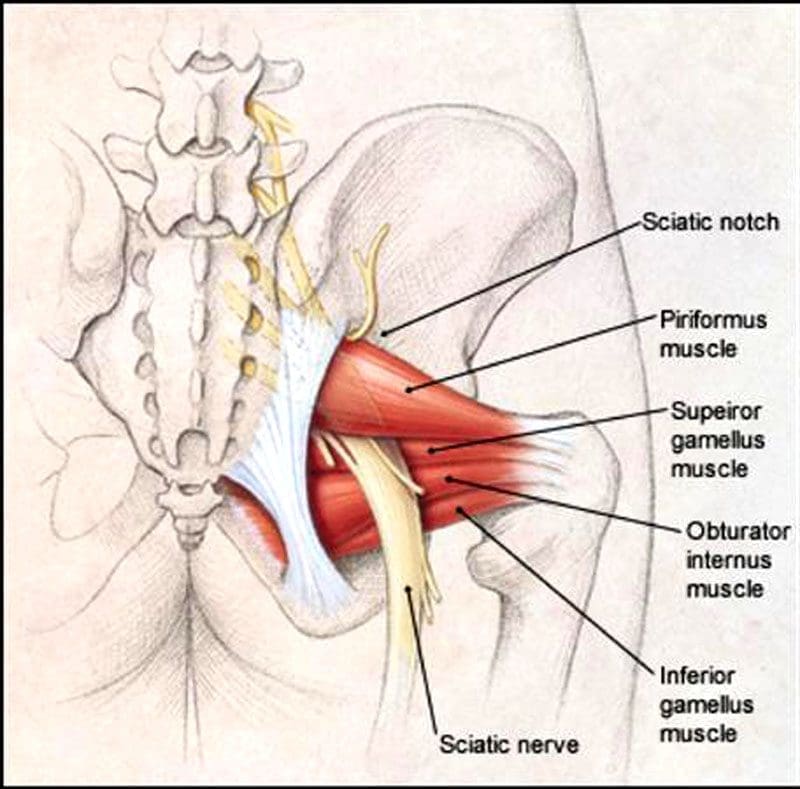
The piriformis is a large and powerful muscle beneath the gluteal/buttocks muscles. It runs from the bottom of the sacrum, where the base of the spine and pelvis converge to the top of the femur. This muscle plays a critical role in running motion; it helps externally rotate the hips and upper leg outward, provides hip flexibility and stability, and stabilizes the pelvis. The sciatic nerve passes next to, over, under, or through the piriformis muscle. When the piriformis contracts or spasms, it can irritate, become entangled and compress the nerve, resulting in painful symptoms. This can lead to various problems and is how piriformis syndrome occurs.
Table of Contents
Running Piriformis Syndrome
The proper function of the piriformis muscle is essential for athletes who participate in running sports. Repetitive activities, like running, can fatigue the muscle and irritate and inflame the nerve.
Symptoms
Piriformis syndrome can be challenging to diagnose because it can be confused for a herniated disc, sciatica, a proximal hamstring strain/high hamstring tendinitis, or lower back problems. A few symptoms that can help determine whether the piriformis is the cause include:
Sitting, Stairs, Squatting Discomfort or Pain
- Individuals don’t always experience discomfort while running.
- Instead, it’s sitting, climbing stairs, and squatting where pain symptoms present.
- Pain while running, specifically an overstretched sensation when going up a hill or increasing speed, is more associated with a proximal hamstring strain.
Tenderness
- The area around the piriformis is tender.
- Applying pressure can cause discomfort or pain around the area and radiate down the leg.
Centered Pain
- Piriformis syndrome is usually felt in the middle of the glutes.
- A proximal hamstring strain typically causes non-radiating pain at the bottom of the glutes, where the hamstrings connect to the pelvis.
Causes
- Pelvic misalignment.
- Pelvic misalignments created by other conditions, like a tilted pelvis, functional leg-length discrepancy, or practicing unhealthy posture, make the piriformis work harder to compensate, which leads to tightness and/or spasms.
- Sudden increases in distance or workout intensity can worsen any weakness in the piriformis and other gluteal muscles.
- Continuing to run, which is possible, can worsen and prolong the condition.
- When running, the muscle’s signal transmissions are interrupted by inflammation and/or compression and cannot synchronize with each other.
- The result is the inability to withstand the repetitive strain of running.
- Not warming up with glute-activation exercises increases the risk of running piriformis syndrome.
Chiropractic Treatment
Resting may not be enough to alleviate piriformis syndrome. This is especially true if the problem involves spine and pelvic misalignment. Chiropractic can provide significant relief from running piriformis syndrome. A combination of spinal, pelvic, and extremity adjustments, therapeutic massage, MET, decompression, stretches, and anti-inflammatory nutrition will take the pressure off overly tight areas, realign the body, and maintain nervous system function.
- Running form could be evaluated and checked for leg-length discrepancies and muscle-strength imbalances.
- Running can continue if the individual can do so without pain or symptoms.
- But it is recommended to avoid slanted surfaces, which increase the risk of pelvic misalignment.
- Avoid long runs, which increase the chance of overload and fatigue.
- The goal is to relax and release the piriformis.
- If it’s impinging on the sciatic nerve, loosening and releasing the muscle will significantly lessen radiating pain.
- Orthotics may be recommended for excessive overpronation or inward movement of the foot when landing.
Other treatments to stop piriformis spasms.
- Ice and take over-the-counter anti-inflammatory medications can be used during acute phases when the area is tender.
- Work out tight spots using a foam roller or percussive massager.
- Stretching and loosening the muscle before and after runs can help it relax and increase blood flow.
- Stretches like pigeon pose and standing figure four and exercises like side planks with a leg lift are recommended.
Building a Stronger Body
References
Ahmad Siraj, Sidra, and Ragini Dadgal. “Physiotherapy for Piriformis Syndrome Using Sciatic Nerve Mobilization and Piriformis Release.” Cureus vol. 14,12 e32952. 26 Dec. 2022, doi:10.7759/cureus.32952
Chang A, Ly N, Varacallo M. Piriformis Injection. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Heiderscheit, Bryan, and Shane McClinton. “Evaluation and Management of Hip and Pelvis Injuries.” Physical Medicine and rehabilitation clinics of North America vol. 27,1 (2016): 1-29. doi:10.1016/j.pmr.2015.08.003
Julsrud, M E. “Piriformis syndrome.” Journal of the American Podiatric Medical Association vol. 79,3 (1989): 128-31. doi:10.7547/87507315-79-3-128
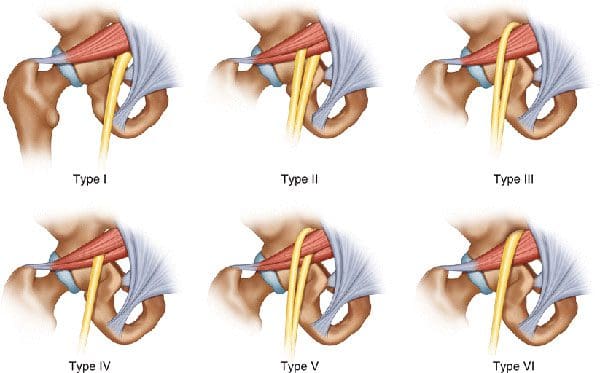
Kraus, Emily, et al. “Piriformis Syndrome With Variant Sciatic Nerve Anatomy: A Case Report.” PM & R: the Journal of Injury, Function, and Rehabilitation vol. 8,2 (2016): 176-9. doi:10.1016/j.pmrj.2015.09.005
Lenhart, Rachel, et al. “Hip muscle loads during running at various step rates.” The Journal of Orthopedic and sports physical therapy vol. 44,10 (2014): 766-74, A1-4. doi:10.2519/jospt.2014.5575
Sulowska-Daszyk, Iwona, and Agnieszka Skiba. “The Influence of Self-Myofascial Release on Muscle Flexibility in Long-Distance Runners.” International Journal of environmental research and public health vol. 19,1 457. Jan 1, 2022, doi:10.3390/ijerph19010457
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card