After a neurological exam, physical exam, patient history, x-rays and any previous screening tests, a doctor may order one or more of the following diagnostic tests to determine the root of a possible/suspected neurological disorder or injury. These diagnostics generally involve neuroradiology, which uses small amounts of radioactive material to study organ function and structure and ordiagnostic imaging, which use magnets and electrical charges to study organ function.
Table of Contents
Neurological Studies
Neuroradiology
- MRI
- MRA
- MRS
- fMRI
- CT scans
- Myelograms
- PET scans
- Many others
Magnetic Resonance Imaging (MRI)
Shows organs or soft tissue well
- No ionizing radiation
Variations on MRI
- Magnetic resonance angiography (MRA)
- Evaluate blood flow through arteries
- Detect intracranial aneurysms and vascular malformations
Magnetic resonance spectroscopy (MRS)
- Assess chemical abnormalities in HIV, stroke, head injury, coma, Alzheimer’s disease, tumors, and multiple sclerosis
Functional magnetic resonance imaging (fMRI)
- Determine the specific location of the brain where activity occurs
Computed Tomography (CT or CAT Scan)
- Uses a combination of X-rays and computer technology to produce horizontal, or axial, images
- Shows bones especially well
- Used when assessment of the brain needed quickly such as in suspected bleeds and fractures
Myelogram
Contrast dye combined with CT or Xray
Most useful in assessing spinal cord
- Stenosis
- Tumors
- Nerve root injury
Positron Emission Tomography (PET Scan)
Radiotracer is used to evaluate the metabolism of tissue to detect biochemical changes earlier than other study types
Used to assess
- Alzheimer’s disease
- Parkinson’s disease
- Huntington’s disease
- Epilepsy
- Cerebrovascular accident
Electrodiagnostic Studies
- Electromyography (EMG)
- Nerve Conduction Velocity (NCV) Studies
- Evoked Potential Studies
Electromyography (EMG)
Detection of signals arising from the depolarization of skeletal muscle
May be measured via:
- Skin surface electrodes
- Not used for diagnostic purposes, more for rehab and biofeedback
Needles placed directly within the muscle
- Common for clinical/diagnostic EMG
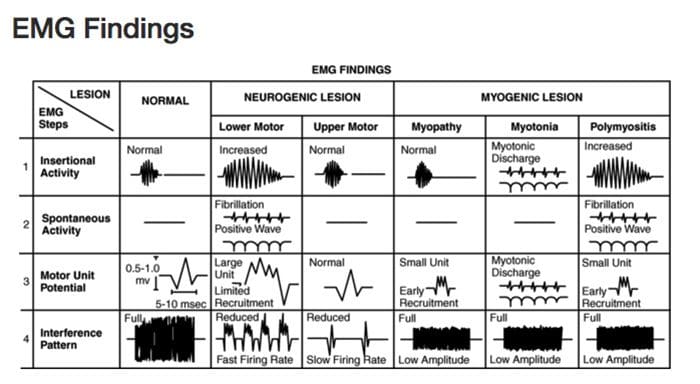 Diagnostic Needle EMG
Diagnostic Needle EMG
Recorded depolarizations may be:
- Spontaneous
- Insertional activity
- Result of voluntary muscle contraction
Muscles should be electrically silent at rest, except at the motor end-plate
- Practitioner must avoid insertion in motor end-plate
At least 10 different points in the muscle are measured for proper interpretation
Procedure
Needle is inserted into the muscle
- Insertional activity recorded
- Electrical silence recorded
- Voluntary muscle contraction recorded
- Electrical silence recorded
- Maximal contraction effort recorded
Samples Collected
Muscles
- Innervated by the same nerve but different nerve roots
- Innervated by the same nerve root but different nerves
- Different locations along the course of the nerves
Helps to distinguish the level of the lesion
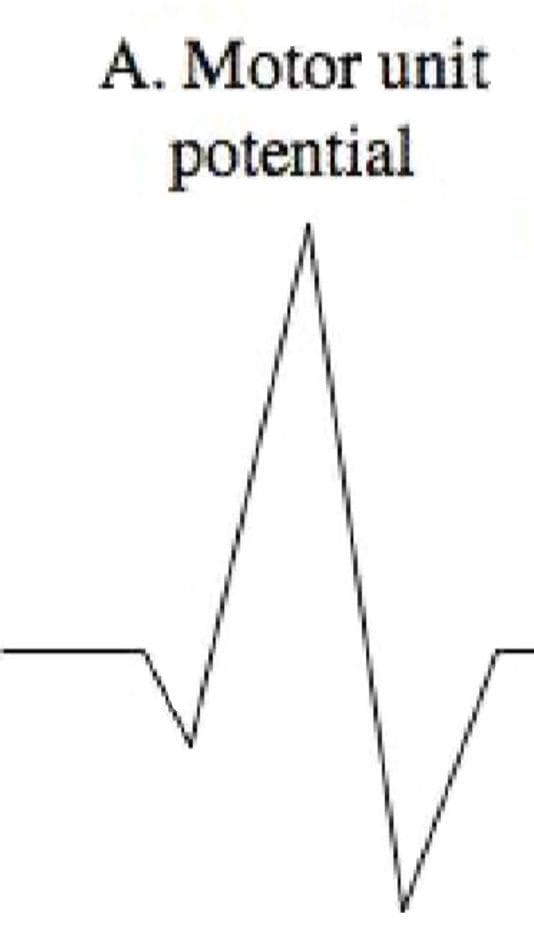
Motor Unit Potential (MUP)
Amplitude
- Density of the muscle fibers attached to that one motor neuron
- Proximity of the MUP
Recruitment pattern can also be assessed
- Delayed recruitment can indicated loss of motor units within the muscle
- Early recruitment is seen in myopathy, where the MUPs tend to be of low amplitude short duration
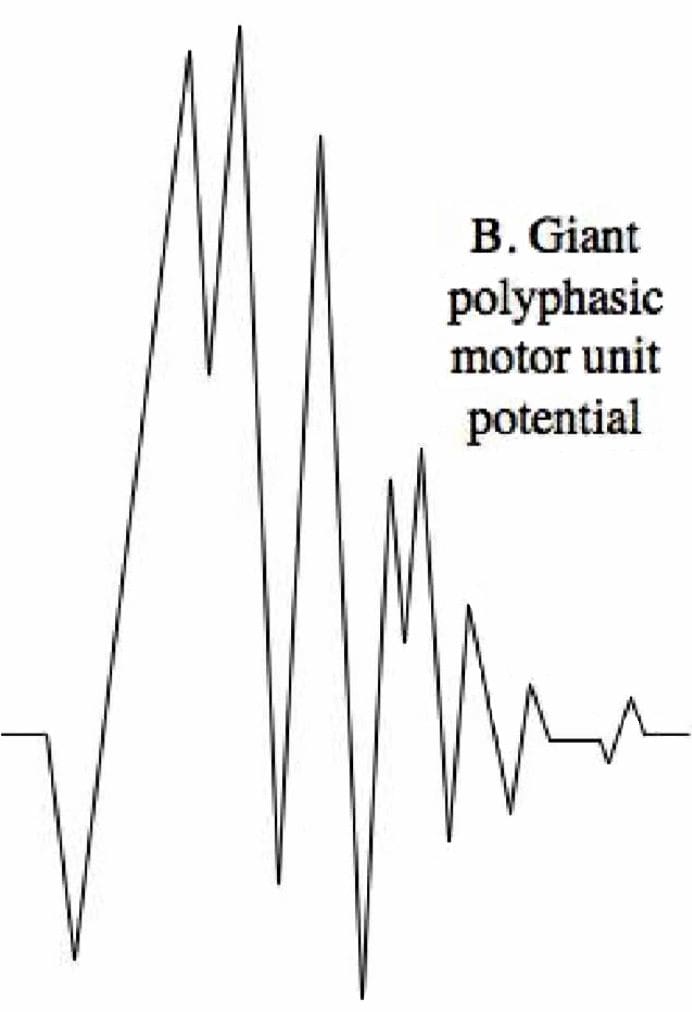
 Polyphasic MUPS
Polyphasic MUPS
- Increased amplitude and duration can be the result of reinnervation after chronic denervation
 Complete Potential Blocks
Complete Potential Blocks
- Demyelination of multiple segments in a row can result in a complete block of nerve conduction and therefore no resulting MUP reading, however generally changes in MUPs are only seen with damage to the axons, not the myelin
- Damage to the central nervous system above the level of the motor neuron (such as by cervical spinal cord trauma or stroke) can result in complete paralysis little abnormality on needle EMG
Denervated Muscle Fibers
Detected as abnormal electrical signals
- Increased insertional activity will be read in the first couple of weeks, as it becomes more mechanically irritable
As muscle fibers become more chemically sensitive they will begin to produce spontaneous depolarization activity
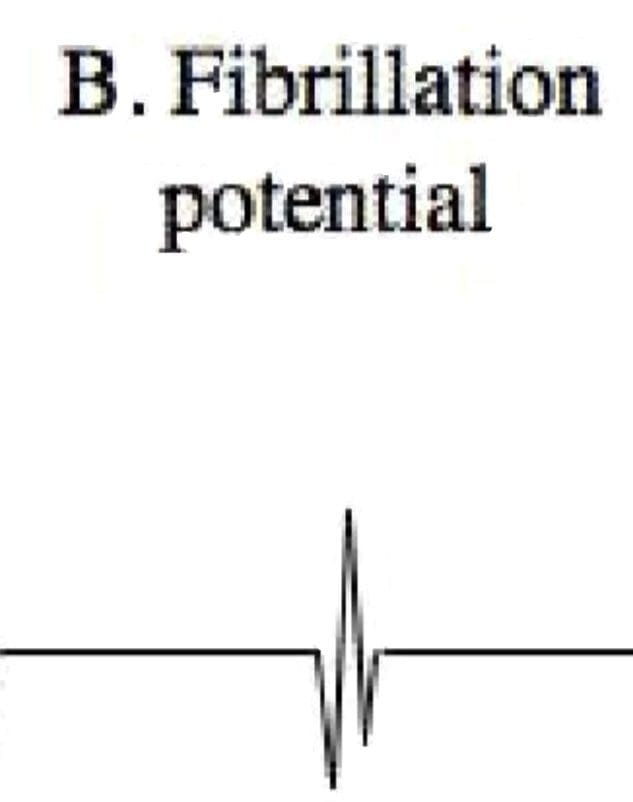
- Fibrillation potentials
Fibrillation Potentials
- DO NOT occur in normal muscle fibers
- Fibrillations cannot be seen with the naked eye but are detectable on EMG
- Often caused by nerve disease, but can be produced by severe muscle diseases if there is damage to the motor axons
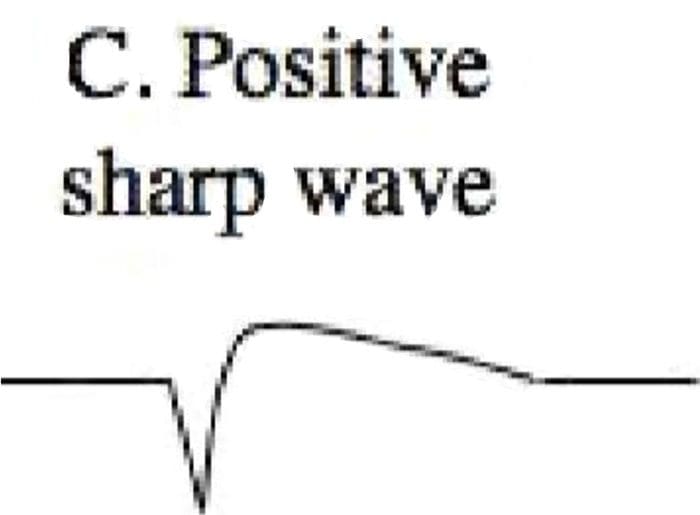
 Positive Sharp Waves
Positive Sharp Waves
- DO NOT occur in normally functioning fibers
- Spontaneous depolarization due to increased resting membrane potential
 Abnormal Findings
Abnormal Findings
- Findings of fibrillations and positive sharp waves are the most reliable indicator of damage to motor axons to the muscle after one week up to 12 months after the damage
- Often termed “acute” in reports, despite possibly being visible months after onset
- Will disappear if there is complete degeneration or denervation of nerve fibers
Nerve Conduction Velocity (NCV) Studies
Motor
- Measures compound muscle action potentials (CMAP)
Sensory
- Measures sensory nerve action potentials (SNAP)
Nerve Conduction Studies
- Velocity (Speed)
- Terminal latency
- Amplitude
- Tables of normal, adjusted for age, height and other factors are available for practitioners to make comparison
Terminal Latency
- Time between stimulus and the appearance of a response
- Distal entrapment neuropathies
- Increased terminal latency along a specific nerve pathway
Velocity
Calculated based on latency and variables such as distance
Dependent on diameter of axon
Also dependent on thickness of myelin sheath
- Focal neuropathies thin myelin sheaths, slowing conduction velocity
- Conditions such as Charcot Marie Tooth Disease or Guillian Barre Syndrome damage myelin in large diameter, fast conducting fibers
Amplitude
- Axonal health
- Toxic neuropathies
- CMAP and SNAP amplitude affected
Diabetic Neuropathy
Most common neuropathy
- Distal, symmetric
- Demyelination and axonal damage therefore speed and amplitude of conduction are both affected
Evoked Potential Studies
Somatosensory evoked potentials (SSEPs)
- Used to test sensory nerves in the limbs
Visual evoked potentials (VEPs)
- Used to test sensory nerves of the visual system
Brainstem auditory evoked potentials (AEPs)
- Used to test sensory nerves of the auditory system
Potentials recorded via low-impedance surface electrodes
Recordings averaged after repeated exposure to sensory stimulus
- Eliminates background “noise”
- Refines results since potentials are small and difficult to detect apart from normal activity
- According to Dr. Swenson, in the case of SSEPs, at least 256 stimuli are usually needed in order to obtain reliable, reproducible responses
Somatosensory Evoked Potentials (SSEPs)
Sensation from muscles
- Touch and pressure receptors in the skin and deeper tissues
Little if any pain contribution
- Limits ability to use testing for pain disorders
Velocity and/or amplitude changes can indicate pathology
- Only large changes are significant since SSEPs are normally highly variable
Useful for intraoperative monitoring and to assess the prognosis of patients suffering severe anoxic brain injury
- Not useful in assessing radiculopathy as individual nerve roots cannot be easily identified
Late Potentials
Occur more than 10-20 milliseconds after stimulation of motor nerves
Two types
- H-Reflex
- F-Response
H-Reflex
Named for Dr. Hoffman
- First described this reflex in 1918
Electrodiagnostic manifestation of myotatic stretch reflex
- Motor response recorded after electrical or physical stretch stimulation of the associated muscle
Only clinically useful in assessing S1 radiculopathy, as the reflex from the tibial nerve to triceps surae can be assessed for velocity and amplitude
- More quantifiable that Achilles reflex testing
- Fails to return with after damage and therefore not as clinically useful in recurrent radiculopathy cases
F-Response
So named because it was first recorded in the foot
Occurs 25 -55 milliseconds after initial stimulus
Due to antidromic depolarization of the motor nerve, resulting in a orthodromic electrical signal
- Not a true reflex
- Results in a small muscle contraction
- Amplitude can be highly variable, so not as important as velocity
- Reduced velocity indicates slowed conduction
Useful in assessing proximal nerve pathology
- Radiculopathy
- Guillian Barre Syndrome
- Chronic Inflammatory Demyelinating Polyradiculopathy (CIDP)
Useful in assessing demyelinative peripheral neuropathies
Sources
- Alexander G. Reeves, A. & Swenson, R. Disorders of the Nervous System. Dartmouth, 2004.
- Day, Jo Ann. “Neuroradiology | Johns Hopkins Radiology.” Johns Hopkins Medicine Health Library, 13 Oct. 2016, www.hopkinsmedicine.org/radiology/specialties/ne uroradiology/index.html.
- Swenson, Rand. Electrodiagnosis.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card