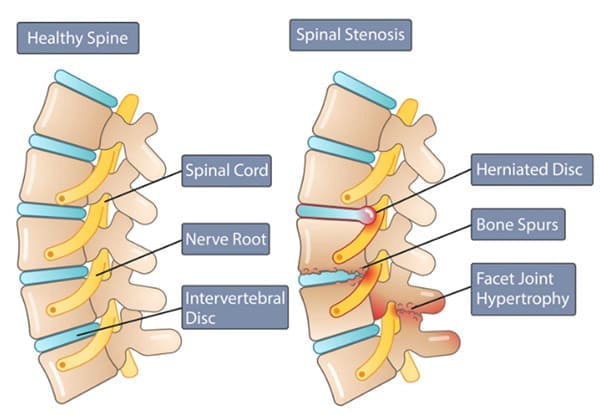
Do you feel tingling sensations in the back of your legs affecting your ability to move around? Or does your lower back feel less mobile than it is used to? When many individuals are experiencing low back pain during their lifetime, it can often correlate with lumbar spinal stenosis. Lumbar spinal stenosis usually occurs when the spinal canal in the lower back becomes constricted, leading to degenerative changes. When the spinal canal starts to narrow in the spine, it can cause significant discomfort, interfere with daily activities, and may result in progressive disability for many individuals. (Munakomi et al., 2024) The symptoms caused by lumbar spinal stenosis range from mild to severe, and on which environmental factors correspond to the issue. At the same time, lumbar spinal stenosis is characterized by symptoms like low back pain that can cause spondylotic changes that induce low back pain that can negatively impact a person’s quality of life. (Ogon et al., 2022) This causes many people to go to their primary doctors to get a diagnosis and learn how to manage the pain associated with lumbar spinal stenosis.
The Diagnosis Of Lumbar Spinal Stenosis
When it comes to diagnosing lumbar spinal stenosis, many healthcare providers will incorporate a comprehensive evaluation, which includes a physical examination to see how mobile a person’s back is and imaging testing like MRIs and CT scans to visualize the spinal canal and assess the extent of the narrowing that is causing pain in the lower extremities. This is because when individuals deal with lumbar spinal stenosis, it can manifest with neurogenic claudication in the lower extremities, especially when a person is standing or sitting. The pain is decreased when their position is changed. (Sobanski et al., 2023) Additionally, lumbar spinal stenosis is one of the most commonly diagnosed spinal disorders that many healthcare professionals assess and evaluate. When there is a narrowing in the spinal canal, leading to the development of lumbar spinal, simple motions like walking can exacerbate the symptoms to the lower extremities and increase the oxygen in the spinal nerves, which may exceed the available blood flow to the extremities. (Deer et al., 2019) To that point, treatments like spinal decompression can help reduce lower back pain associated with lumbar spinal stenosis.
The Non-Surgical Approach To Wellness- Video
A Path To Relief Using Spinal Decompression
When it comes to individuals experiencing the pain caused by lumbar spinal stenosis, many individuals can seek out non-surgical treatments like spinal decompression to relieve lower back pain. Spinal decompression has emerged as a non-invasive, effective treatment option for lumbar spinal stenosis. It utilizes gentle mechanical traction on the spine to be stretched, relieving the spinal nerves by creating more space within the spinal canal. Spinal decompression decreases the degenerative process while the surrounding muscles are gently stretched, and the spinal disc height increases due to negative pressure. (Kang et al., 2016)
The Benefits Of Spinal Decompression & Restoring Mobility
Additionally, the gentle traction from spinal decompression helps enhance the production flow of nutrients and oxygen back to the affected spinal discs and spine to foster a better healing environment for the body. Since spinal decompression can be combined with other non-surgical treatments, like physical therapy and spinal manipulation, it can provide long-lasting positive effects for individuals with lumbar spinal stenosis. (Ammendolia et al., 2022) Some of the beneficial results of spinal decompression include:
- Pain relief by alleviating pressure off the spinal nerves to reduce pain and discomfort in the lower extremities significantly.
- Improved mobility allows the individual to return to their daily activities with ease.
Many people can benefit from spinal decompression to reduce the effects of lumbar spinal stenosis and have their lower extremity mobility restored after consecutive sessions to reduce the chances of the pain from coming back. By thinking more about their health and wellness, many people can make small routine changes in their activities to mitigate the pain and remain mobile throughout their lives. This allows them to have a sense of hope to relieve them from the pain they have been under.
References
Ammendolia, C., Hofkirchner, C., Plener, J., Bussieres, A., Schneider, M. J., Young, J. J., Furlan, A. D., Stuber, K., Ahmed, A., Cancelliere, C., Adeboyejo, A., & Ornelas, J. (2022). Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. BMJ Open, 12(1), e057724. https://doi.org/10.1136/bmjopen-2021-057724
Deer, T., Sayed, D., Michels, J., Josephson, Y., Li, S., & Calodney, A. K. (2019). A Review of Lumbar Spinal Stenosis with Intermittent Neurogenic Claudication: Disease and Diagnosis. Pain Med, 20(Suppl 2), S32-S44. https://doi.org/10.1093/pm/pnz161
Kang, J. I., Jeong, D. K., & Choi, H. (2016). Effect of spinal decompression on the lumbar muscle activity and disk height in patients with herniated intervertebral disk. Journal of Physical Therapy Science, 28(11), 3125-3130. https://doi.org/10.1589/jpts.28.3125
Munakomi, S., Foris, L. A., & Varacallo, M. (2024). Spinal Stenosis and Neurogenic Claudication. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/28613622
Ogon, I., Teramoto, A., Takashima, H., Terashima, Y., Yoshimoto, M., Emori, M., Iba, K., Takebayashi, T., & Yamashita, T. (2022). Factors associated with low back pain in patients with lumbar spinal stenosis: a cross-sectional study. BMC Musculoskelet Disord, 23(1), 552. https://doi.org/10.1186/s12891-022-05483-7
Sobanski, D., Staszkiewicz, R., Stachura, M., Gadzielinski, M., & Grabarek, B. O. (2023). Presentation, Diagnosis, and Management of Lower Back Pain Associated with Spinal Stenosis: A Narrative Review. Med Sci Monit, 29, e939237. https://doi.org/10.12659/MSM.939237
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card