It’s the weekend in the backyard doing some chores, grilling, etc, while several kids play and jump on a nearby trampoline. The joviality from all this fun is filled with laughter, screams of joy, and other sounds or game instructions from one child to another. Then there is silence. The kids are huddled around their friend. One of the children fell off flat on their back.
The paramedics arrive and immobilize the head, neck, and spine strapping the child to a backboard and off to the hospital where there is no severe damage, just some mild bruising but everything turned out ok. This was a made-up scenario but unfortunately, emergency room doctors are seeing and treating this type of injury more and more.

Table of Contents
Statistics
The statistics of the number of trampoline-related injuries treated in emergency rooms.
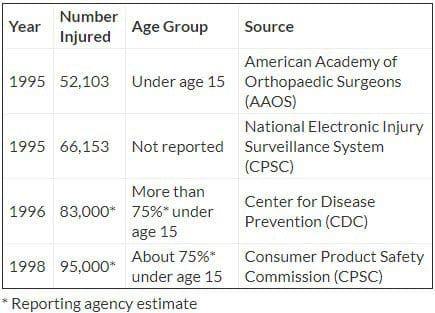
A simple analysis of the above stats is shocking. This means that since 1995, the number of injuries has increased between 30 and 45 percent. The CDC states that around 10 percent of trampoline injuries affect the head and neck. Many injuries are minor like bruising, scrapes and whatnot but some can be serious like broken bones, blunt-force trauma, and even paralysis.
For Home
Most of us see trampolines as a toy but are not aware of the dangers that come with it. Most injuries take place on trampolines purchased for home use. The American Academy of Pediatrics recommends that parents never let their children use a friend’s trampoline. While the American Medical Association recommends children should not be allowed to play/jump on a trampoline, even with adult supervision.
Trampoline Safety
Equipment Tips
A full-size trampoline consists of flexible fabric attached to a metal frame with springs, hooks, and a safety mesh/net. Most are around three feet off the ground. Consider the following safety tips:
- Read the information and instructions provided by the trampoline manufacturer. Give this information to anyone who will be using the trampoline.
- The proper placement of the trampoline is very important. Look at the location and surrounding area. Don’t place the trampoline close to a house/building, playground equipment, a swimming pool, the street, electrical lines, outdoor appliances, and plants/trees.
- Remember a child can bounce 10 feet or higher in the air from a trampoline.
- Make sure the springs, hooks, and frame are secured and covered with sturdy shock-absorbing pads.
- There should be shock-absorbing material all-around and under the trampoline. Use the owner’s manual for recommended materials.
- Stores where trampolines are sold often sell special padding.
- Check the trampoline for wear and tear often. Which include the frame’s structure like the screws, bolts springs, hooks, and fabric.

Using the Trampoline
- Step-ladders, boxes, and chairs to climb on the trampoline should be kept out of reach to prevent children from using the equipment without permission. And they should be moved out of the way once the individuals are on.
- Do not use the trampoline when darkness begins to take over like sunset. Individuals cannot see and when up in the air judging distance and where the trampoline is can be difficult/impossible.
- Before use, warm-up with a few exercises. To make sure muscles are loose and ready to react.
- Children need adult supervision at all times. Judging distances, foreseeing danger and quick reaction in situations that can become dangerous require an adult.
- At least two adults are needed to spot the individuals and help prevent anyone from falling off.
- Most want to jump together but too many people on a trampoline can be dangerous. Limit the number of people to where they can bounce safely without bumping into someone else, or falling off from lack of space.
- CDC reports that half of all injuries happen when more than two people use a trampoline. Usually, this happens with children that are lightweight, still not fully coordinated, and can’t control how they move, especially in the air.
- Learn how to land properly.
- Unless a professional or expertly trained do not try somersaults, backflips, stunts, or crazy acrobatics.
- Don’t jump or bounce off the trampoline.
Professional Help
There are professional gymnastic centers that have trampolines with padding all around and also give lessons/classes on proper usage. This could help a great deal, as it could be a safe alternative instead of home use. But if not then take the classes which could save a trip to an emergency room!
As El Paso’s Chiropractic Rehabilitation & Integrated Medicine Center, we are focused on treating patients after debilitating injuries and chronic pain conditions. We focus on improving your ability through flexibility, mobility and agility programs tailored for all age groups and disabilities.
Best Sports Injury Chiropractor El Paso, TX.
NCBI Resources
Spinal cord injuries occur more in the neck or cervical spine. Around 60% of cases involve the neck, followed by the mid-back or thoracic spine that averages to around 32% of injuries. Although most people experience low-back pain, only 9% of spinal injuries occur in the low back and tailbone or lumbosacral spine.
Damage to the spinal cord not only affects the area where the point of impact occurred. The primary injury can also damage cells, dislocate the vertebrae and cause spinal compression. It can also trigger secondary injuries, that cause a series of biological changes. This can happen within weeks or months after the injury.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



