Sciatica is a prevalent and painful issue. Keeping it in check can be difficult, especially with various causes that can generate flare-ups. Individuals managing sciatica must pay attention and be vigilant of the negative activities/movements that could cause symptoms to reappear. A few common causes include:
- Excessively tight-fitting pants
- Improperly lifting heavy objects
- Poor posture
- Weight gain
- Not stretching out
- Wearing the wrong shoes
Knowing what not to do is just as effective for helping sciatica flare-ups as knowing what is best.

Table of Contents
Sciatica Causes
The sciatic nerve is the longest nerve. It comes out the spine through the pelvis, down the leg to the foot. One sciatic nerve on each side of the body can either become irritated, injured, or inflamed. However, both are rarely irritated at the same time. The underlying causes can vary. Most of the time, the cause is a herniated disc that presses against the nerve, causing the pain. Even though this happens in the lower back, an individual might only feel pain in the buttocks and the back of the leg. Other causes of sciatic nerve pain include:
- Bone spurs
- Degenerative disc disease
- Muscle inflammation
- Muscle spasms
- Spinal stenosis
- Spondylolysis
Making Sciatica Flare-ups Worse
What makes sciatica worse depends on the underlying cause. For most, this is a herniated or bulging disc that presses against the nerve. Any increased pressure on the discs can worsen the symptoms in this type of case. Sitting down puts more pressure on the spinal discs, worsening the pain. Lying down can also worsen symptoms. When the pain is peaking, lying down for a little while can help, but too long can worsen symptoms. Standing with a neutral spine and walking around a bit can help with nerve pain relief and healing.

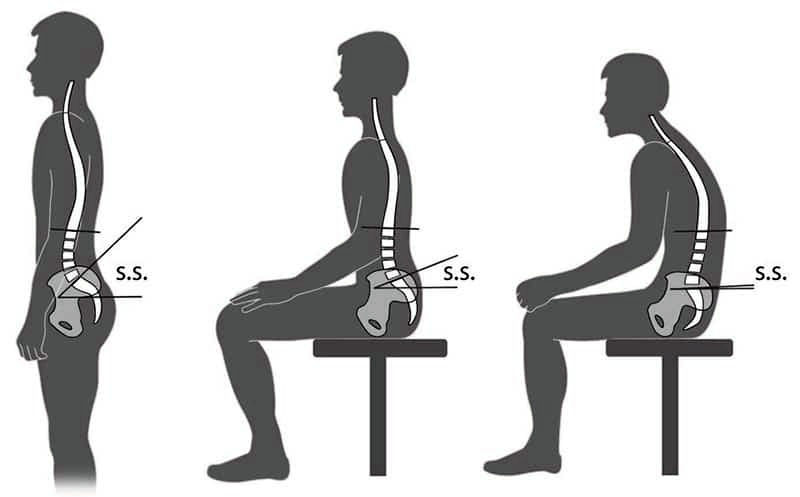
Improper/Poor Posture
Poor posture, especially the rounding of the lower back. This usually happens when sitting. The rounded low back becomes a bad habit that individuals think will help with the pain. This can cause a flare-up. The spine has a natural S-curve; the more an individual can maintain that natural curve, the better off they will be.
Weight Gain
Too much weight can cause flare-ups with added stress/pressure on the spine, especially the low back. Maintaining a healthy weight will help relieve the added pressure; however, many who experience sciatica have trouble exercising. This is where a physical therapist and chiropractor can assist an individual with customized exercise and diet programs to overcome this obstacle. Eating is a way that individuals deal with pain, anxiety, and depression. But weight gain and poor health can worsen sciatica. Overweight individuals experience more inflammation throughout the body, making sciatica even worse.
Stretching
Not stretching, especially as the body ages, tightens the muscles, ligaments, and tendons. And stretching improperly can injure these areas. There are recommended and non-recommended stretches for individuals dealing with/managing sciatica. Stretches that require bending the low back can place added pressure on the lumbar spine, causing sciatica flare-ups.

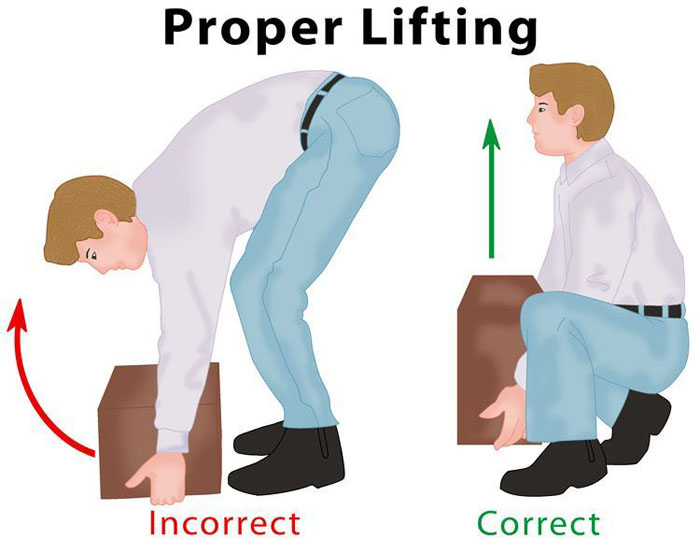
Lifting Heavy Things
Lifting and improperly lifting heavy objects can worsen sciatica. This has to do with the rounding of the low back. Any time the spine is taken out of its natural S-curve, there is undue pressure on the joints and discs. When lifting heavy objects in this position, the problem is worsened. When possible, avoid lifting anything heavy while dealing with sciatica. It’s healthy to stay active, but there is no need to do intense workouts at home or the gym, especially heavy lifting.
Tight Pants
Tight pants can contribute to sciatica. Wear overly tight and form-fitting pants should be avoided in shorts, jeans, or skirts until the sciatica is gone. And even after, it is not recommended to wear overly tight-fitting clothing, as this can cause blood and nerve circulation problems.
Shoes
Like tight pants, the wrong shoes without adequate support can cause flare-ups. For example, high heels distribute weight to the front of the feet. For the body to compensate, pushing the pelvis and hips forward is normal. When the body is in this position for a long time, it starts to place stress on the hamstrings, which will exacerbate sciatica. Shoes without adequate support place added stress on the feet, which gets transferred up the leg to the hamstrings. Customized shoe inserts designed especially for individuals with sciatica can help prevent symptoms.
Improvement
Sciatica takes time to heal. Avoiding making it worse and taking all the steps to help it heal can bring the body back to normal within 2 weeks. For most, it takes around 4 weeks for the pain to go away. This depends on various factors. For example, if sciatica develops during pregnancy, it could take longer to get rid of the pain. One sign that shows improvement is called centralization, meaning the pain is moving out of the leg and into the spine. This is a good sign that the individual is on the right track.
Body Composition
Meal Planning
The convenience of food delivery is wonderful, but remember that frequently eating food prepared away from home increases the risk of weight gain and obesity. Restaurants tend to serve oversized portions and prepare meals with excessive calories, sodium, and sugar. The benefit of eating from home is that individuals have more control over the ingredients and cooking methods used to prepare the food. It helps plan meals and snacks to ensure they are balanced. Here are the types of foods that should be included in a balanced meal plan:
- A variety of whole fruits
- Non-starchy vegetables – leafy greens, red and orange veggies
- Starchy vegetables – potatoes, green peas, legumes, winter squash
- Grains, with the goal to make at least ½ from whole-grain sources
- Low-fat or fat-free dairy milk, yogurt, cheese
- Protein from various sources – lean meats, seafood, eggs, nuts & seeds, and soy products
- Healthy cooking oils – olive oil or canola oil
- Nuts and nut butter
- Fresh or frozen fruits
- Dried herbs and spices
References
Sciatica. MedlinePlus. https://medlineplus.gov/sciatica.html. Accessed November 29, 2018.
Sciatica Sciatic Nerve Pain During Pregnancy. babyMed. https://www.babymed.com/pregnancy/sciatica-pain-during-pregnancy. Updated on August 29, 2018. Accessed November 29, 2018.
Shiel WC. Degenerative Disc Disease and Sciatica. MedicineNet. https://www.medicinenet.com/degenerative_disc/article.htm#what_are_the_symptoms_of_radiculopathy_and_sciatica. Last reviewed August 10, 2018. Accessed November 29, 2018.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


