Chiropractor, Dr. Alexander Jimenez gives insight into the relevant anatomy and functional biomechanics of the piriformis muscle, highlights the role it plays in musculoskeletal dysfunction and looks at management options in cases of muscle dysfunction.
The piriformis muscle (PM) is well-known in the fraternity of sports medicine as a significant muscle in the posterior hip. It is a muscle that has a role in controlling hip joint rotation and abduction, and it is also a muscle made famous due to its ‘inversion of action’ in rotation. Furthermore, the PM also grabs attention due to its role in the contentious ‘piriformis syndrome’, a condition implicated as a potential source of pain and dysfunction, not only in the general population but in athletes as well.
Table of Contents
Relevant Anatomy
The name piriformis was first coined by Belgian Anatomist Adrian Spigelius in the early 17th century. Its name is derived from the Latin word ‘pirum’ meaning ‘pear’ and ‘forma’ meaning ‘shape’ – ie a pear shaped muscle (see Figure 1)(1).
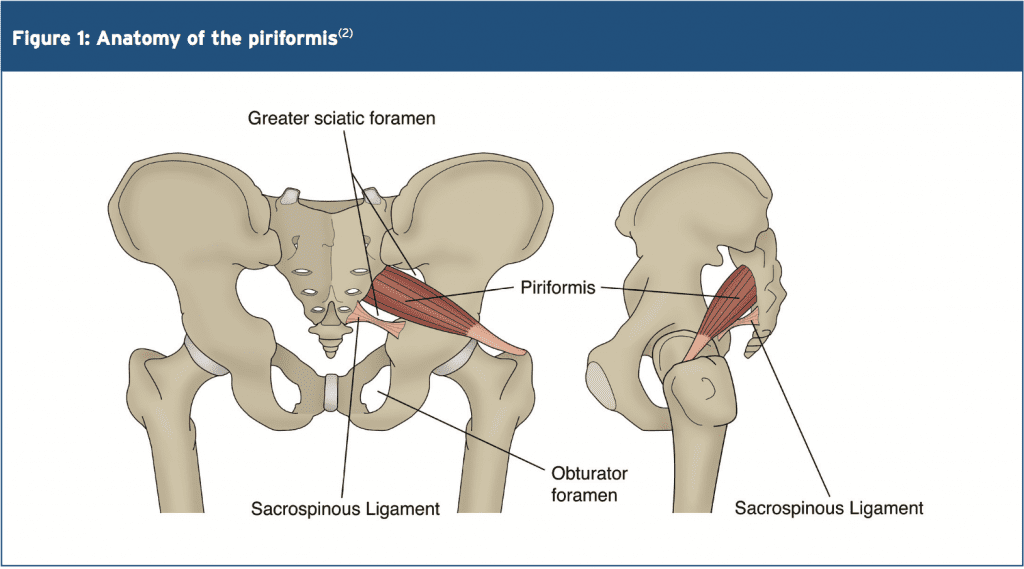 The PM originates on the anterior surface of the sacrum and is anchored to it by three fleshy attachments between the first, second, third and fourth anterior sacral foramina(2). Occasionally its origin may be so broad that it joins the capsule of the sacroiliac joint above and with the sacrotuberous and/or sacrospinous ligament below(3,4).
The PM originates on the anterior surface of the sacrum and is anchored to it by three fleshy attachments between the first, second, third and fourth anterior sacral foramina(2). Occasionally its origin may be so broad that it joins the capsule of the sacroiliac joint above and with the sacrotuberous and/or sacrospinous ligament below(3,4).
PM is a thick and bulky muscle, and as it passes out of the pelvis through the greater sciatic foramen, it divides the foramen into the suprapiriform and infra-piriform foramina(5). As it courses antero-laterally through the greater sciatic foramen, it tapers out to form a tendon that is attached to the superior-medial surface of the greater trochanter, commonly blending with the common tendon of the obturator internus and gemelli muscles(6).
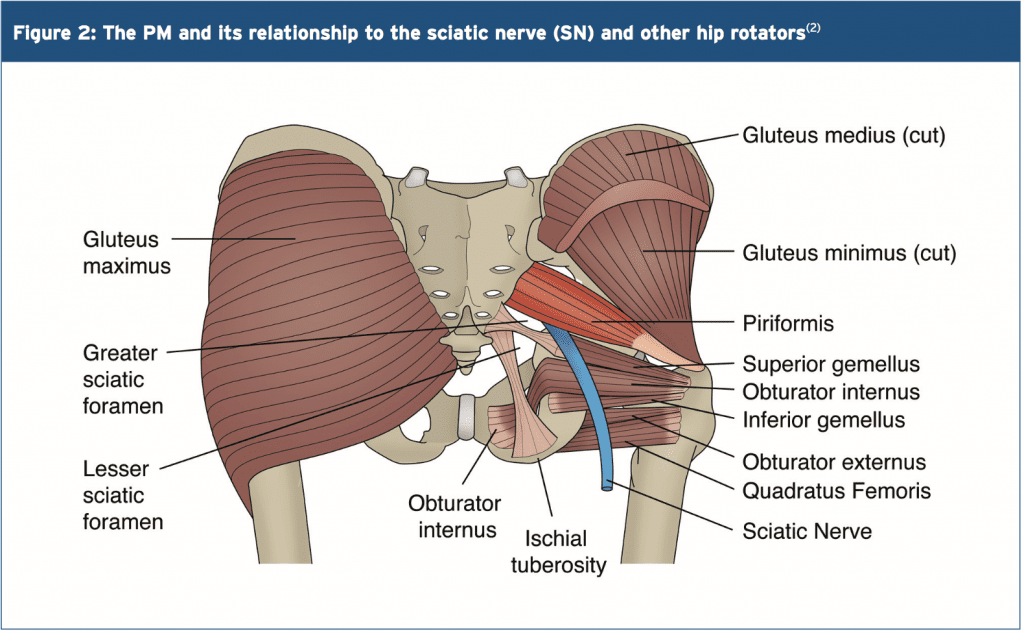
The nerves and blood vessels in the suprapiriform foramen are the superior gluteal nerve and vessels, and in the infra- piriforma fossa are the inferior gluteal nerves and vessels and the sciatic nerve (SN)(5). Due to its large volume in the greater sciatic foramen, it has the potential to compress the numerous vessels and nerves that exit the pelvis.
PM is closely associated with the other short hip rotators that lie inferior such as the superior gemellus, obturator internus, inferior gemellus and obturator externus(2). The primary difference between the PM and other short rotators is the relationship to the SN. The PM passes posterior to the nerve whereas the other otators pass anterior (see figure 2).
 Variants
Variants
A few anatomical variants have been found with the PM:
1. Additional medial attachments to the first and fifth sacral vertebrae and to the coccyx(7).
2. The tendon may fuse with the gluteus medius or minimus above, or superior gemellus below(7).
3. In less than 20% of cases it is divided into two distinct portions through which part or all of the sciatic nerve may pass(7).
4. It may blend with the posterior hip joint capsule as a conjoined tendon with the obturator internus(8).
5. The distal attachment of the PM has shown to vary in dimensions and position on the supero-medial surface of the greater trochanter. It can span a distance of between 25-64% of the anterior-posterior length on the greater trochanter, with 57% attaching more anterior and 43% more posterior(9).
6. Pine et al (2011) studied the insertion point extensively and found that four types of insertion existed and these were classified based on the relationship to the obturator internus(10). The variability in position and breadth of the distal attachment of the PM muscle may influence the validity of the concept known as ‘inversion of action’ (see below).
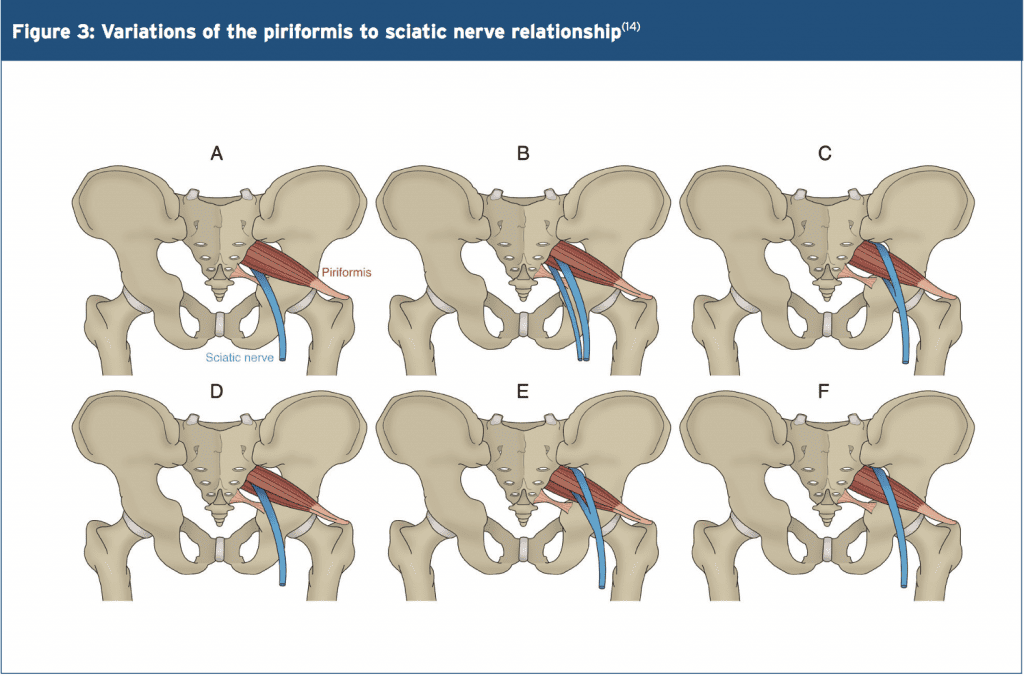
The other hotly debated issue is the relationship between the PM and the SN. The conclusion is that there are several anatomical variations of the PM and its SN relationship. The sub-types of this variation include(11-13):
- Type 1 (A below). Typical pear shape muscle with the nerve running anteriorly and inferiorly to this (in 70%-85% of cases).
- Type 2 (B below). The PM is divided into two parts with the common peroneal nerve running between the two parts and the tibial nerve running anterior and below (found in 10-20% of cases).
- Type 3 (C below). The peroneal portion loops over the top of the muscle and the tibial portion is below (found in 2-3% of cases).
- Type 4 (D below). Undivided nerve passing through the PM (occurs in about 1% of cases).
It is also believed that two other very uncommon variations occur (see E and F below).
Type A is the most common variation, showing the SN passing below the PM
Functional Considerations
The primary functional roles of the PM are;
1. Hip external rotation(15).
2. Abductor at 90 degrees of hip flexion(15).
3. In weight-bearing, the PM restrains the femoral internal rotation during stance phase of walking and running(2).
4. Assists the short hip rotators in compressing the hip joint and stabilising the joint(6).
5. As it can exert an oblique force on the sacrum, it may produce a strong rotary shearing force on the sacroiliac joint (SIJ). This would displace the ipsilateral base of the sacrum anteriorly (forward) and the apex of the sacrum posteriorly(16).
As the PM is the most posterior of the hip external rotators due to its attachment on the anterior surface of the sacrum, it has the greatest leverage to exert a rotation effect on the hip joint. It is often seen clinically that the PM appears to be tight and hypertonic, while the other short hip rotators that are closer to the axis of rotation become inhibited and hypotonic.
Inversion Of Action
The most contentious issue related to the function of the PM is its ‘reversal-of- function role’ or ‘inversion of action’ role. Many authors have suggested that as the hip approaches angles of 60-90 degrees and greater, the tendon of the PM shifts superiorly on the greater trochanter. As a result, its line of pull renders it ineffective as a hip external rotator; however it does contribute to internal hip rotation. Therefore it reverses its rotation role at high hip flexion angles(15,17,18).
The function of the PM at varying joint angles is an important consideration for the clinician who is evaluating and treating ‘piriformis syndrome’. Often it has been advocated to stretch the hip into flexion, adduction and external rotation to stretch the PM over the glutes by utilising the ‘reversal of function’ concept.
However, more recent anatomical dissection studies have shown that the attachment of the PM onto the greater trochanter can be variable and in some instances it may insert in a position whereby it is unable to reverse its function, for example in a more posteriorly placed attachment(19). Therefore, stretching the PM into external rotation when the hip is flexed beyond 90 degrees – based upon reversal of function – would be ineffective as a treatment or misleading as an examination technique(19)
MSK Dysfunction & PM Syndrome
Many decades ago, the role that the PM played in creating sciatic-like symptoms was first suggested by Yeoman (1928) when it was considered that some cases of sciatica may originate outside the spine(20). This was supported soon after when Freiberg and Vinkle (1934) successfully cured sciatica by surgically dividing the PM(21). Based on cadaver dissections Beaton and Anson (1938) gave the hypothesis that the spasm of the PM could be responsible for the irritation of the SN(12).
The term ‘piriformis syndrome’ was first coined by Robinson in 1947(22) and was applied to sciatica thought to be caused by an abnormality in the PM (usually traumatic in origin) with emphasis on ruling out more common causes of sciatica such as nerve root impingement from a disc protrusion. It soon became an accepted clinical entity – but with no consensus about the exact clinical signs and diagnostic tests to differentiate it from other sources of sciatica(23,24).
Piriformis syndrome can be defined as a clinical entity whereby the interaction between the PM and SN may irritate the SN and produce posterior hip pain with distal referral down the posterior thigh, imitating ‘true sciatica’. Isolating the dysfunction to this region usually follows exclusion of the more common causes of buttock pain and sciatica.
More specifically, complaints of buttock pain with distal referral of symptoms are not unique to the PM. Similar symptoms are prevalent with the more clinically evident lower back pain syndromes and pelvic dysfunctions. Thus, a thorough evaluation of these regions must be performed to exclude underlying pathology(4). It has been suggested that piriformis syndrome’ is responsible for 5-6% of cases of sciatica(25,26). In the majority of cases, it occurs in middle-aged patients (mean age 38 yr)(27) and is more prevalent in women(28).
Pathogenesis Of Piriformis Syndrome (PS)
PS may be caused by or relate to three primary causative factors;
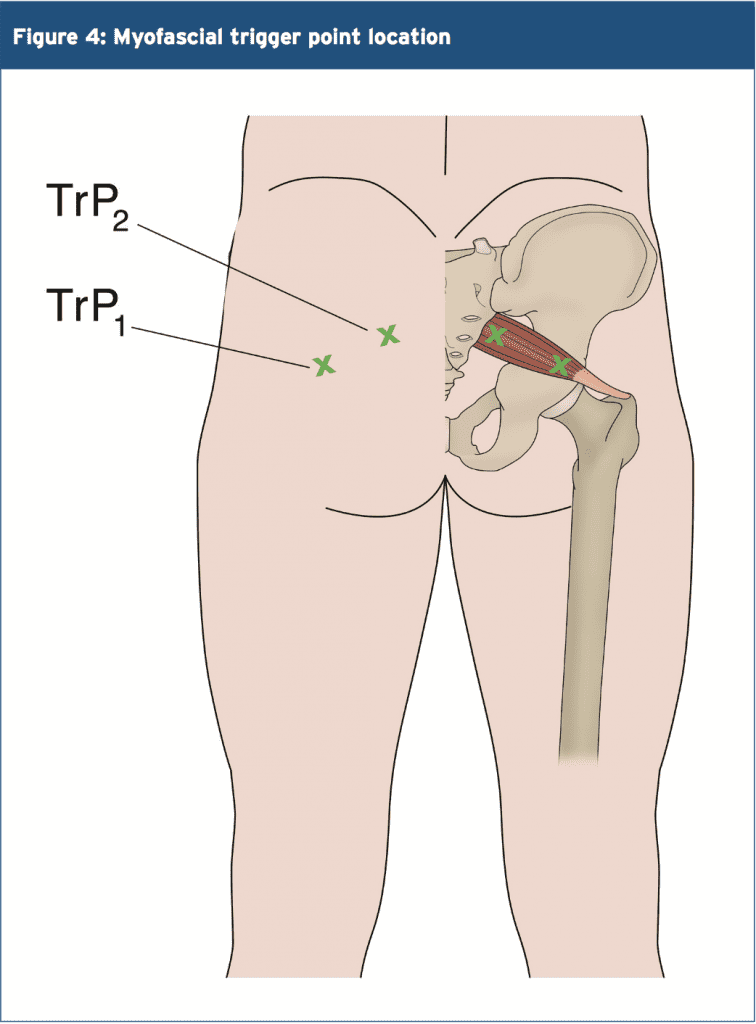
1. Referred pain due to myofascial trigger points (see Figure 4)(2,28-30). Examples include tight and shortened muscle fibres precipitated by muscle overuse such as squat and lunge movements in external rotation, or direct trauma(16). This increases the girth of the PM during contraction, and this may the source of the compression/entrapment.
 2. Entrapment of the nerve against the greater sciatic foramen as it passes through the infrapiriform fossa, or within a variant PM(29,31).
2. Entrapment of the nerve against the greater sciatic foramen as it passes through the infrapiriform fossa, or within a variant PM(29,31).
3. SIJ dysfunction causing PM spasm(29,32).
Janvokic (2013) has presented a number of causative factors in PS(29);
1. Gluteal trauma in the sacroiliac or gluteal areas.
2. Anatomical variations.
3. Myofascial trigger points.
4. Hypertrophy of the PM or spasm of the PM.
5. Secondary to spinal surgery such as laminectomy.
6. Space occupying lesions such as neoplasm, bursitis, abscess, myositis. 7. Intragluteal injections.
8. Femoral nailing.
Symptoms
Typical symptoms reported in piriformis syndrome include:
- A tight or cramping sensation in the buttock and/or hamstring(33).
- Gluteal pain (in 98% of cases)(34).
- Calf pain (in 59% of cases)(34).
- Aggravation through sitting and squatting(35), especially if the trunk is inclined forward or the leg is crossed over the unaffected leg(36).
- Possible peripheral nerve signs such as pain and paraesthesia in the back, groin, buttocks, perineum, back of the thigh (in 82% of cases)(34).
Physical Findings & Examinations
- Palpable spasm in and around the PM and obturator internus and external tenderness over the greater sciatic notch (in 59-92% of cases)(34,35). The patient is placed in the Sims position. The piriformis line overlies the superior border of the PM and extends from immediately above the greater trochanter to the cephalic border of the greater sciatic foramen at the sacrum. The line is divided into equal thirds. The fully rendered thumb presses on the point of maximum trigger-point tenderness, which is usually found just lateral to the junction of the middle and last thirds of the line.
- Hip flexion with active external rotation or passive internal rotation may exacerbate the symptoms(36).
- Positive SLR that is less than 15 degrees the normal side(37).
- Positive Freiberg’s sign (in 32-63% of cases)(34,35). This test involves reproducing pain on passive forced internal rotation of the hip in the supine position – thought to result from passive stretching of the PM and pressure on the sciatic nerve at the sacrospinous ligament.
- Pacers sign (in 30-74% of cases)(34,35). This test involves reproducing pain and weakness on resisted abduction and external rotation of the thigh in a sitting position.
- Pain in a FAIR position(34). This involves the reproduction of pain when the leg is held in flexion, adduction and internal rotation.
- An accentuated lumbar lordosis and hip flexor tightness predisposes one to increased compression of the sciatic nerve against the sciatic notch by a shortened piriformis(38).
- Electro-diagnostic tests may prove useful (see below).
Investigations
Conventional imaging such as X-ray, CT scan and MRI tend to be ineffective in diagnosing piriformis syndrome.
However, some value may exist in electro- diagnostic testing.
It is beyond the scope of this paper to discuss in detail the process of electro- diagnostic testing; the reader is directed to references for more a more detailed description of how these tests are administered(35,36,39). However the purpose of these tests is to find conduction faults in the SN. Findings such as long-latency potentials (for example the H reflex of the tibial nerve and/or peroneal nerve) may be normal at rest but become delayed in positions where the hip external rotators are tightened(27,36,39).
It is accepted that the tibial division of the SN is usually spared, the inferior gluteal nerve that supplies the gluteus maximus may be affected and the muscle becomes atrophied(40). However testing of the peroneal nerve may provide more conclusive results as is more likely to be the impinged portion of the SN. The H-wave may become extinct during the painful position of forced adduction-internal rotation of the affected leg(36).
The ‘Myth’ Of Piriformis Syndrome
Stewart 2003 argues that piriformis syndrome is an often over-used term to describe any non-specific gluteal tenderness with radiating leg pain(41). He argues that only in rare cases is the PM implicated in nerve compression of the SN to truly qualify as a piriformis syndrome. He cites only limited evidence and cases where the diagnosis of piriformis syndrome can be made.
1. Compressive damage to the SN by the PM. Stewart cites studies whereby in few isolated studies, the SN was seen to be compressed by the PM in instances such as hypertrophy of the muscle, usual anatomical anomalies such as a bifid PM, and due to compression by fibrous bands.
2. Trauma and scarring to the PM leading to SN involvement; it is possible that rare cases of true Piriformis Syndrome have been caused by direct heavy trauma to the PM due to a blunt trauma to the muscle. This is termed ‘post- traumatic PS’.
McCory (2001) supports this argument by stating that it is more likely that (given the anatomical relationship of the PM to the various nerves in the deep gluteal region) the buttock pain represents entrapment of the gluteal nerves, and the hamstring pain entrapment of the posterior cutaneous nerve of the thigh, rather than the SN alone(33). This would explain the clinically observed phenomenon in the absence of distal sciatic neurological signs. Whether the PM is the cause of the compression has not been clearly established. It is possible that the obturator internus/gemelli complex is an alternative cause of neural compression. He suggests using the term ‘deep gluteal syndrome’ rather than piriformis syndrome.
Treatment
When it is believed that a piriformis syndrome exists and the clinician feels that a diagnosis has been made, the treatment will usually depend on the suspected cause. If the PM is tight and in spasm then initially conservative treatment will focus on stretching and massaging the tight muscle to remove the PM as being the source of the pain. If this fails, then the following have been suggested and may be attempted(23,36):
- Local anaesthetic block – usually performed by anaesthesiologists who have expertise in pain management and in performing nerve blocks.
- Steroid injections into the PM.
- Botulinum toxin injections into the PM.
- Surgical Neurolysis.
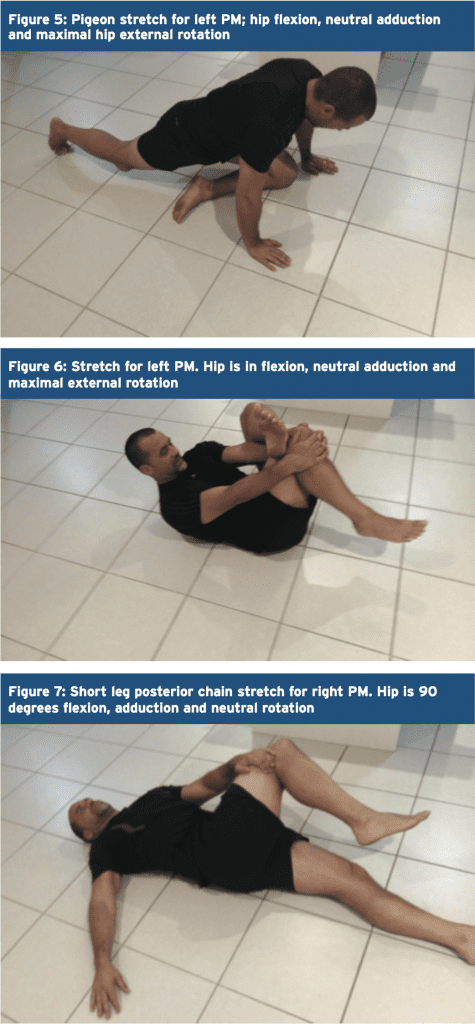
Here, we will focus on therapist-directed interventions such as stretching of the PM and direct trigger point massage. It has always been advocated that PM stretches are done in positions of hip flexion greater than 90 degrees, adduction and external rotation to utilize the ‘inversion of action’ effect of the PM to isolate the stretch to this muscle independent of the other hip external rotators.
However, recent evidence from Waldner (2015) using ultrasound investigation discovered that there was no interaction between hip flexion angle and the thickness of the PM tendon in both internal and lateral hip rotation stretching – suggesting that the PM does not invert its action(19). Furthermore, Pine et al (2011)(9) and Fabrizio et al (2011)(10) in their cadaveric studies found that the PM insertion is a lot more complex and varied than first thought. It is possible that the PM may invert its action only in some subjects but not others.
Therefore, due to the disagreements and confusions over the ‘inversion of action’ concept, it is recommended that the clinician ‘covers all bases’ and performs two variations of a PM stretch – stretches in flexion, adduction and external rotation and stretches in flexion, adduction and internal rotation. Examples of these stretches are given in figures 5-7 below.
 Trigger Points & Massage
Trigger Points & Massage
(see Figure 8)
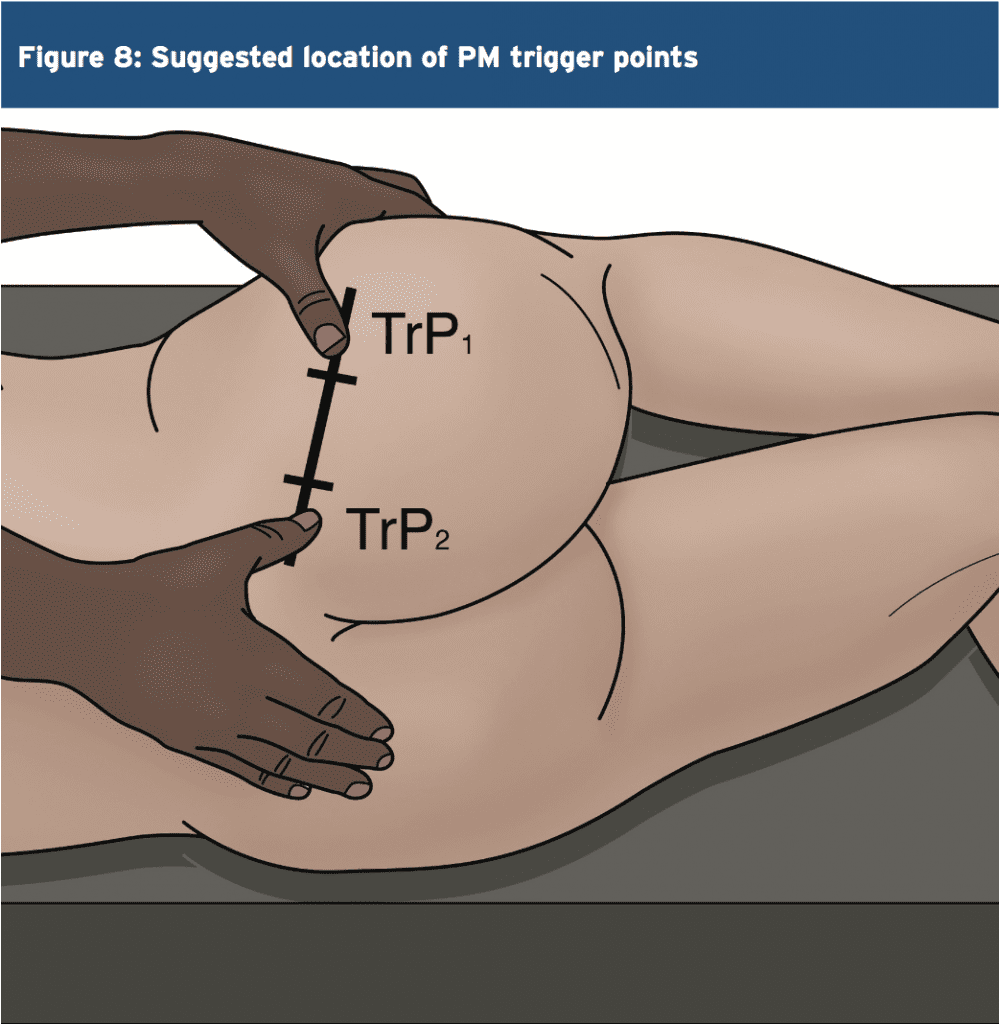 The best approach to palpate the PM trigger points is in the position suggested by Travel and Simons(2) and this is shown below. In this position, the clinician can feel for the deep PM trigger points and apply a sustained pressure to alleviate the trigger points – and also apply a flush massage to the muscle in this position. In this position the large gluteus maximus is relaxed and it is easier to feel the deeper PM.
The best approach to palpate the PM trigger points is in the position suggested by Travel and Simons(2) and this is shown below. In this position, the clinician can feel for the deep PM trigger points and apply a sustained pressure to alleviate the trigger points – and also apply a flush massage to the muscle in this position. In this position the large gluteus maximus is relaxed and it is easier to feel the deeper PM.
Summary
The PM is a deep posterior hip muscle that is closely related anatomically to both the sacroiliac joint and the sciatic nerve. It is a hip external rotator at hip flexion angles of neutral to 60 degrees of hip flexion, an abductor when in flexion and also contributes to hip extension.
It has been previously accepted that the PM will ‘invert its action’ or ‘reverse its function’ after 60 degrees of flexion to become a hip internal rotator. However, recent ultrasound and cadaveric studies has found conflicting evidence that this ‘inversion of action’ may in fact not exist.
PM is a muscle that is a dominant hip rotator and stabiliser, and thus has a tendency to shorten and become hypertonic. Therefore, stretching and massage techniques are best utilised to reduce the tone through the muscle. Furthermore, it has also been implicated in compression and irritation of the sciatic nerve – often referred to as piriformis syndrome’.
References
1. Contemp Orthop 6:92-96, 1983.
2. Simons et al (1999) Travell and Simons’ Myofascial Pain and Dysfunction. Volume 1 Upper Half of the Body (2nd edition). Williams and Wilkins. Baltimore.
3. Anesthesiology; 98: 1442-8, 2003.
4. Joumal of Athletic Training 27(2); 102-110, 1996.
5. Journal of Clinical and Diagnostic Research. Mar, Vol-8(3): 96-97, 2014.
6. Clemente CD: Gray’s Anatomy of the Human Body, American Ed. 30. Lea & Febiger, Philadelphia, 1985 (pp. 568-571).
7. Med J Malaysia 36:227-229, 1981.
8. J Bone Joint Surg;92-B(9):1317-1324, 2010.
9. J Ortho Sports Phys Ther. 2011;41(1):A84, 2011.
10. Clin Anat;24:70-76, 2011.
11. Med Sci Monit, 2015; 21: 3760-3768, 2015.
12. J Bone Joint Surg Am 1938, 20:686-688,1938.
13. Journal of Clinical and Diagnostic Research. 2014 Aug, Vol-8(8): 7-9, 2014.
14. Peng PH. Piriformis syndrome. In: Peng PH, editor. Ultrasound for Pain Medicine Intervention: A Practical Guide. Volume 2. Pelvic Pain. Philip Peng Educational Series. 1st ed. iBook, CA: Apple Inc.; 2013 .
15. Kapandji IA. The Physiology of Joints. 2nd ed. London: Churchill Livingstone; 1970: 68.
16. J Am Osteopath Assoc 73:799-80 7,1974.
17. J Biomechanics. 1999;32:493-50, 1999.
18. Phys Therap. 66(3):351-361, 1986.
19. Journal of Student Physical Therapy Research. 8(4), Article 2 110-122, 2015.
20. Lancet. 212: 1119-23, 1928.
21. J Bone Joint Surg Am 16:126–136, 1934.
22. Am J Surg 1947, 73:356-358, 1947.
23. J Neurol Sci; 39: 577–83, 2012.
24. Orthop Clin North Am; 35: 65-71, 2004
25. Arch Phys Med Rehabil; 83: 295-301,2002.
26. Arch Neurol. 63: 1469–72, 2006.
27. J Bone Joint Surg Am; 81: 941-9,1999.
28. Postgrad Med 58:107-113, 1975.
29. Can J Anesth/J Can Anesth;60:1003–1012, 2013.
30. Arch Phys Med Rehabil 69:784, 1988.
31. Muscle Nerve; 40: 10-8, 2009.
32. J Orthop Sports Phys Ther;40(2):103-111, 2010.
33. Br J Sports Med;35:209–211, 2001.
34. Man Ther 2006; 10: 159-69, 2006.
35. Eur Spine J. 19:2095–2109, 2010.
36. Journal of Orthopaedic Surgery and Research, 5:3, 2010.
37. Muscle & Nerve. November. 646-649, 2003.
38. Kopell H, Thomnpson W. Peripheral Entrapment Neuropathies. Huntington, NY: Krieger, 1975:66.
39. Arch Phys Med Rehabil;73:359–64, 1992.
40. J Bone and Joint Surg, 74-A:1553-1559, 1992.
41. Muscle & Nerve. November. 644-646, 2003
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


