The gut-brain connection is essential in the body. If an individual has a leaky gut that is causing inflammation, it can send the signal to the brain and it can create problems like neurotransmitter dysfunction to systems that just don’t connect. The leaky gut can lead to brain dysfunction or brain dysfunction can lead to leaky gut. Sometimes an autoimmunity disease in the stomach can lead to a disruption in the mind. Then, brain disruption can also lead to inflammation in the gut. It’s a never-ending loop that the brain and gut can go on forever. Studies have stated that gut microbiota appears to influence the development of emotional behaviors like stress, pain modulation systems, and brain neurotransmitter systems.
Table of Contents
The Brain System to the Gut System
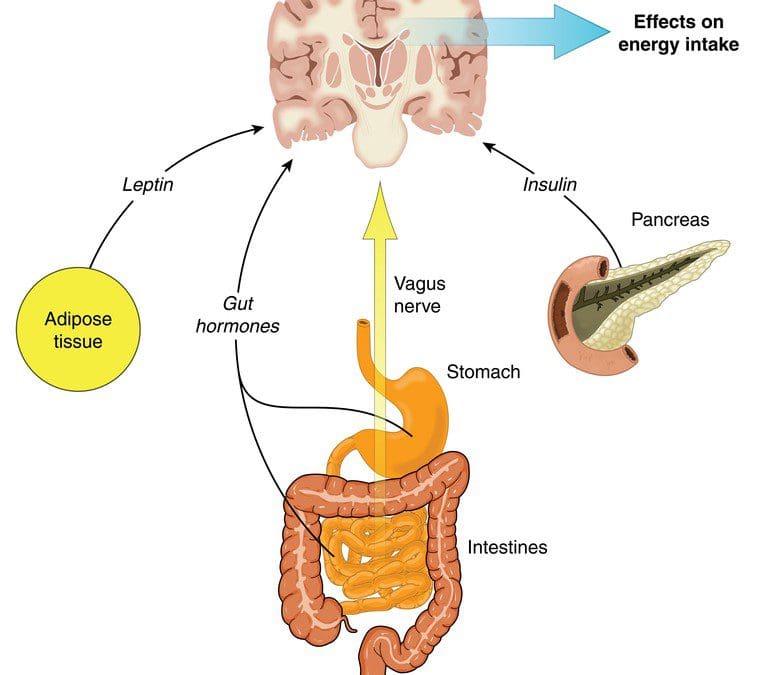
The brain is the main control room that controls the body’s system and how the body should behave. The human brain also contains neuron cells that are found in the central nervous system. With the gut-brain connection, two critical systems help send the signal to the brain and the gut; these are known as the vagus nerve and the neurotransmitters.
The Vagus Nerve
There are approximately 100 billion neurons in the brain, while the gut contains about 500 million neurons, which is connected to the brain through the nerves in the nervous system. The vagus nerve is one of the most significant nerves that send signals back and forth to the brain and the gut. When the body is stressed, the stress signal inhibits the vagus nerve, and it can cause problems to the gut-brain connection. Animal studies have shown that any stress that is in the animal’s body can cause gastrointestinal issues and PTSD. While another study stated that individuals that have IBS (irritable bowel syndrome) have a reduced function of the vagus nerve.
There are ways to reduce the stress hormone so that the vagus nerve can function properly and send the right signals to the gut and the brain. Probiotic foods can help lower the amount of stress hormone in the bloodstream. When that happens, the body can start healing naturally when the stress is reduced; however, if the vagus nerve is damaged, then the probiotic has no effect.
Neurotransmitters
Neurotransmitters are produced chemically in the brain by controlling feelings and emotions in the body. Since the brain and gut are connected to neurotransmitters, the neurotransmitters can create these compounds that help contribute to the body. In the brain, the neurotransmitter can produce serotonin to make the person feel happy and help control their body’s biological clock.
In the gut, there are trillions of microbes that live there, and interestingly researchers stated that serotonin is mainly being produced by the gut system. Another neurotransmitter that is provided in the gut is called GABA (gamma-aminobutyric acid), which helps control the feeling of fear and anxiety. When the brain feels overly anxious or has been through a traumatic experience that has caused them to be fearful, it can cause them to be hypersensitive and can cause a chemical imbalance to the gut, causing inflammation or leaky gut if it is severe.
The Gut System to the Brain System
The gut microbes can produce neurotransmitters to send to the brain, protect the intestinal barrier and the tight junction integrity, regulate the mucosal immune system, and modulates the enteric sensory afferents. The gut microbe produces a lot of SCFA (short-chain fatty acids) that form a barrier between the brain and blood flow called the blood-brain barrier. The blood-brain barrier protects the CNS (central nervous system) from toxins, pathogens, inflammation, injury, and disease.
The gut microbes also metabolize bile and amino acids to help produce other chemicals that affect the brain. When the body is stressed, it can reduce the production of bile acid by gut bacteria and alter the genes that are involved. When that stress is still creating problems in mind, the gut can develop gastrointestinal issues that will destroy the permeability barrier that is protecting the intestines.
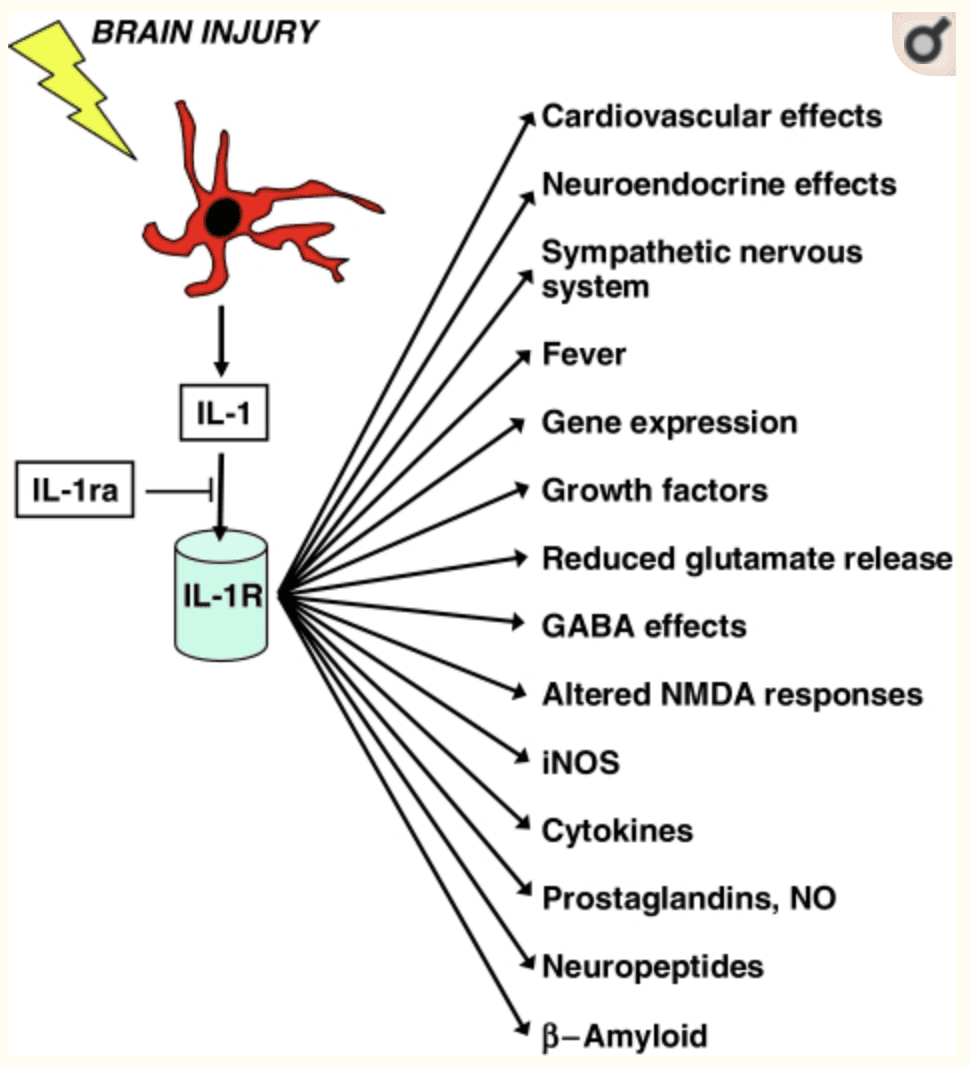
The gut-brain connection plays an essential role in the body’s immune system as it controls inflammation and what passes into the body. Since the immune system controls inflammation, if it is turned on for too long, inflammation can occur as well as several brain disorders like depression and Alzheimer’s disease. Stress can even disrupt the gut by causing contractions to the GI tract, make inflammation worse in the intestinal permeability, and making the body more at risk to infections.
When the body starts to alleviate stress, it can naturally heal itself, and the gut-brain connection can begin functioning normally. With changes in a person’s eating habits and lifestyle, it can drastically change a person’s mood and recover from intestinal ailments they may have. If the brain feels right, then the gut feels good as well. They work together side by side to make sure that the body is functioning correctly. When either one is being disrupted, then the body does not function properly.
Conclusion
Therefore, the gut-brain connection is vital to the body. Neurotransmitters and other components that are in both systems work together to make sure that the body is working correctly. When one of the connections is being disrupted, however, the body can develop many chronic illnesses even if the person seems fine. By altering little things like changing a person’s diet and lifestyle, it can help improve the body and bring the balance back to the gut-brain connection.
In honor of Governor Abbott’s proclamation, October is Chiropractic Health Month. To learn more about the proposal on our website.
The scope of our information is limited to chiropractic, musculoskeletal, and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
References:
Anguelova, M, et al. “A Systematic Review of Association Studies Investigating Genes Coding for Serotonin Receptors and the Serotonin Transporter: I. Affective Disorders.” Molecular Psychiatry, U.S. National Library of Medicine, June 2003, www.ncbi.nlm.nih.gov/pubmed/12851635.
Bravo, Javier A, et al. “Ingestion of Lactobacillus Strain Regulates Emotional Behavior and Central GABA Receptor Expression in a Mouse via the Vagus Nerve.” Proceedings of the National Academy of Sciences of the United States of America, National Academy of Sciences, 20 Sept. 2011, www.ncbi.nlm.nih.gov/pubmed/21876150.
Carabotti, Marilia, et al. “The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems.” Annals of Gastroenterology, Hellenic Society of Gastroenterology, 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/.
Daneman, Richard, and Alexandre Prat. “The Blood-Brain Barrier.” Cold Spring Harbor Perspectives in Biology, Cold Spring Harbor Laboratory Press, 5 Jan. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4292164/.
Herculano-Houzel, Suzana. “The Human Brain in Numbers: a Linearly Scaled-up Primate Brain.” Frontiers in Human Neuroscience, Frontiers Research Foundation, 9 Nov. 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC2776484/.
Lucas, Sian-Marie, et al. “The Role of Inflammation in CNS Injury and Disease.” British Journal of Pharmacology, Nature Publishing Group, Jan. 2006, www.ncbi.nlm.nih.gov/pmc/articles/PMC1760754/.
Mayer, Emeran A, et al. “Gut/Brain Axis and the Microbiota.” The Journal of Clinical Investigation, American Society for Clinical Investigation, 2 Mar. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4362231/.
Mayer, Emeran A. “Gut Feelings: the Emerging Biology of Gut-Brain Communication.” Nature Reviews. Neuroscience, U.S. National Library of Medicine, 13 July 2011, www.ncbi.nlm.nih.gov/pmc/articles/PMC3845678/.
Mazzoli, Roberto, and Enrica Pessione. “The Neuro-Endocrinological Role of Microbial Glutamate and GABA Signaling.” Frontiers in Microbiology, Frontiers Media S.A., 30 Nov. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5127831/.
Pellissier, Sonia, et al. “Relationship between Vagal Tone, Cortisol, TNF-Alpha, Epinephrine and Negative Affects in Crohn’s Disease and Irritable Bowel Syndrome.” PloS One, Public Library of Science, 10 Sept. 2014, www.ncbi.nlm.nih.gov/pubmed/25207649.
Rooks, Michelle G, and Wendy S Garrett. “Gut Microbiota, Metabolites and Host Immunity.” Nature Reviews. Immunology, U.S. National Library of Medicine, 27 May 2016, www.ncbi.nlm.nih.gov/pubmed/27231050.
Sahar, T, et al. “Vagal Modulation of Responses to Mental Challenge in Posttraumatic Stress Disorder.” Biological Psychiatry, U.S. National Library of Medicine, 1 Apr. 2001, www.ncbi.nlm.nih.gov/pubmed/11297721.
Yano, Jessica M, et al. “Indigenous Bacteria from the Gut Microbiota Regulate Host Serotonin Biosynthesis.” Cell, U.S. National Library of Medicine, 9 Apr. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4393509/.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


