Herniated discs are a debilitating condition characterized by pain, numbness and weakness in one or more limbs. While some people may experience no pain at all, those that do may often wish for fast pain relief to avoid long periods of sick leave from their jobs. Many healthcare professionals recommend surgery for patients with persistent and/or worsening herniated disc symptoms but other non-operative treatment options can help treat disc herniations. The purpose of the following article is to demonstrate how a structured physiotherapy treatment model can provide rapid relief to patients who qualify for lumbar disc surgery.
Table of Contents
A Structured Physiotherapy Treatment Model Can Provide Rapid Relief to Patients Who Qualify for Lumbar Disc Surgery: A Prospective Cohort Study
Abstract
- Objective: To evaluate a structured physiotherapy treatment model in patients who qualify for lumbar disc surgery.
- Design: A prospective cohort study.
- Patients: Forty-one patients with lumbar disc herniation, diagnosed by clinical assessments and magnetic resonance imaging.
- Methods: Patients followed a structured physiotherapy treatment model, including Mechanical Diagnosis and Therapy (MDT), together with graded trunk stabilization training. Study outcome measures were the Oswestry Disability Index, a visual analogue scale for leg and back pain, the Tampa Scale for Kinesiophobia, the European Quality of Life in 5 Dimensions Questionnaires, the Zung Self-Rating Depression Scale, the Self-Efficacy Scale, work status, and patient satisfaction with treatment. Questionnaires were distributed before treatment and at 3-, 12- and 24-month follow-ups.
- Results: The patients had already improved significantly (p<0.001) 3 months after the structured physiotherapy treatment model in all assessments: disability, leg and back pain, kinesiophobia, health-related quality of life, depression and self-efficacy. The improvement could still be seen at the 2-year follow-up.
- Conclusion: This study recommends adopting the structured physiotherapy treatment model before considering surgery for patients with symptoms such as pain and disability due to lumbar disc herniation.
- Keywords: intervertebral disc displacement; rehabilitation; physical therapy modalities.
Introduction
Symptoms of lumbar disc herniation are relatively common in the general population, although the prevalence rates vary widely between different studies (1). Symptom severity also varies and, in many patients, pain and loss of function may lead to disability and long periods of sick leave (2). Spontaneous resolution of symptoms after a lumbar disc herniation is regarded as common, which makes it difficult to evaluate the effects of treatment. Furthermore, in studies evaluating spontaneous healing, different physiotherapy treatments are often included, together with pain medication (3–5), which makes it difficult to determine the extent of natural healing. On the other hand, in patients with sciatica, but without confirmed disc herniation on magnetic resonance imaging (MRI), approximately one-third of subjects recover 2 weeks after the onset of sciatica and approximately three-quarters recover after 3 months (6).
In contrast to evaluating spontaneous healing, surgery for lumbar disc herniation has been investigated in numerous studies. Surgery has been compared with a variety of treatments, such as education, chiropractic, unspecified physiotherapy, acupuncture, injections and medication (7–10). The non-surgical treatments have, however, been described only in vague terms, and variations in treatments have been used. Previous studies have reported favourable short-term (after 1 year) outcomes for surgery, but no major differences between surgical and other treatments have been demonstrated in the long term (over 2 years) (7, 10, 11). The conclusions that are drawn from the comparison between surgery and non-systematic non-surgical treatments may thus be misleading. This has been confirmed in a systematic review, which concluded that there is conflicting evidence as to whether surgery is more beneficial than nonsurgical care for both short- and long-term follow-up (12).
Kinesiophobia has been evaluated in patients after lumbar disc surgery, and almost 50% of patients were classified as having kinesiophobia (13). To our knowledge kinesiophobia has not been evaluated in patients with lumbar disc herniation treated with a structured physiotherapy treatment.
There are many different non-surgical treatment methods for patients with low-back pain and sciatica. One common management method is Mechanical Diagnosis and Therapy (MDT), also known as the McKenzie method, which aims to eliminate or minimize pain (14). A systematic review from 2004 of the efficacy of MDT showed that patients with low-back pain treated with MDT reported a greater, more rapid reduction in pain and disability compared with non-steroidal anti-inflammatory drugs (NSAIDs), educational booklets, back massage and back care advice, strength training, spinal mobilization and general exercises (15). In a randomized controlled trial with a 1-year follow-up from 2008, Paatelma and co-workers (16) found that the McKenzie method was only marginally more effective compared with only giving advice to patients with low-back pain. For patients with low-back pain, sciatica and a verified lumbar disc herniation, it has, however, been shown that a selected group of patients who responded to MDT after 5 days of treatment also reported that they were satisfied after 55 weeks (17). The patients started treatment just 12 days after the onset of symptoms and the effects of spontaneous healing cannot therefore be excluded. Taken together, the treatment effects of MDT for patients with a verified lumbar disc herniation appear to require further evaluation.
Trunk stabilization exercises, which aim to restore deep trunk muscle control, have been used for the prevention and rehabilitation of low-back pain (18). A randomized controlled trial revealed a reduction in the recurrence of low-back pain episodes after specific trunk stabilization exercises compared with a control group receiving advice and the use of medication (19). Dynamic lumbar stabilization exercises have been found to relieve pain and improve function in patients who have undergone microdiscectomy (20). The effects of trunk stabilization exercises combined with MDT have, however, not been studied in patients with non-operated lumbar disc herniation. MDT is seldom recommended for patients with MRI verified lumbar disc herniation with a broken outer annulus. At our hospital, however, we have several years of good clinical experience of a combination of MDT and trunk stabilization exercises for this category of patients. To our knowledge, no previous study has investigated whether patients with a lumbar disc herniation verified by MRI, symptoms for at least 6 weeks (minimizing effects of spontaneous healing) and who qualified for disc surgery could improve with a structured physiotherapy treatment model including MDT and gradually progressive trunk stabilization exercises. The aim of this study was therefore to evaluate a structured physiotherapy treatment model in patients who qualified for lumbar disc surgery.
Material and Methods
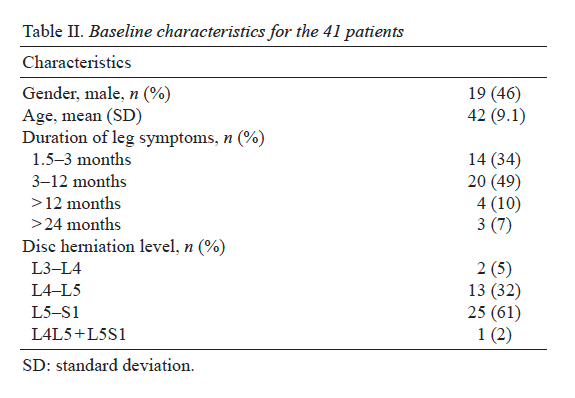
During the study inclusion period, 150 patients, who were referred to the orthopaedic clinic at Sahlgrenska University Hospital, Gothenburg, from November 2003 to January 2008, were identified as potential participants since disc herniation was confirmed with MRI. Inclusion criteria were: 18–65 years of age; MRI confirming disc herniation explaining the clinical findings; symptoms for at least 6 weeks (minimizing the effects of spontaneous healing) and pain distribution with concomitant neurological disturbances correlated to the affected nerve root. Exclusion criteria were: cauda equina syndrome, previous spinal surgery, other spinal diseases, such as spinal stenosis and spondylolisthesis, and inadequate command of Swedish. However, 70 patients were excluded because of spontaneous resolution of pain and symptoms. The remaining 80 patients met the inclusion criteria and qualified for surgery. Orthopaedic surgeons determined whether the patients qualified for lumbar disc surgery after MRI and physical examination according to the recommendations of the American Academy of Orthopaedic Surgeons for patients with lumbar disc herniation (21).
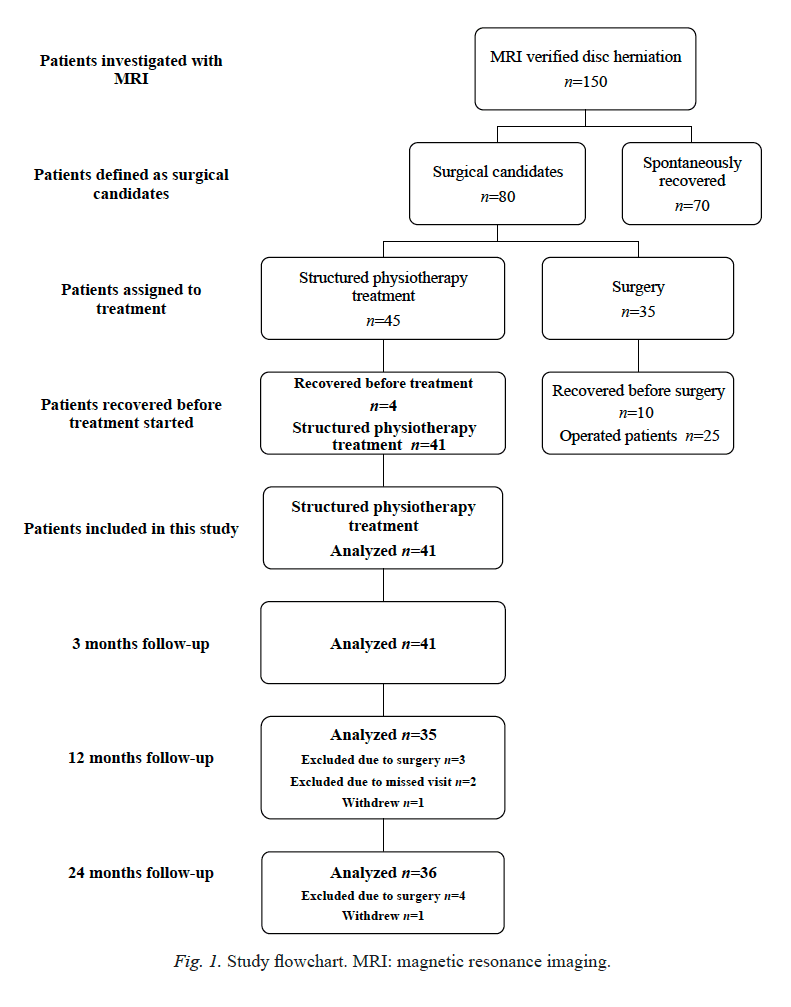
Initially, the study was planned as a randomized controlled trial (RCT) between a structured physiotherapy treatment model and surgery, but the number of patients was not sufficient to obtain acceptable power. Eighteen of the 80 patients were initially randomized to physiotherapy, 17 patients were randomized to surgery and 45 patients did not agree to undergo randomization. Twenty-seven of the 45 patients who did not agree to randomization agreed to take part in the structured physiotherapy treatment and 18 patients agreed to undergo surgery. A decision was therefore made solely to present a cohort of 45 patients treated according to the structured physiotherapytreatment protocol (Fig. 1). Patients were given verbal and written information and informed consent was obtained. The study was approved by the Regional Ethical Review Board.
Before structured physiotherapy treatment began, 4 patients recovered to the extent that they could no longer be accepted as surgical candidates and they were therefore excluded from the study. The remaining 41 patients treated according to the structured physiotherapy model are presented in this paper.
A Structured Physiotherapy Treatment Model
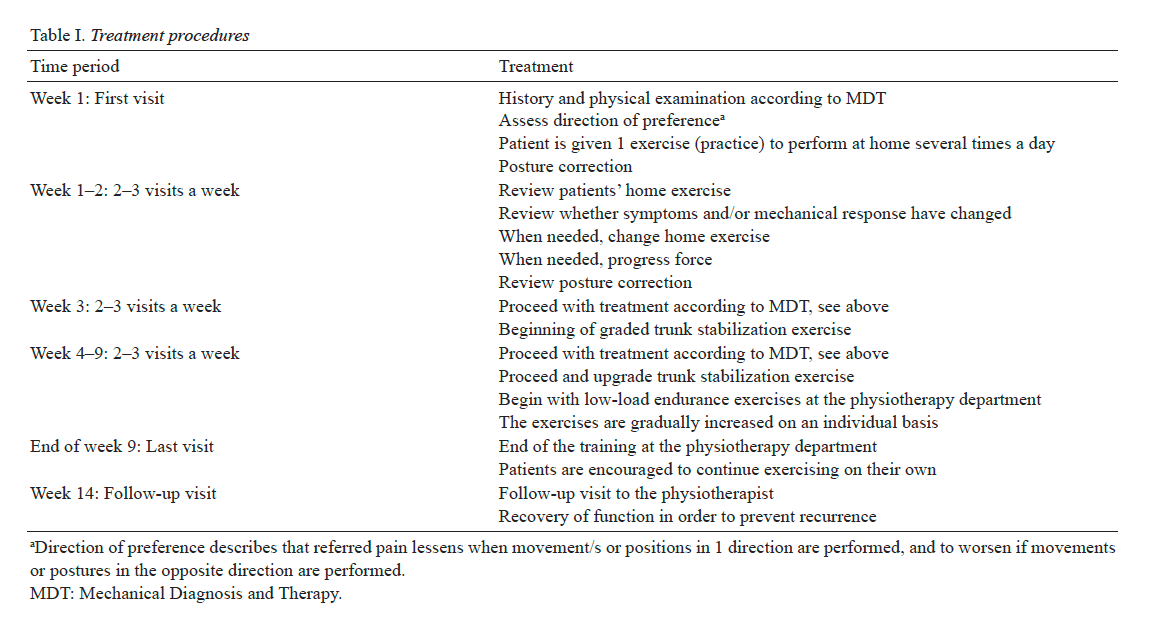
Six physiotherapists with credentialed examinations in MDT, which is an examination within the MDT concept after completing 4 courses of 4 days each for evaluating and treating patients with spinal problems. Following completion of these courses, an extensive literature study and practice in evaluating and treating patients is required before the examination can be completed. The physiotherapists involved in the study had 5–20 years of clinical experience of treating patients with back problems and herniated lumbar disc. The inter-examiner reliability of the MDT assessment has been shown to be good if the examiner is trained in the MDT method (22). The physiotherapists examined and treated the patients during a 9-week period (Table I). For the first 2 weeks of treatment, an MDT protocol was followed, based on clinical examinations of individual mechanical and symptomatic responses to positions and movements, with the aim of minimizing pain and with the emphasis on self-management (14). During the third week of treatment, graded trunk stabilization exercises were added to the MDT protocol. The purpose of graded trunk stabilization exercises was to improve muscle control (23). The low-load muscular endurance exercises were gradually increased in intensity on an individual basis with respect to the patients’ reported leg pain and the observed movement control and quality. During treatment, the patients were encouraged to continue exercising on their own at a gym, or to perform some other type of physical training of their own choice after the structured physiotherapy treatment was concluded. Four weeks after the completion of the 9-week physiotherapy treatment period, the patients attended a follow-up visit with the physiotherapist who had treated them. The aim of this visit was to encourage a high level of compliance with respect to continued trunk stabilization exercises and MDT practice (Table I).
Study Outcome Measures
The patients were given a battery of questionnaires to complete. Independent examiners, who were not involved in the treatment, distributed the questionnaires before treatment (baseline) and at the 3-, 12- and 24-month follow-ups.
The primary outcome measures were pain intensity in the leg, rated using a visual analogue scale (VAS) 0–100 mm (24) and the Oswestry Disability Index (ODI) 0–100 % (25). A score of 0–10 mm on the VAS was defined as no pain according to Öberg et al. (26). An ODI score of 0–20% was defined as minimal or no disability, and a score of over 40% was defined as severe disability (25). These primary outcome measures are commonly used in evaluations after surgery for lowback pain and for assessing patients with lumbar disc herniation (27).
Secondary outcome measures included pain intensity in the back rated using a VAS and the degree of kinesiophobia using the Tampa Scale for Kinesiophobia (TSK). The TSK score varies between 17 and 68 and a cut-off more than 37 was defined as a high degree of kinesiophobia (28). Health-Related Quality of Life (HRQoL) in the European Quality of Life in 5 Dimensions Questionnaires (EQ-5D) was used. The EQ-5D includes 2 parts, EQ-5Dindex ranges from 0 to 1.0, where 1.0 is optimal health and EQ-5DVAS is a vertical visual analogue scale ranging from 0 (worst possible health state) to 100 (best possible health state) (29). The Zung Self-Rating Depression Scale (ZDS) ranges from 20–80 and the more depressed the patient is, the higher score (30). The Self-Efficacy Scale (SES) ranges from 8 to 64, with higher scores indicating more positive beliefs (31) was also used. Work status was measured using a 3-grade Likert scale: working full time, full-time sick leave and part-time sick leave. Likewise, patient satisfaction with treatment was measured on a 3-grade Likert scale; satisfied, less satisfied and dissatisfied (32). These secondary outcome measures evaluate bio-psychosocial factors described as important in connection with lumbar disc surgery (33).
Statistical Analyses
The results are presented as median values and interquartile range (IQR), except for age, which is presented as the mean and standard deviation (SD). Changes over time within the group were analysed with the Wilcoxon signed-rank test. Statistical significance was set at an alpha level of 0.05.
Results
The baseline characteristics are shown in Table II. No patient had undergone surgery at the 3-month follow-up. At the 12-month follow-up, 3 patients had undergone surgery and, at the 24-month follow-up, 1 additional patient had been operated on. After surgery, these 4 patients were excluded from further follow-ups (Fig. 1).
Change Over Time in Primary Outcome Measures
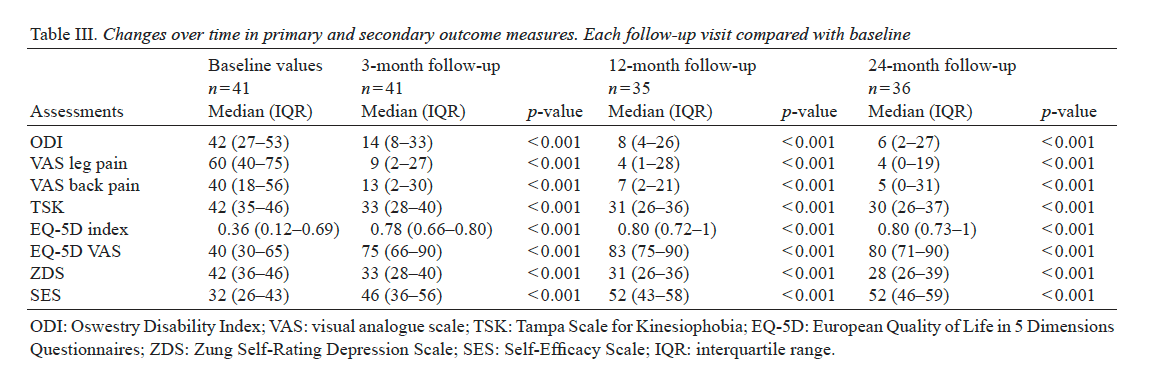
Disability. The patients showed significant improvements (p < 0.001) in ODI at the 3-month follow-up compared with baseline. The median (IQR) score decreased from 42 (27–53) to 14 (8–33). This improvement could still be seen at 12 and 24 months (Table III and Fig. 2). At baseline, 22 patients reported severe disability (54%) and 3 patients reported no disability. The degree of disability decreased at the 3-month follow-up, as only 9 patients (22%) reported severe disability and 26 (64%) reported no disability. At 12- and 24-month follow-ups only 2 patients (5%) reported severe disability. At 12-month followup 26 patients still reported no disability, and at 24-month follow-up 27 patients reported no disability.
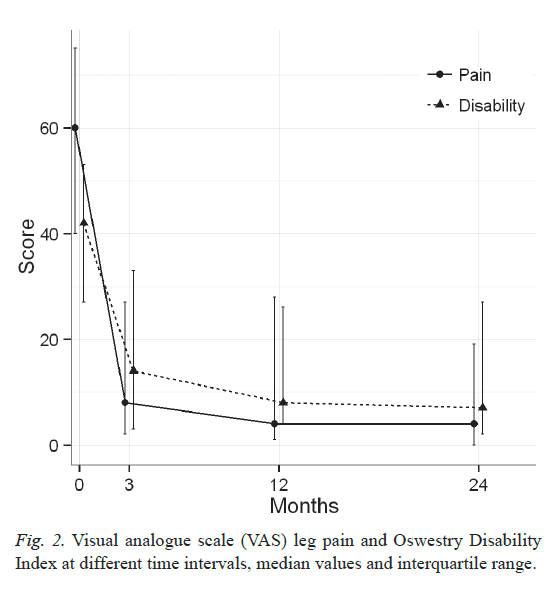
Leg pain. A significant reduction in patients’ leg pain was found at the 3-month follow-up (p < 0.001) on the VAS compared with baseline. The median (IQR) on the VAS decreased from 60 (40–75) to 9 (2–27). This improvement could still be seen at the 12- and 24-month follow-ups (Table III and Fig. 2). Before treatment, all patients reported leg pain. Three months after treatment, the median on the VAS was 9 mm, i.e. classified as no leg pain (26). Twenty-three patients (56%) reported no leg pain at the 3-month follow-up. At the 12-month follow-up 22 patients reported no leg pain, and after 24 months 24 patients reported no leg pain.
Change in Secondary Outcome Measures Over Time
Back pain. A significant improvement in back pain was found at the 3-month follow-up (p < 0.001) on the VAS compared with baseline. This improvement could still be seen at 12 and 24 months (Table III). At baseline, 6 patients (15%) reported no back pain. Three months after treatment began, 20 patients (49%) reported no back pain.
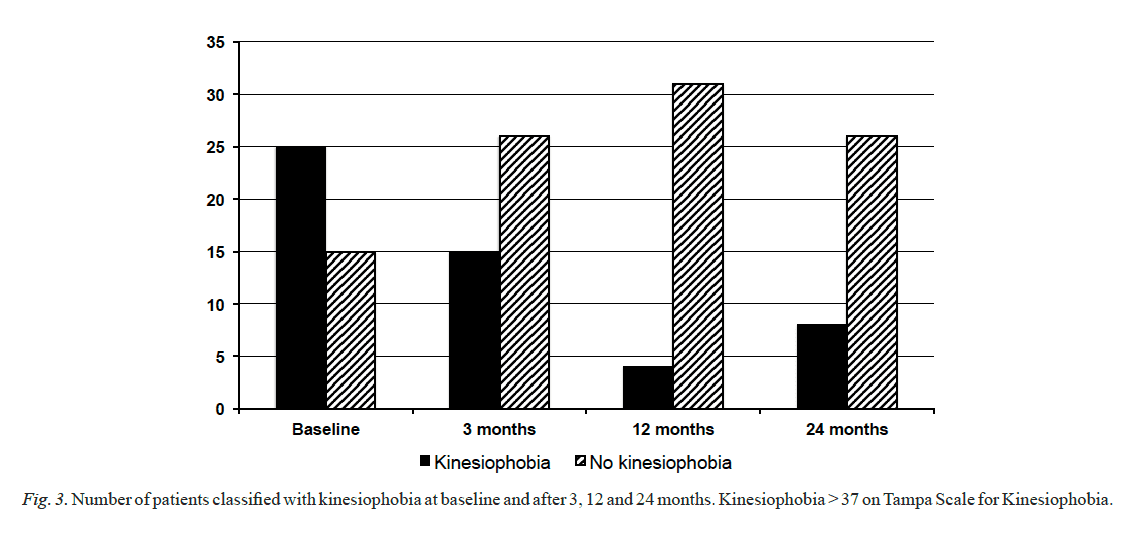
Kinesiophobia. The degree of kinesiophobia showed a significant improvement at the 3-month follow-up (p < 0.001) and the improvement could be seen throughout the follow-up period (Table III). Before treatment, 25 patients (61%) were classified as having kinesiophobia and 15 patients (37%) had no kinesiophobia, while data for 1 patient was missing. After 3 months, 15 patients (37%) had kinesiophobia and 26 (63%) had no kinesiophobia. At the 12-month follow-up, the number of patients with kinesiophobia had reduced to 4 (11%) (Fig. 3).
Health-related quality of life, depression and self-efficacy. All 4 assessments (EQ-5Dindex, EQ-5DVAS, ZDS and SES) showed significant improvements at the 3-month follow-up (p < 0.001). This improvement could still be seen at 12 and 24 months (Table III).
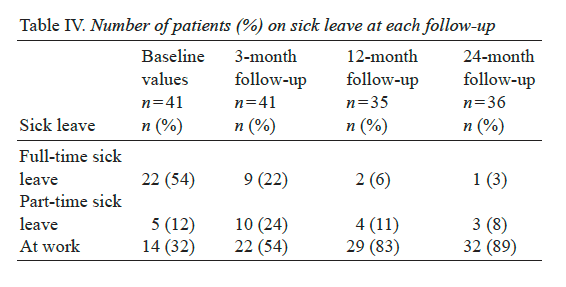
Sick leave. At baseline, 22 patients (54%) were on full-time sick leave (Table IV), compared with 9 (22%) patients at the 3-month follow-up. At baseline, 14 patients (34%) were working full time, compared with 22 (54%) at the 3-month follow-up.
Satisfaction with Treatment
At the 3-month follow-up, 32 (78%) of 41 patients were satisfied with the structured physiotherapy treatment. Seven patients were less satisfied and 2 patients were dissatisfied. Both of the dissatisfied patients were later operated. At the 2-year follow-up, the number of satisfied patients was 29 (80%) of 36. Seven patients were less satisfied, but none dissatisfied after structured physiotherapy treatment.
Dr. Alex Jimenez’s Insight
A disc herniation in the lumbar spine can cause pain, numbness and weakness in the lower back. Because of the severity of the symptoms, many patients seeking fast pain relief consider surgery. However, many non-operative treatment options can help improve as well as manage lumbar herniated disc symptoms. A structured physiotherapy treatment model can provide rapid pain relief to patients who would otherwise qualify for lumbar disc surgery, according to the following article. Patients looking to avoid taking long periods of sick leave from work due to their symptoms may benefit from a structured physiotherapy treatment model. As with any type of injury and/or condition, the use of other treatment options should be properly considered before turning to surgical interventions for fast pain relief.
Discussion
The principal finding of this study was that patients who qualified for lumbar disc surgery improved to a statistically significant and clinically substantial degree just 3 months after the start of the structured physiotherapy treatment in all assessments: disability, leg and back pain, kinesiophobia, health-related quality of life, depression and self-efficacy. The improvements could still be seen at the 2-year follow-up.
The natural course of healing must be considered carefully, especially when evaluating treatment effects in patients with disc herniation. The symptoms often vary over time and many discs heal spontaneously and the symptoms cease. Approximately 75% of patients with sciatica, without an MRI-verified disc herniation, recover within 3 months, and approximately one-third of patients recover within 2 weeks after the onset of sciatica (6). The natural course of sciatica was evaluated in a randomized controlled trial (34), which compared NSAIDs with placebo. The patients were, however, examined within 14 days after the onset of radiating leg pain. After 3 months, 60% of the patients had recovered and, after 12 months, 70% had recovered. In order to minimize the influence of spontaneous healing in the present study, the patients were therefore included only if they had had persistent pain and disability for more than 6 weeks. In fact, the majority of the patients had had pain and disability for more than 3 months. It is therefore most likely that the effects of treatment seen in the present study are, in the majority of patients, an effect of the structured physiotherapy treatment model and not a result of spontaneous healing.
In the study by Weber et al. (34), the VAS leg pain mean score was reduced from 54 mm at baseline to 19 mm within 4 weeks for all 183 patients, regardless of treatment. After 1 year, the VAS leg pain mean score was 17 mm. The patients in the present study who were a little worse at baseline (60 mm) reported 9 mm on the VAS leg pain just 3 months after treatment. Consequently, in the present study, the median VAS level had already been reduced to under the no-pain score, defined as 0–10 on the VAS (26), at the 3-month follow-up and this was maintained to the 12- and 24-month follow-ups.
Physiotherapy treatment for patients with lumbar disc herniation can lead to improvements. Brötz et al. (17) included a selected group of patients who responded with the centralization of pain after the first 5 daily sessions of treatment according to the MDT method. Centralization of pain is defined as a clinically induced change in the location of pain referred from the spine, that moves from the most distal position toward the lumbar midline (35). However, the patients’ medium duration of symptoms before treatment was only 12 days and the possibility that patients recovered naturally cannot therefore be excluded (17).
In a retrospective study, 95 patients were treated with a functional restoration programme (36). The patients achieved significant improvements after a mean treatment period of 8.7 months. The evaluation was performed at discharge only. With a treatment period of this length, it is, however, difficult to differentiate between the effects of treatment and the natural healing process. In the present study, a shorter treatment period was adopted, and large and significant improvements were found after just 3 months and were still present at the 24-month follow-up. It is therefore not likely that the natural healing process was responsible for the positive results in the present study.
In a prospective study of 82 consecutive patients with acute severe sciatica, included for conservative management, only a minority of the patients had made a full recovery after 12 months (37). Twenty-five percent of the patients underwent surgery within 4 months and one-third had surgery within 1 year. In spite of the fact that the inclusion criteria in the present study followed the recommendations for surgery (21, 38), no patient required surgery at the 3-month follow-up and, after 12 months, only 3 patients (7%) had undergone surgery. The interpretation of the divergence could be that the structured physiotherapy treatment model used in the present study appeared to influence patients with lumbar disc herniation in a very positive direction. One recommendation is therefore to follow the structured physiotherapy treatment model before considering surgery.
In this study, MRI verification of disc herniation was an inclusion criterion. In clinical practice, MRI verification is not mandatory, as it is in surgical treatment, before introducing structured physiotherapy treatment to patients with symptoms from a disc herniation. Consequently, treatment according to the structured physiotherapy treatment model can start early after the commencement of symptoms, as it is not necessary to wait for an MRI. It is possible to speculate that, if treatment with a structured physiotherapy model starts earlier than in the present study, the improvements would be even better, further reducing the risk of persistent pain and accompanying problems. Moreover, the need for MRI is likely to diminish; this, however, should be further evaluated in future studies.
One explanation for the good results of this study could be that the patients followed a structured physiotherapy treatment model, comprising MDT and trunk stabilization exercises, allowing for an individual design and progression of the treatment. Similar results were described in a retrospective cohort study (39) using several treatment methods for pain control as well as for exercise training for patients with lumbar disc herniation. The evaluation was not carried out until approximately 31 months after treatment. The results of Saal et al. (39) and of the present study are in agreement, in that structured physiotherapy treatment can reduce symptoms, but symptoms were relieved much more rapidly in the present study.
In a multicentre study comprising 501 patients, randomized to surgery or non-operative care, 18% of the patients assigned to non-operative treatment underwent surgery within 6 weeks and 30% had surgery at approximately 3 months (7). The nonoperative treatment group received non-specified ”usual care”, which could include a variety of different treatment methods. In contrast, the patients in the present study were offered a structured physiotherapy treatment model that included both bio-psychological and social components, as described in the International Classification of Functioning, Disability and Health (40).
There are many possible explanations for the positive effects seen in this present study, and 5 of these will now be discussed. Firstly, the patients were well informed about the design of the structured physiotherapy treatment model, including the timetable for different phases of the treatment and when the treatment was planned to end. This information enhanced the patients’ opportunity for self-management and gave them an active role in treatment decision-making.
Secondly, the patients acquired strategies to deal with their pain by using the different activities and movements in order to reduce pain according to the MDT method (14). The MDT method aims to enhance the patients’ ability to cope with the symptoms, motivate the patient to comply with the treatment and empower them to achieve independence. Leijon et al. (41) have shown that low levels of motivation plus pain are important factors that enhance non-adherence to physical activity. It therefore appears important to reduce pain and increase motivation as early as possible. It is reasonable to believe that, when the patients participated in the evaluation of different activities and exercises, this augmented their opportunity to discover the connection between activities and the following reduction or increase in symptoms. This could have led to the increased self-efficacy and empowerment of the patients. The use of empowerment in physiotherapy has been recommended in a review by Perrault (42), who argues that empowerment improves the intervention.
Thirdly, the intensity of exercises was gradually increased on an individual basis with respect to the patients’ reported pain. The objective was to strengthen the patients’ self-efficacy, which also improved significantly in the present study. Fourthly, the trunk stabilization exercises were conducted with the aim of increasing deep trunk muscle control (23). It can be speculated that the physiological effects of training may also have led to reduced pain through increased blood circulation, muscle relaxation and the release of pain-reducing substances, such as endorphins.
Finally, one reason for the improvements could be that the physiotherapists were experienced and well educated in the MDT method. Subsequently, the physiotherapists were able to guide the patients during the rehabilitation process. It is, however, not possible to determine whether and how much each of the reasons discussed above contributed to the improvements. It seems reasonable to assume that all 5 factors were operating.
In this study, the majority of patients experienced kinesiophobia before treatment started. As early as 3 months after the structured physiotherapy treatment started, the number of patients with kinesiophobia fell dramatically and the majority of patients no longer experienced kinesiophobia. These results are in agreement with those of a study of patients with chronic pain and high kinesiophobia who increased their physical activity level after a pain management programme designed to enable the patients to regain overall function (43).
There are some limitations to this study. It is not possible to exclude the possibility that some patients may have improved spontaneously without treatment. Measures were taken to limit this risk by using symptoms for at least 6 weeks as an inclusion criterion. Again, the majority of patients had symptoms for more than 3 months. Another limitation might relate to whether the patients were selected accurately for the study. Clinically experienced orthopaedic surgeons evaluated the clinical findings and the MRI scans and classified the patients as surgical candidates based on recommendations from the American Academy of Orthopaedic Surgeons for intervention for disc herniation published in 1993 (21). The patients included in the present study also fulfilled the recommendations as presented by Bono and co-workers in 2006 (38). The patients can therefore be regarded as serving as their own controls, and comparisons can be made with baseline symptoms and with patients from other studies. An RCT would have been the best way to explore different treatment options; however, we did not reach the number of patients required for an RCT. As the treatment model used in the present study has not been evaluated previously in a group of patients with long-standing pain, with the majority of the patients having pain for more than 3 months due to disc herniation, and, as the results are clinically interesting, it was decided to present the results as a cohort study.
In conclusion, this study shows that patients eligible for lumbar disc surgery improved significantly after treatment with the structured physiotherapy model, as early as 3 months after treatment, and the results could still be seen at the 24-month follow-up. Consequently, these patients did not qualify for lumbar disc surgery 3 months after the physiotherapy treatment started. Moreover, the majority of patients had symptoms for more than 3 months at the start of treatment and, for this reason, most of the spontaneous healing ought to have occurred before this study started. This study therefore recommends adoption of the structured physiotherapy treatment model before considering surgery when patients report symptoms such as pain and disability due to lumbar disc herniation.
Acknowledgements
The authors would like to thank physiotherapists Patrik Drevander, Christina Grundén, Sofia Fridén and Eva Fahlgren for treating the patients and Valter Sundh for statistical support. This study was supported by grants from the Health & Medical Care Committee of the Västra Götaland Region, Renée Eander’s Foundation and Wilhelm & Martina Lundgren’s Foundation of Science.
Herniated discs can cause pain, numbness and weakness, a variety of symptoms which may often become so severe, that surgery might seem like the only option for fast relief. However, a structured physiotherapy treatment model can provide rapid relief to patients who qualify for lumbar disc surgery, according to the results of the research study. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
1. Konstantinou K, Dunn KM. Sciatica: review of epidemiological
studies and prevalence estimates. Spine (Phila Pa 1976) 2008;
33: 2464–2472.
2. Nygaard OP, Kloster R, Solberg T. Duration of leg pain as a
predictor of outcome after surgery for lumbar disc herniation:
a prospective cohort study with 1-year follow up. J Neurosurg
2000; 92: 131–134.
3. Orief T, Orz Y, Attia W, Almusrea K. Spontaneous resorption
of sequestrated intervertebral disc herniation. World Neurosurg
2012; 77: 146–152.
4. Maigne JY, Rime B, Deligne B. Computed tomographic follow-up
study of forty-eight cases of nonoperatively treated lumbar intervertebral
disc herniation. Spine (Phila Pa 1976) 1992; 17: 1071–1074.
5. Takada E, Takahashi M, Shimada K. Natural history of lumbar disc
hernia with radicular leg pain: spontaneous MRI changes of the
herniated mass and correlation with clinical outcome. J Orthopaed
Surg (Hong Kong) 2001; 9: 1–7.
6. Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome
of sciatica at short-term follow-up. Br J Gen Pract 2002;
52: 119–123.
7. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom
B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar
disk herniation: the Spine Patient Outcomes Research Trial
(SPORT): a randomized trial. JAMA 2006; 296: 2441–2450.
8. Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW.
Prolonged conservative care versus early surgery in patients with
sciatica caused by lumbar disc herniation: two year results of a
randomised controlled trial. BMJ 2008; 336: 1355–1358.
9. Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term
outcomes of surgical and nonsurgical management of sciatica secondary
to a lumbar disc herniation: 10 year results from the maine
lumbar spine study. Spine (Phila Pa 1976) 2005; 30: 927–935.
10. Weber H. Lumbar disc herniation. A controlled, prospective
study with ten years of observation. Spine (Phila Pa 1976) 1983;
8: 131–140.
11. Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized
controlled trial with 2 years of follow-up. Spine (Phila Pa 1976)
2006; 31: 2409–2414.
12. Jacobs WC , van Tulder M, Arts M, Rubinstein SM, van Middelkoop
M, Ostelo R, et al. Surgery versus conservative management of
sciatica due to a lumbar herniated disc: a systematic review. Eur
Spine J 2011; 20: 513–522.
13. Svensson GL, Lundberg M, Östgaard HC, Wendt GK. High degree
of kinesiophobia after lumbar disc herniation surgery: a crosssectional
study of 84 patients. Acta Orthop 2011; 82: 732–736.
14. McKenzie R, May S. The lumbar spine: mechanical diagnosis
& therapy. 2nd ed. Spinal Publications New Zealand Limited:
Wellington; 2003.
15. Clare HA, Adams R, Maher CG. A systematic review of efficacy
of McKenzie therapy for spinal pain. Aust J Physiother 2004;
50: 209–216.
16. Paatelma M, Kilpikoski S, Simonen R, Heinonen A, Alen M, Videman
T. Orthopaedic manual therapy, McKenzie method or advice
only for low back pain in working adults: a randomized controlled
trial with one year follow-up. J Rehabil Med 2008; 40: 858–863.
17. Brötz D, Kuker W, Maschke E, Wick W, Dichgans J, Weller M.
A prospective trial of mechanical physiotherapy for lumbar disk
prolapse. J Neurol 2003; 250: 746–749.
18. Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic
region: effect and possible mechanisms. J Electromyogr
Kinesiol 2003; 13: 361–370.
19. Hides JA, Jull GA, Richardson CA. Long-term effects of specific
stabilizing exercises for first-episode low back pain. Spine (Phila
Pa 1976) 2001; 26: E243–E248.
20. Yilmaz F, Yilmaz A, Merdol F, Parlar D, Sahin F, Kuran B. Efficacy
of dynamic lumbar stabilization exercise in lumbar microdiscectomy.
J Rehabil Med 2003; 35: 163–167.
21. Nachemson AL. Lumbar disc herniation – conclusions. Acta Orthop
Scand Suppl 1993; 251: 49–50.
22. Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman
T, Alen M. Interexaminer reliability of low back pain assessment
using the McKenzie method. Spine (Phila Pa 1976) 2002; 27:
E207–E214.
23. Richardson CA, Jull GA. Muscle control-pain control. What exercises
would you prescribe? Man Ther 1995; 1: 2–10.
24. Scott J, Huskisson EC. Graphic representation of pain. Pain 1976;
2: 175–184.
25. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry
low back pain disability questionnaire. Physiotherapy 1980; 66:
271–273.
26. Öberg B, Enthoven P, Kjellman G, Skargren E. Back pain in
primary care: a prospective cohort study of clinical outcome and
healthcare consumption. Adv Physiother 2003; 5: 98.
27. Bombardier C. Outcome assessments in the evaluation of treatment
of spinal disorders: summary and general recommendations. Spine
2000; 25: 3100–3103.
28. Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of
movement/(re)injury in chronic low back pain and its relation to
behavioral performance. Pain 1995; 62: 363–372.
29. EuroQol – a new facility for the measurement of health-related quality
of life. The EuroQol Group. Health Policy 1990; 16: 199–208.
30. Zung WW. A self-rating depression scale. Arch Gen Psychiatry
1965; 12: 63–70.
31. Estlander AM, Vanharanta H, Moneta GB, Kaivanto K. Anthropometric
variables, self-efficacy beliefs, and pain and disability
ratings on the isokinetic performance of low back pain patients.
Spine 1994; 19: 941–947.
32. Strömqvist B, Jönsson B, Fritzell P, Hägg O, Larsson BE, Lind B.
The Swedish National Register for lumbar spine surgery: Swedish
Society for Spinal Surgery. Acta Orthop Scand 2001; 72: 99–106.
33. den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans
M, Evers AW. A systematic review of bio-psychosocial risk factors
for an unfavourable outcome after lumbar disc surgery. Eur Spine
J 2006; 15: 527–536.
34. Weber H, Holme I, Amlie E. The natural course of acute sciatica
with nerve root symptoms in a double-blind placebo-controlled
trial evaluating the effect of piroxicam. Spine (Phila Pa 1976)
1993; 18: 1433–1438.
35. Werneke M, Hart DL, Cook D. A descriptive study of the centralization
phenomenon. A prospective analysis. Spine (Phila Pa
1976) 1999; 24: 676–683.
36. Hahne AJ, Ford JJ, Hinman RS, Taylor NF, Surkitt LD, Walters
AG, et al. Outcomes and adverse events from physiotherapy
functional restoration for lumbar disc herniation with associated
radiculopathy. Disabil Rehabil 2011; 33: 1537–1547.
37. Balague F, Nordin M, Sheikhzadeh A, Echegoyen AC, Brisby H,
Hoogewoud HM, et al. Recovery of severe sciatica. Spine (Phila
Pa 1976) 1999; 24: 2516–2524.
38. Bono CM, Wisneski R, Garfin SR. Lumbar disc herniations. In:
Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA,
editors. Rothman-Simeone the spine. 5th ed. Saunders Elsevier:
Philadelphia; 2006: p. 979–980.
39. Saal JA, Saal JS. Nonoperative treatment of herniated lumbar
intervertebral disc with radiculopathy. An outcome study. Spine
(Phila Pa 1976) 1989; 14: 431–437.
40. World Health Organisation. International Classification of Functioning,
Disability and Health (ICF). 2001 [cited 2012 Oct 9].
Available from: www.who.int/classifications/icf/en/.
41. Leijon ME, Faskunger J, Bendtsen P, Festin K, Nilsen P. Who is
not adhering to physical activity referrals, and why? Scand J Prim
Health Care 2011; 29: 234–240.
42. Perreault K. Linking health promotion with physiotherapy for low
back pain: a review. J Rehabil Med 2008; 40: 401–409.
43. Koho P, Orenius T, Kautiainen H, Haanpaa M, Pohjolainen T, Hurri
H. Association of fear of movement and leisure-time physical
activity among patients with chronic pain. J Rehabil Med 2011;
43: 794–799.

Additional Topics: Neck Pain
Neck pain is a common complaint which can result due to a variety of injuries and/or conditions. According to statistics, automobile accident injuries and whiplash injuries are some of the most prevalent causes for neck pain among the general population. During an auto accident, the sudden impact from the incident can cause the head and neck to jolt abruptly back-and-forth in any direction, damaging the complex structures surrounding the cervical spine. Trauma to the tendons and ligaments, as well as that of other tissues in the neck, can cause neck pain and radiating symptoms throughout the human body.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


