For individuals looking to improve their spinal health, can understanding the anatomy of the intervertebral foramen help in injury rehabilitation and prevention?
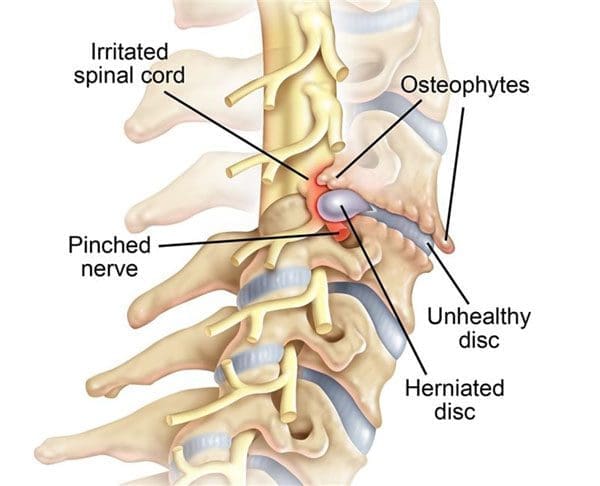
Table of Contents
Intervertebral Foramen
The intervertebral foramen, aka neural foramen, is the opening between the vertebrae through which spinal nerve roots connect and exit to other body areas. If the foramina narrows, it can place added pressure on the nerve roots near and around them, causing pain symptoms and sensations. This is known as neuroforaminal stenosis. (Sumihisa Orita et al., 2016)
Anatomy
- The vertebrae comprise the spinal column.
- They protect and support the spinal cord and most of the weight placed on the spine.
- Foramen is the singular form, and foramina is the plural form.
Structure
- The body is the large, round part of the bone that makes up each vertebra.
- The body of each vertebra is attached to a bony ring.
- As the vertebrae are stacked on each other, the ring creates a tube through which the spinal cord passes. (American Academy of Orthopaedic Surgeons 2020)
- The intervertebral foramen opening is between every two vertebrae, where the nerve roots exit the spine.
- Two neural foramina exist between each pair of vertebrae, with one on each side.
- The nerve roots move through the foramen to the rest of the body.
Function
- The intervertebral foramina are exits from which the nerve roots leave the spine and branch out to the rest of the body.
- Without the foramen, nerve signals cannot transmit to and from the brain to the body.
- Without nerve signals, the body is unable to function correctly.
Conditions
A common condition that can affect the neuroforamina is spinal stenosis. Stenosis means narrowing.
- Spinal stenosis is (not always) usually an age-related disorder associated with arthritis. (American Academy of Orthopaedic Surgeons, 2021)
- Stenosis can occur in the spinal canal, known as central canal stenosis, and the foramina.
- Pain brought on by neuroforaminal spinal stenosis and arthritis-related bone growth/bone spurs/osteophytes that are present in one or more foramen rub against the nerve root that passes through the space, causing radicular pain.
- Pain accompanied by other sensations, like tingling or numbness, is known as radiculopathy. (Young Kook Choi, 2019)
- The main symptom is pain.
- Numbness and/or tingling can present depending on the injury.
- Neurogenic claudication occurs as a result of ischemia or a lack of blood circulation to the nerves and typically presents with a heaviness in the legs.
- It is typically associated with central stenosis rather than foraminal stenosis.
- Most individuals with spinal stenosis feel better when flexing or bending forward and worse when arching their backs.
- Other symptoms include weakness and/or difficulty walking. (Seung Yeop Lee et al., 2015)
Treatment
Stenosis treatment aims to relieve pain and prevent nerve symptoms from occurring or worsening. Conservative treatments are recommended and can be highly effective.
These include:
- Physical therapy
- Acupuncture and Electroacupuncture
- Chiropractic
- Non-surgical decompression
- Therapeutic massage
- Nonsteroidal anti-inflammatory drugs/NSAIDs
- Targeted exercises and stretches
- Cortisone injections. (American Academy of Orthopaedic Surgeons, 2021)
- Surgery is usually not necessary.
However, a doctor may recommend surgery for an individual who is experiencing:
- Radiculopathy – pain, pins and needles, electrical sensations, and/or weakness going down one arm or leg (Jon Lurie, Christy Tomkins-Lane, 2016)
- Neurogenic claudication in the lower back (Jon Lurie, Christy Tomkins-Lane, 2016)
- Myelopathy in the neck and/or upper or mid-back (myelopathy symptoms are spinal cord related and occur in central canal stenosis) (Cleveland Clinic. 2021)
- Intense incapacitating pain
Different surgical techniques include:
- Decompression laminectomy – entails removing the buildup of bone in the spinal canal.
- Spinal fusion – when there is instability of the spine or severe foraminal stenosis.
- However, most cases don’t require fusion. (American Academy of Orthopaedic Surgeons, 2021)
Root Causes Spinal Stenosis
References
Orita, S., Inage, K., Eguchi, Y., Kubota, G., Aoki, Y., Nakamura, J., Matsuura, Y., Furuya, T., Koda, M., & Ohtori, S. (2016). Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie, 26(7), 685–693. https://doi.org/10.1007/s00590-016-1806-7
American Academy of Orthopaedic Surgeons. (2020). Spine Basics (OrthoInfo, Issue. https://orthoinfo.aaos.org/en/diseases–conditions/spine-basics/
American Academy of Orthopaedic Surgeons. (2021). Lumbar spinal stenosis (OrthoInfo, Issue. https://orthoinfo.aaos.org/en/diseases–conditions/lumbar-spinal-stenosis/
Choi Y. K. (2019). Lumbar foraminal neuropathy: an update on non-surgical management. The Korean journal of pain, 32(3), 147–159. https://doi.org/10.3344/kjp.2019.32.3.147
Lee, S. Y., Kim, T. H., Oh, J. K., Lee, S. J., & Park, M. S. (2015). Lumbar Stenosis: A Recent Update by Review of Literature. Asian spine journal, 9(5), 818–828. https://doi.org/10.4184/asj.2015.9.5.818
Lurie, J., & Tomkins-Lane, C. (2016). Management of lumbar spinal stenosis. BMJ (Clinical research ed.), 352, h6234. https://doi.org/10.1136/bmj.h6234
Cleveland Clinic. (2021). Myelopathy (Health Library, Issue. https://my.clevelandclinic.org/health/diseases/21966-myelopathy
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


