Can individuals find therapeutic ways to reduce restless leg syndrome and improve their sleep quality in their beds?
Table of Contents
What Is Restless Leg Syndrome?
Do you feel general aches or leg pain, causing you to feel restless? Do you experience fatigue throughout the day, making it difficult to fall asleep? Or do you feel uncomfortable sensations in your legs, making falling and staying asleep difficult? Many people worldwide have experienced these issues known as restless leg syndrome. Also known as Willis-Ekbom disease, restless leg syndrome is often characterized by an uncomfortable urge to move legs when a person rests for the night and can be accompanied by unpleasant sensations that cause irresistible restlessness. (Gossard et al., 2021) Restless leg syndrome (RLS) can also be primary or secondary depending on the severity of the issue affecting the individual’s legs. Since the legs allow the individual to be mobile through walking, running, and jumping, the various muscles and tendons that make up the legs can succumb to RLS. As it is a chronic movement disorder, it is common to many individuals. It is associated with abnormal, non-painful sensations that are active when a person rests and relieved when they are in motion. (Mansur et al., 2025) We associate with certified medical providers who inform our patients of how restless leg syndrome affects their legs. While asking important questions to our associated medical providers, we advise patients to incorporate ways to reduce restless leg syndrome and restore their sleep quality. Dr. Alex Jimenez, D.C., envisions this information as an academic service. Disclaimer.
Causes
What causes individuals to develop RLS can often be correlated with environmental factors. Additionally, since RLS can be primary or secondary, the overlapping risk profiles also play a factor. Environmental factors like stress and anxiety can cause the central nervous system to go haywire, causing the sensations to set off and become worse. When RLS is primary, the central nervous system can cause the legs to develop RLS by not getting enough dopamine, which is a neurotransmitter that regulates body movement. The RLS symptoms can worsen when there isn’t enough dopamine in the body. When RLS is secondary, it could be due to iron deficiency that the brain areas have low levels of iron being transported to the blood-brain barrier and not being imported to the neuronal cells. (Vlasie et al., 2022) This can cause numerous symptoms and affect the legs when a person is trying to get a good night’s rest.
Symptoms
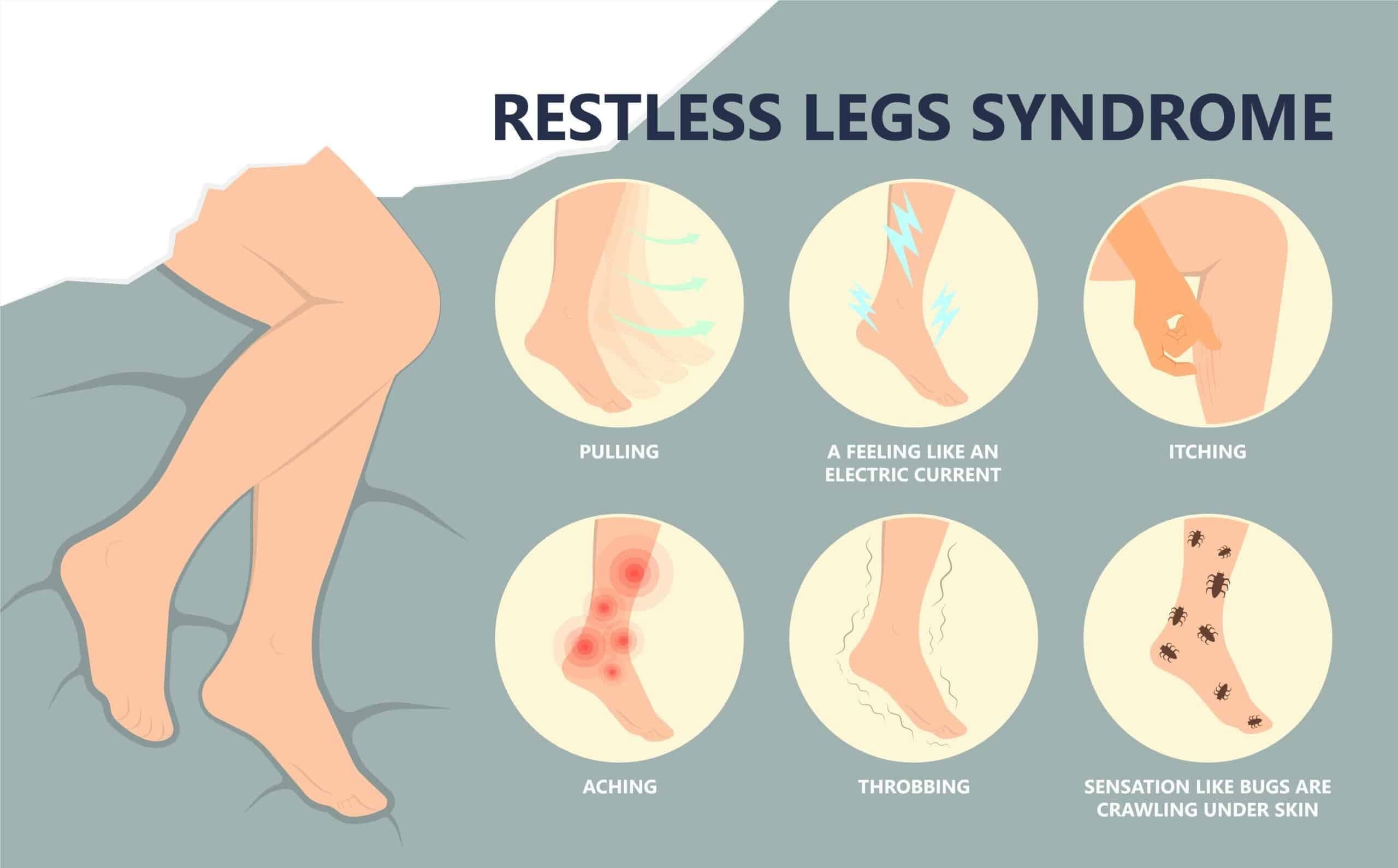
Some of the symptoms associated with RLS can affect the circadian rhythm, which can cause the central nervous system to sensitize and hyperarousal, leading to sensory disturbances and frequent awakening periods. (Tang et al., 2023) Other symptoms include:
- Crawling/ Itching sensations
- Fatigue
- Mood changes
- Difficulty concentrating
- Sleep disruptions
Peripheral Neuropathy & Chiropractic Care-Video
Ways To Reduce Restless Leg Syndrome
When it comes to reducing restless leg syndrome, many people can find ways to minimize the comorbidities associated with RLS. Many people can sleep with the right mattress and pillows that can help provide them with a restful night. Others may try exercising or meditation to reduce the everyday stress that is affecting them. These small changes can help many people develop healthy sleeping habits that improve sleep quality and incorporate a proper sleeping routine. (Taximaimaiti et al., 2021)
Vitamins & Supplements
Incorporating iron supplements to reduce the effects of restless leg syndrome by replenishing the neurons and cells in the central nervous system. (Elstrott et al., 2020) Combined with magnesium, this can help lower the intensity of the RLS symptoms and even improve sleep quality. (Jadidi et al., 2022) Ask the doctor which iron supplement the body is low on before buying.
Massage
Incorporating massages as part of a routine to reduce restless leg syndrome can benefit the body. Massage therapists can work on the muscles in the lower extremities to manipulate the soft tissues while strengthening the immune system. Massages like reflexology, Swedish, and deep tissue can help reduce stress and anxiety, relieve leg fatigue, improve blood circulation, and reduce sleep disturbances. (Ghanbari et al., 2022)
Conclusion
Incorporating these various techniques and remedies to reduce restless leg syndrome can improve the body and increase sleep quality. Making small changes to these everyday stressors can reduce the chances of restless leg syndrome returning.
References
Elstrott, B., Khan, L., Olson, S., Raghunathan, V., DeLoughery, T., & Shatzel, J. J. (2020). The role of iron repletion in adult iron deficiency anemia and other diseases. Eur J Haematol, 104(3), 153-161. https://doi.org/10.1111/ejh.13345
Ghanbari, A., Shahrbabaki, P. M., Dehghan, M., Mardanparvar, H., Abadi, E. K. D., Emami, A., & Sarikhani-Khorrami, E. (2022). Comparison of the Effect of Reflexology and Swedish Massage on Restless Legs Syndrome and Sleep Quality in Patients Undergoing Hemodialysis: a Randomized Clinical Trial. Int J Ther Massage Bodywork, 15(2), 1-13. https://doi.org/10.3822/ijtmb.v15i2.705
Gossard, T. R., Trotti, L. M., Videnovic, A., & St Louis, E. K. (2021). Restless Legs Syndrome: Contemporary Diagnosis and Treatment. Neurotherapeutics, 18(1), 140-155. https://doi.org/10.1007/s13311-021-01019-4
Jadidi, A., Rezaei Ashtiani, A., Khanmohamadi Hezaveh, A., & Aghaepour, S. M. (2022). Therapeutic effects of magnesium and vitamin B6 in alleviating the symptoms of restless legs syndrome: a randomized controlled clinical trial. BMC Complement Med Ther, 23(1), 1. https://doi.org/10.1186/s12906-022-03814-8
Mansur, A., Castillo, P. R., Rocha Cabrero, F., & Bokhari, S. R. A. (2025). Restless Legs Syndrome. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/28613628
Tang, M., Sun, Q., Zhang, Y., Li, H., Wang, D., Wang, Y., & Wang, Z. (2023). Circadian rhythm in restless legs syndrome. Front Neurol, 14, 1105463. https://doi.org/10.3389/fneur.2023.1105463
Taximaimaiti, R., Luo, X., & Wang, X. P. (2021). Pharmacological and Non-pharmacological Treatments of Sleep Disorders in Parkinson’s Disease. Curr Neuropharmacol, 19(12), 2233-2249. https://doi.org/10.2174/1570159X19666210517115706
Vlasie, A., Trifu, S. C., Lupuleac, C., Kohn, B., & Cristea, M. B. (2022). Restless legs syndrome: An overview of pathophysiology, comorbidities and therapeutic approaches (Review). Exp Ther Med, 23(2), 185. https://doi.org/10.3892/etm.2021.11108
Disclaimer
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card