An axillary nerve injury can cause pain, weakness, and shoulder mobility loss. Can physical therapy help restore and maintain shoulder joint flexibility?
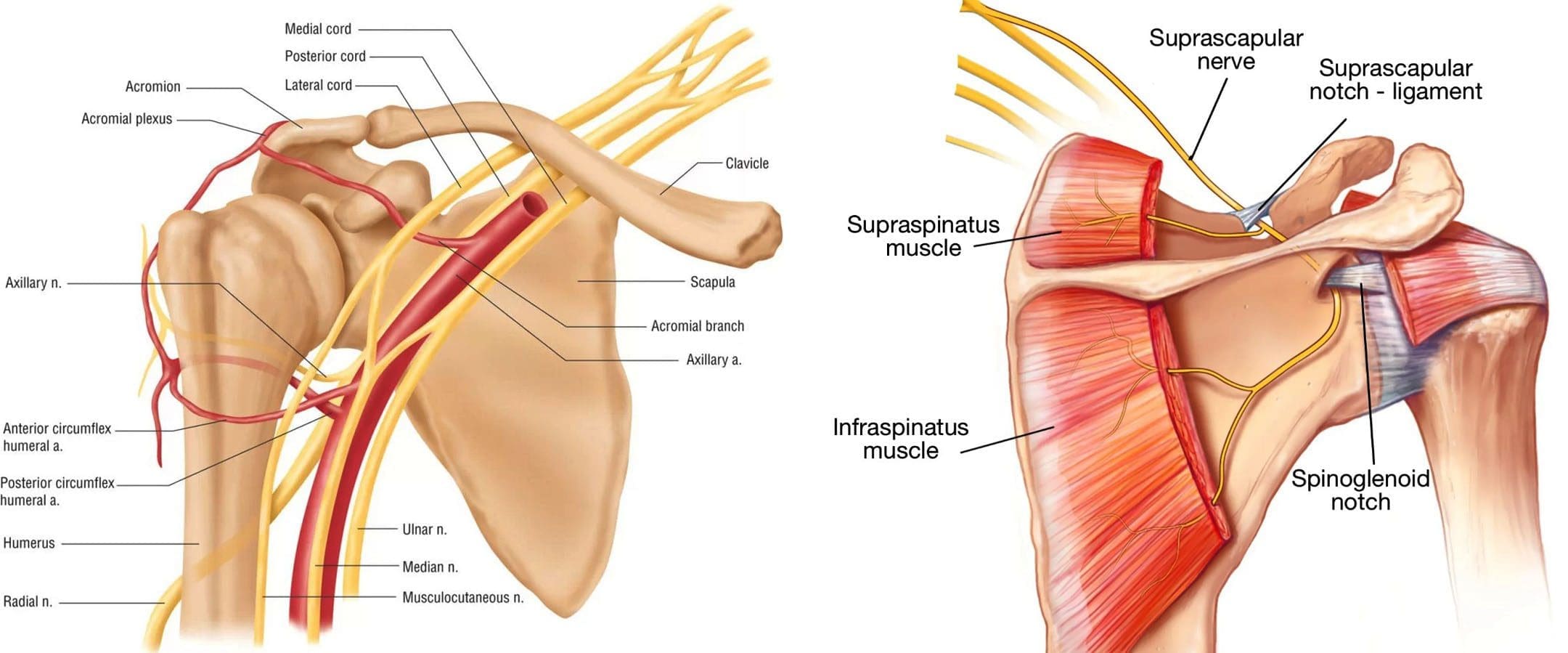
Table of Contents
Axillary Nerve
The axillary nerve, or the circumflex nerve, is a peripheral nerve that runs through the shoulder and supports movement and sensation in the upper limbs. It originates in the neck at the brachial plexus, a network of nerves that extends from the neck and upper torso to the shoulders and arms. Its primary purpose is to supply nerve function to the shoulder joint and three muscles in the arm and also innervates some skin in the region.
Anatomy
Except for the cranial nerves, all the body’s nerves branch off from the spinal cord, emerge from between vertebrae and continue to branch off as they travel to various muscles and other structures. The axillary nerve is named after the axilla, the medical name for the armpit. Individuals have two, one on each side. After leaving the spinal column, the axillary nerve runs behind the axillary artery and continues to the shoulder blade’s lower edge of the subscapularis muscle. It winds back and travels down the arm along the posterior humeral circumflex artery, which then passes through the quadrangular space (a small area of the shoulder blade just above the armpit where there is a gap in the muscles that allows nerves and blood vessels to pass through to the arm before it divides into terminal branches, which are:
Anterior Division
- Supplies motor innervation to the deltoid’s anterior and middle heads, allowing the arm to abduct or move away from the body.
- It winds around the neck of the humerus/funny bone, goes beneath the deltoid muscle, and then connects to the forward edge of the deltoid.
- A few small cutaneous branches serve the skin in that area.
Posterior Division
- Innervates the teres minor muscles and the lower part of the deltoid.
- It enters the deep fascia and becomes the superior lateral cutaneous nerve.
- It then wraps around the lower edge of the deltoid, connects to the skin over the lower two-thirds of the muscle, and covers the long head of the triceps brachii.
Articular Branch
- Comes from the trunk of the axillary nerve and enters the glenohumeral joint, which is in the shoulder, below the subscapularis muscle.
Anatomical Variations
In a case report, healthcare providers noted an incidence of the nerve branching directly off the upper trunk of the brachial plexus rather than the posterior cord. (Subasinghe S. K. and Goonewardene S. 2016) In this case, it innervated the subscapularis muscle, latissimus dorsi, and the deltoid and teres minor muscles and also had a communicating branch to the posterior cord. Another case documented multiple abnormalities in the course of the axillary nerve in an individual with pain and severely limited shoulder mobility. (Pizzo R. A. et al., 2019) During reverse shoulder arthroplasty, the surgeon discovered that the axillary nerve ran beside the coracoid process instead of underneath and stayed close to the subscapularis muscle instead of traveling through the quadrangular space. The case noted earlier reports of axillary nerves not running through the quadrangular space. In those cases, the nerve pierced the subscapularis muscle or split into branches before reaching the quadrangular space.
Function
The axillary nerve functions as a motor nerve that controls movement and a sensory nerve that controls sensations like touch or temperature.
Motor
As a motor nerve, the axillary nerve innervates three muscles in the arm and includes:
Deltoid
- Allows flexing of the shoulder joint and rotating the shoulder inward.
Long Head of the Triceps
- It runs down the back of the outer arm, allowing straightening, pulling the upper arm toward the body, or extending it backward.
- The radial nerve can also innervate this muscle.
Teres Minor
- One of the rotator cuff muscles starts outside the shoulder and runs diagonally along the bottom edge of the shoulder blade.
- It works with other muscles to allow for the external rotation of the shoulder joint.
Sensory
In its sensory role, the nerve carries information to the brain from the following:
- Glenohumeral joint or the ball-and-socket joint in the shoulder.
- The skin on the lower two-thirds of the deltoid muscle through the superior lateral cutaneous branch.
Injuries and Conditions
Problems with the axillary nerve can be caused by injuries anywhere along the arm and shoulder and by disease. Common injuries include:
Dislocations
- Of the shoulder joint, which can cause axillary nerve palsy.
Fracture
- Of the surgical neck of the humerus.
Compression
- This stems from walking with crutches, also known as crutch palsy.
Direct Trauma
- This can be from an impact sports, work, automobile accident, collision, or laceration.
Added Pressure
- This can be from wearing a cast or splint.
Surgical Accidental Injury
- An injury or damage can come from shoulder surgery, especially arthroscopic surgery on the inferior glenoid and capsule.
Quadrangular Space Syndrome
- This is where the axillary nerve is compressed where it passes through that space, which is most common in athletes who perform frequent overhead motions)
Nerve Root Damage
- Between the fifth and sixth cervical vertebrae, where the nerve emerges from the spinal cord, which can be caused by traction, compression, spinal disc prolapse, or a bulging disc.
Systemic Neurological Disorders
- Example – multiple sclerosis
Erb’s Palsy
- A condition often is the result of a birth injury called shoulder dystocia, in which a baby’s shoulder/s becomes stuck during childbirth.
Axillary Nerve Palsy
- Damage can result in a type of peripheral neuropathy that can cause weakness in the deltoid and teres minor muscles.
- This can result in losing the ability to lift the arm away from the body and weakness in various shoulder movements.
- If the damage is severe enough, it can cause paralysis of the deltoid and other minor muscles, resulting in flat shoulder deformity, in which individuals cannot lay their shoulders flat when lying down.
- Axillary nerve damage also can lead to a change, reduction, or loss of sensation in a small part of the arm just below the shoulder.
Nerve Injury Statistics
- Three times more common in men than women.
- It may be present in as many as 65% of shoulder injuries.
- The risk of injury due to dislocation is significantly increased after age 50.
Tests
If a healthcare provider suspects a problem with axillary nerve function, they’ll test the shoulder’s range of motion and skin sensitivity. A difference in the range of motion between the shoulders can indicate a nerve injury. Individuals may be sent for electromyography and a nerve conduction study to verify nerve palsy. In some cases, an MRI and/or X-rays may be ordered, especially if the cause of possible nerve damage is unknown.
Rehabilitation
Depending on the severity and cause of the injury, non-surgical treatments may be recommended, with surgery as a last resort. Non-surgical treatment can include some combination of immobilization, rest, ice, physical therapy, and anti-inflammatory meds. Physical treatment typically lasts about six weeks and focuses on strengthening and stimulating the muscles to prevent joint stiffness, which can impair long-term function.
Surgery
If conservative treatments don’t work, surgery may be recommended, especially if several months have passed without improvement. Surgical outcomes are generally better if surgery is performed within six months of the injury, and regardless of the time frame, the prognosis is considered positive in about 90% of cases. Surgical procedures performed for axillary nerve dysfunction or injury include:
Neurolysis
- This procedure involves targeted damage/degeneration of nerve fibers, interrupts the nerve signals, and eliminates pain while the damaged area heals.
Neurorrhaphy
- This procedure stitches a severed nerve back together.
Nerve Grafting
- Grafting involves transplanting a portion of another nerve, usually the sural nerve, to reconnect severed nerves.
- This helps, especially when the damaged portion is too large to be repaired by neurorrhaphy.
- It allows a pathway for signals and encourages the regrowth of nerve axons.
Neurotization or Nerve Transfer
- Similar to grafting but used when the nerve is too damaged to heal.
- This procedure involves transplanting a healthy but less important nerve, or a portion of a nerve, to replace the damaged one and restore function.
Injury Medical Chiropractic and Functional Medicine Clinic
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues.
Shoulder Pain Chiropractic Treatment
References
Subasinghe, S. K., & Goonewardene, S. (2016). A Rare Variation of the Axillary Nerve Formed as Direct Branch of the Upper Trunk. Journal of clinical and diagnostic research : JCDR, 10(8), ND01–ND2. https://doi.org/10.7860/JCDR/2016/20048.8255
Pizzo, R. A., Lynch, J., Adams, D. M., Yoon, R. S., & Liporace, F. A. (2019). Unusual anatomic variant of the axillary nerve challenging the deltopectoral approach to the shoulder: a case report. Patient safety in surgery, 13, 9. https://doi.org/10.1186/s13037-019-0189-1
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


