Abstract
This paper explores the relationship between traumatic ligament laxity of the spine and the resultant instability that may occur. Within, there is a discussion of the various spinal ligamentous structures that may be affected by macro and micro traumatic events and the neurologic and musculoskeletal effects of instability. There is a detailed discussion of the diagnosis, quantification, and documentation.
Soft tissue cervical and lumbar sprain/strains are the most common injury in motor vehicle collisions, with 28% to 53% of collision victims sustaining this type of injury (Galasko et al., 1993; Quinlan et al., 2000). The annual societal costs of these injuries in the United States are estimated to be between 4.5 and 8 billion dollars (Kleinberger et al., 2000; Zuby et al., 2010). Soft tissue injuries of the spinal column very often become chronic, with the development of long-term symptoms, which can inevitably adversely affect the victim’s quality of life. Research has indicated that 24% of motor vehicle collision victims have symptoms 1 year after an accident and 18% after 2 years (Quinlan et al., 2004). Additionally, it has been found that between 38% and 52% of motor vehicle collision cases involved rear-impact scenarios
It is well known that the major cause of chronic pain due to these injuries is directly related to the laxity of spinal ligamentous structures (Ivancic et al., 2008). Ligaments are fibrous bands or sheets of connective tissue linking two or more bones, cartilages, or structures. One must fully understand the structure and function of ligaments to realize the effects of traumatic ligament laxity. We know that one or more ligaments provide stability to a joint during rest and movement. Excessive movements such as hyper-extension or hyper-flexion, which occur during a traumatic event such as a motor vehicle collision, may be restricted by ligaments unless these forces are beyond the tensile strength of these structures; this will be discussed later in this paper.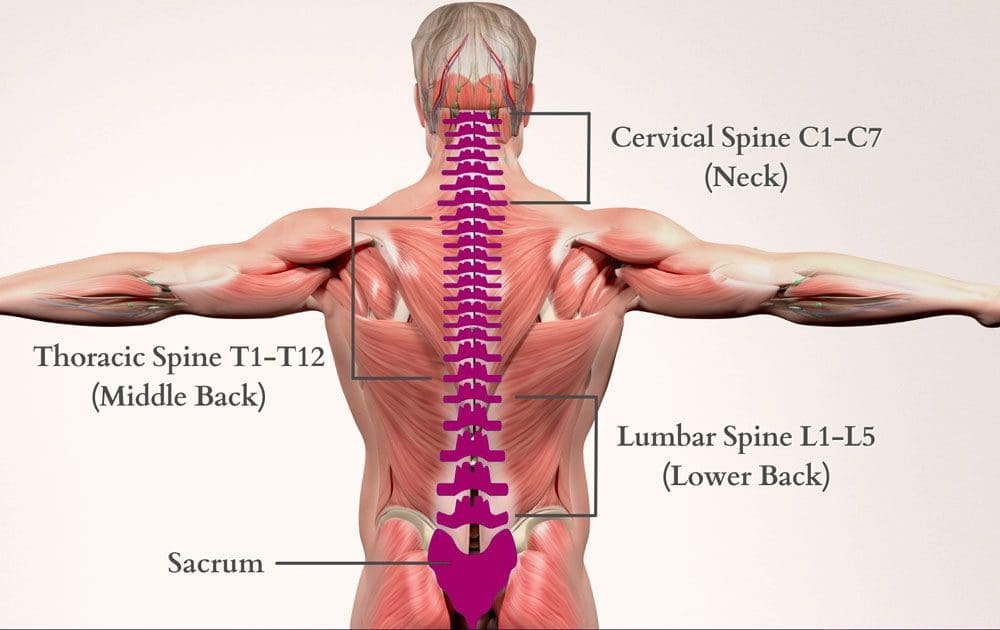
Table of Contents
Ligament Laxity Spine Injury Background
Three of the more important ligaments in the spine are the ligamentum flavum, the anterior longitudinal ligament, and the posterior longitudinal ligament (Gray’s Anatomy, 40th Edition). The ligamentum flavum forms a cover over the dura mater, a layer of tissue that protects the spinal cord. This ligament connects under the facet joints to create a small curtain, so to speak, over the posterior openings between vertebrae (Gray’s Anatomy, 40th edition). The anterior longitudinal ligament attaches to each vertebra’s front (anterior) and runs vertically or longitudinal (Gray’s Anatomy, 40th edition). The posterior longitudinal ligament also runs vertically or longitudinally behind (posterior) the spine and inside the spinal canal (Gray’s Anatomy, 40th Edition). AOtherligaments include facet capsular, interspinous, supraspinous, and intertransverse ligaments. The alignments above limit flexion and extension, except the ligament, which limits lateral flexion. The ligamentum nuchae, a fibrous membrane, limits flexion of the cervical spine (Gray’s Anatomy, 40th Edition). The four ligaments of the sacroiliac joints:
(iliolumbar, sacroiliac, sacrospinous, sacrotuberous), provide stability and some motion. The upper cervical spine has its own ligamentous structures or systems; the occipitoatlantal ligament complex, occipitoaxial ligament complex, atlantoaxial ligament complex, and the cruciate ligament complex (Gray’s Anatomy, 40th Edition). The upper cervical ligament system is especially important in stabilizing the upper cervical spine from the skull to C2 (axis) (Stanley Hoppenfeld, 1976). It is important to note that although the cervical vertebrae are the smallest, the neck has the greatest range of motion.
Causes of Ligament Laxity Injuries in the Spine
Ligament laxity may happen due to a ‘macro trauma”, such as a motor vehicle collision, or may develop over time due to repetitive use or work-related injuries. The cause of this laxity develops through similar mechanisms, which leads to the facet joints’ excessive motion and will cause various degrees of physical impairment. When ligament laxity develops over time, it is defined as “creep” and refers to the elongation of a ligament under constant or repetitive stress (Frank CB, 2004). Low-level ligament injuries, or those where the ligaments are simply elongated, represent the vast majority of cases and can potentially incapacitate a patient due to disabling pain, vertigo, tinnitus, etc. Unfortunately, these strains may progress to sub-failure tears of ligament fibers, leading to instability at the level of facet joints (Chen HB et al., 2009). Traumatic or repetitive causes of ligament laxity will ultimately produce abnormal motion and function between vertebrae under normal physiological loads, inducing irritation to nerves, possible structural deformation, and/or incapacitating pain.
Patients who have suffered a motor vehicle collision or a work-related injury often have chronic pain syndromes due to ligament laxity. The ligaments surrounding the facet joints of the spinal column, known as capsular ligaments, are highly innervated mechanoreceptive and nociceptive free nerve endings. Therefore, the facet joint is considered the primary source of chronic spinal pain (Boswell MV et al., 2007; Barnsley L et al., 1995). When the mechanoreceptors and nociceptors are injured or even irritated, the overall joint function of the facet joints is altered (McLain RF, 1993).
One must realize that instability is not similar to hyper-mobility. In the clinical context, instability implies a pathological condition with associated symptomatology, whereas joint hypermobility alone does not. Ligament laxity, which produces instability, refers to a loss of “motion stiffness,” so to speak, in a particular spinal segment when a force is applied to this segment, which produces a greater displacement than would be observed in a normal motion segment. When instability is present, pain and muscular spasms can be experienced within the patient’s range of motion and not just at the joint’s end-point. In Chiropractic, we understand that a “guarding mechanism” is triggered after an injury, which is the muscle spasm. These muscle spasms can cause intense pain and are the body’s response to instability since the spinal supporting structures, the ligamentous structures, act as sensory organs, which initiate a ligament-muscular reflex. This reflex is a “protective reflex” or “guarding mechanism” produced by the mechanoreceptors of the joint capsule, and these nerve impulses are ultimately transmitted to the muscles. Activation of surrounding musculature, or guarding, will help to maintain or preserve joint stability, either directly by muscles crossing the joint or indirectly by muscles that do not cross the joint but limit joint motion (Hauser RA et al., 2013). This reflex is fundamental to the understanding of traumatic injuries.
This reflex is designed to prevent further injury. However, the continued feedback and reinforcement of pain and muscle spasms will delay the healing process. The ‘perpetual loop” may continue for a long period of time, making further injury more likely due to muscle contraction. Disrupting this cycle of pain and inflammation is key to resolution.
When traumatic ligament laxity produces joint instability, with neurologic compromise, it is understood that the joint has sustained considerable damage to its stabilizing structures, which could include the vertebrae themselves. However, research indicates that joints that are hypermobile demonstrate increased segmental mobility but are still able to maintain their stability and function normally under physiological loads (Bergmann TF et al., 1993).
Clinical Diagnosis
Clinicians classify instability into 3 categories, mild, moderate, and severe. Severe instability is associated with a catastrophic injury like a motor vehicle collision. Mild or moderate clinical instability is usually without neurologic injury and is most commonly due to cumulative micro-trauma, such as those associated with repetitive use injuries, prolonged sitting, standing, flexed postures, etc.
In a motor vehicle collision, up to 10 times more force is absorbed in the capsular ligaments versus the intervertebral disc (Ivancic PC et al., 2007). This is true because, unlike the disc, the facet joint has a much smaller area to disperse this force. As previously discussed, the capsular ligaments become elongated, resulting in abnormal motion in the affected spinal segments (Ivancic PC et al., 2007; Tominaga Y et al., 2006). This sequence has been documented with both in vitro and in vivo studies of segmental motion characteristics after torsional loads and resultant disc degeneration (Stokes IA et al., 1987; Veres SP et al., 2010). Injury to the facet joints and capsular ligaments has been further confirmed during simulated whiplash traumas (Winkelstein BA et al., 2000).
Maximum ligament strains occur during shear forces, such as when a force is applied while the head is rotated (axial rotation). While capsular ligament injury in the upper cervical spine region can occur from compressive forces alone, exertion from a combination of shear, compression, and bending forces is more likely and usually involves much lower loads to cause injury (Siegmund GP et al., 2001). If the head is turned during a whiplash trauma, the peak strain on the cervical facet joints and capsular ligaments can increase by 34% (Siegmund GP et al., 2008). One research study reported that during an automobile rear-impact simulation, the magnitude of the joint capsule strain was 47% to 196% higher in instances when the head was rotated 60 degrees during impact compared with those when the head was forward facing (Storvik SG et al., 2011). Head rotation to 60 degrees is similar to an individual turning his/her head to one side while checking for on-coming traffic and suddenly experiencing a rear-end collision. The impact was greatest in the ipsilateral facet joints, such that head rotation to the left caused higher ligament strain at the left facet joint capsule.
Other research has illustrated that motor vehicle collision trauma has been shown to reduce ligament strength (i.e., failure force and average energy absorption capacity) compared with controls or computational models (Ivancic PC et al., 2007; Tominaga Y et al., 2006). This is particularly true in the case of capsular ligaments since this type of trauma causes capsular ligament laxity. Interestingly, one research study conclusively demonstrated that whiplash injury to the capsular ligaments resulted in an 85% to 275% increase in ligament elongation (laxity) compared to controls (Ivancic PC et al., 2007).
The study also reported evidence that trauma-related tension of the capsular ligaments is requisite for producing pain from the facet joint. Whiplash injuries cause compression injuries to the posterior facet cartilage. This injury also results in trauma to the synovial folds, bleeding, inflammation, and pain. Simply stated, this stretching injury to the facet capsular ligaments will result in joint laxity and instability.
Traumatic ligament laxity resulting in instability is a diagnosis based primarily on a patient’s history (symptoms) and physical examination. Subjective findings are the patient’s complaints in their own words or their perception of pain, sensory changes, motor changes, or range of motion alterations. After the patient presents their complaints to the clinician, these subjective findings must be correlated and confirmed through a proper and thorough physical examination, including imaging diagnostics that objectively explain a particular symptom, pattern, or area of complaint. Without concrete evidence explaining a patient’s condition, we merely have symptoms with no forensic evidence. Documentation is key, as well as quantifying the patient’s injuries objectively.
To adequately quantify the presence of instability due to ligament laxity, the clinician could utilize functional computerized tomography, functional magnetic resonance imaging scans, and digital motion x-ray (Radcliff K et al., 2012; Hino H et al., 1999). Studies using functional CT for diagnosing ligamentous injuries have demonstrated the ability of this technique to show excess movement during axial rotation of the cervical spine (Dvorak J et al., 1988; Antinnes J et al., 1994).
This is important to realize when patients have the signs and symptoms of instability but have normal MRI findings in the neutral position. Functional imaging technology, as opposed to static standard films, is necessary for the adequate radiologic depiction of instability because they provide dynamic imaging during movement and are extremely helpful for evaluating the presence and degree of instability.
Although functional imaging may be superior plain-film radiography is still a powerful diagnostic tool for evaluating instability due to ligament laxity. Performing a “Davis Series” of the cervical spine is common practice when a patient presents status-post motor vehicle collision. This x-ray series consists of 7 views: anterior-posterior open mouth, anterior-posterior, lateral, oblique, and flexion-extension views. The lumbar spine is treated in a similar fashion. X-ray views will include anterior-posterior, lateral, oblique, and flexion-extension views. The flexion-extension views are key in the diagnosis of instability. It is well known that the dominant motion of the cervical and lumbar spine, where most pathological changes occur, is flexion extension. Translation of one vertebral segment in relation to the one above and/or below will be most evident in these views. The translation is the total anterior-posterior movement of vertebral segments. After the appropriate views are taken, the images may be evaluated utilizing CRMA or Computed Radiographic Mensuration Analysis. These measurements are taken to determine the presence of ligament laxity. In the cervical spine, a 3.5mm or greater translation of one vertebra on another is an abnormal and ratable finding, indicative of instability (AMA Guides to the Evaluation of Permanent Impairment, 6th Edition).
Alteration of Motion Segment Integrity (AOMSI) is crucial as it relates to ligament laxity. The AMA Guides to the Evaluation of Permanent Impairment 6th Edition, recognize linear stress views of radiographs as the best form of diagnosing George’s Line (Yochum & Rowe’s Essentials of Radiology, page 149), which states that if there is a break in George’s Line on a radiograph, this could be a radiographic sign of instability due to ligament laxity.
Discussion
Our discussion of ligament laxity and instability continues with the “Criteria for Rating Impairment Due to Cervical and Lumbar Disorders,” as described in the AMA Guides to the Evaluation of Permanent Impairment, 6th Edition. According to the guidelines, a DRE (Diagnosed Related Estimate) Cervical Category IV is considered a 25% to 28% impairment of the whole person. Category IV is described as “alteration of motion segment integrity or bilateral or multilevel radiculopathy; alteration of motion segment integrity is defined from flexion and extension radiographs, as at least 3.5mm of translation of one vertebra on another, or angular motion of more than 11 degrees greater than at each adjacent level; alternatively, the individual may have a loss of motion of a motion segment due to a developmental fusion or successful or unsuccessful attempt at surgical arthrodesis; radiculopathy, as defined in Cervical Category III, need not be present if there is an alteration of motion segment integrity; or fractures: (1) more than 50% compression of one vertebral body without residual neural compromise. One can compare a 25% to 28% cervical impairment of the whole person to the 22% to 23% whole person impairment due to an amputation at the thumb level at or near the carpometacarpal joint or the distal third of the first metacarpal.
According to the guidelines, a DRE (Diagnosed Related Estimate) Lumbar Category IV is considered a 20% to 23% impairment of the whole person. Category IV is described as “loss of motion segment integrity defined from flexion and extension radiographs as at least 4.5mm of translation of one vertebra on another or angular motion greater than 15 degrees at L1-2, L2-3, and L3-4, greater than 20 degrees at L4-5, and greater than 25 degrees at L5-S1; may have a complete or near complete loss of motion of a motion segment due to developmental fusion, or a successful or unsuccessful attempt at surgical arthrodesis or fractures: (1) greater than 50% compression of one vertebral body without residual neurologic compromise. One can compare a 20% to 23% Lumbar Impairment of the whole person to the 20% whole person impairment due to an amputation of the first metatarsal bone.
Conclusions
After careful interpretation of the AMA Guides to the Evaluation of Permanent Impairment, 6th Edition, regarding whole-person impairment due to ligament laxity/instability of the cervical and lumbar spine, one can see the severity and degree of disability that occurs. Once ligament laxity is correctly diagnosed, it will objectively quantify a patient’s spinal injury regardless of symptoms, disc lesions, range of motion, reflexes, etc. When we quantify the presence of ligament laxity, we also provide a crucial element to demonstrate instabilities in a specific region. Overall, clarifying and quantifying traumatic ligament laxity will help the patient legally, objectively, and, most importantly, clinically.
Adrenal Insufficiency
Additional Topics: Preventing Spinal Degeneration
Spinal degeneration can occur naturally over time due to age and the constant wear-and-tear of the vertebrae and other complex structures of the spine, generally developing in people over the age of 40. Occasionally, spinal degeneration can also occur due to spinal damage or injury, which may result in further complications if left untreated. Chiropractic care can help strengthen the spine’s structures, helping prevent spinal degeneration.
References
AMA Guides to the Evaluation of Permanent Impairment, 6th Edition
Antinnes J, Dvorak J, Hayek J, Panjabi MM, Grob D. The value of functional computed tomography in the evaluation of soft-tissue injury in the upper cervical spine. Eur Spine J. 1994; 98-101. [PubMed]
Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of cervical zygapophyseal joint pain after whiplash. Spine (Phila Pa 1976). 1995;20: 20-5. [PubMed]
Bergmann TF, Peterson DH. Chiropractic technique principles and procedures, 3rd ed. New York Mobby Inc. 1993
Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007;10(1): 229-53. [PubMed]
Chen HB, Yang KH, Wang ZG. Biomechanics of whiplash injury. Chin J Traumatol.2009;12(5): 305-14. [PubMed]
Dvorak J, Penning L, Hayek J, Panjabi MM, Grob D, Zehnder R. Functional diagnostics of the cervical spine using computer tomography. Neuroradiology. 1988;30: 132-7. [PubMed]
Examination of the Spine and Extremities, Stanley Hoppenfeld, 1976
Frank CB. Ligament structure, physiology, and function. J Musculoskelet Neuronal Interact. 2004;4(2): 199-201. [PubMed]
Galasko, C.S., P.M. Murray, M. Pitcher, H. Chanter, S. Mansfield, M. Madden, et al. Neck sprains after road traffic accidents: a modern epidemic. Injury 24(3): 155-157, 1993
American Medical Association. (2009). Guides to the evaluation of permanent impairment,
6th edition. Chicago, Il: AMA
Antinnes, J., Dvorak, J., Hayek, J., Panjabi, M.M., & grob, D. (1994). The value of functional
Computed tomography in the evaluation of soft tissue injury in the upper cervical
spine. European Spine Journal, 98-101.
Barnsley, L., Lord, S.M., Wallis, B.J., & Bogduk, N. (1995). The prevalence of cervical zygapophyseal
joint pain after whiplash. Spine, 20, 20-25.
Bergmann, T.F., & Peterson, D.H. (1993). Chiropractic technique principles and procedures,
3rd edition. New York: Mobby Inc.
Boswell, M.V., Colson, J.D., Sehgal, N., Dunbar, E.E., & Epter, R. (2007). A symptomatic review
of therapeutic facet joint interventions in chronic spinal pain. Pain Physician, 10(1),
229-253.
Chen, H.B., Yang, K.H., & Wang, Z.G. (2009). Biomechanics of whiplash injury. Chinese Journal
Traumatol, 12(5), 305-314.
Dvorak, J., Penning, L., Hayek, J., Panjabi, M.M., Grob, D., & Zehnder, R. (1988). Functional
diagnostics of the cervical spine using computer tomography. Neuroradiology, 30, 132-
137.
Frank, C.B. (2004). Ligament structure, physiology, and function. Musculoskeletal Neuronal
Interaction, 4, 199-201.
Galasko, C.S., Murray, P.M., Pitcher, M., Chantar, S., & Mansfield, M. (1993). Neck sprains after
road traffic accidents: A modern epidemic. Injury, 24(3), 155-157.
Gray, H. (2008). Gray’s anatomy. London: Churchill Livingstone/Elsevier.
Hoppenfeld, S. (1976). Physical examination of the spine and extremities. East Norwalk, CT:
Appleton-Century-Crofts.
Ivancic, P.C., Coe, M.P., & Ndu, A.B. (2007). Dynamic mechanical properties of intact human
cervical ligaments. Spine Journal, 7(6), 659-665.
Ivancic, P.C., Ito, S., Tominaga, Y., Rubin, W., Coe, M.P., Ndu, A.B., et al. (2008). Whiplash causes
Increased laxity of cervical capsular ligament. Clinical Biomechanics (Bristol Avon).
Kleinberger, M. (2000). Frontiers in whiplash trauma. Amsterdam: ISO Press.
Siegmund, G.P., Davis, M.B., & Quinn, K.P. (2008). Head-turned postures increase the risk of
cervical facet capsule injury during whiplash. Spine, 33(15), 1643-1649.
Siegmund, G.P., Meyers, B.S., Davis, M.B., Bohnet, H.F., & Winkelstein, B.A. (2001). Mechanical
evidence of cervical facet capsule injury during whiplash, a cadaveric study using
combined shear, compression, and extension loading. Spine, 26(19), 2095-2101.
Stokes, I.A., & Frymoyer, J.W. (1987). Segmental motion and instability. Spine, 7, 688-691.
Storvik, S.G., & Stemper, B.D. (2011). Axial head rotation increases facet joint capsular ligament
strains in automotive rear impact. Medical Bioengineeering Comput., 49(2), 153-161.
Tominaga, Y., Ndu, A.B., & Coe, M.P. (2006). Neck ligament strength is decreased following
whiplash trauma. BMC Musculoskeletal Disorders, 7, 103.
Veres, S.P., Robertson, P.A., & Broom, N.D. (2010). The influence of torsion on disc herniation
when combined with flexion. European Spine Journal, 19, 1468-1478.
Winkelstein, B.A., Nightingale, R.W., Richardson, W.J., & Myers, B.S. (2000). The cervical
facet capsule and its role in whiplash injury: A biomechanical investigation. Spine,
25(10), 1238-1246.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


