Muscle wasting is a prevalent finding in multiple chronic diseases, and it affects almost 70% of the patients suffering from end-stage renal disease (ESRD). The detrimental effect of low muscle mass is associated with higher mortality rates, and its finding depends on body composition evaluation. Nevertheless, body mass index (BMI), the most common measurement related to health status, cannot determine muscle mass or adipose tissue quantity. Therefore, BMI is a non-specific nutritional status marker for chronic kidney disease (CKD).
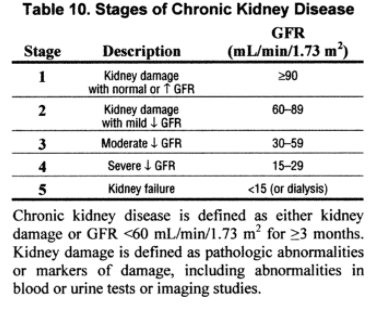
The KDOQI guidelines classify the presence of kidney disease by stages, the damage, and level of kidney function (glomerular rate, GFR).
Table of Contents
Stages of CKD, KDOQI guidelines.
CKD and Body composition
The physiological changes that come with the pathogenesis of CDK affect the patient in a multifactorial manner, being body composition one of these factors. Nevertheless, a body’s functional structure going through this pathological process reflects higher morbidity and mortality rates. Therefore, acquiring knowledge about the body composition changes in this process can help reverse and prevent the functional derangements that result from the loss of protein structures, such as muscle.
Protein-energy wasting
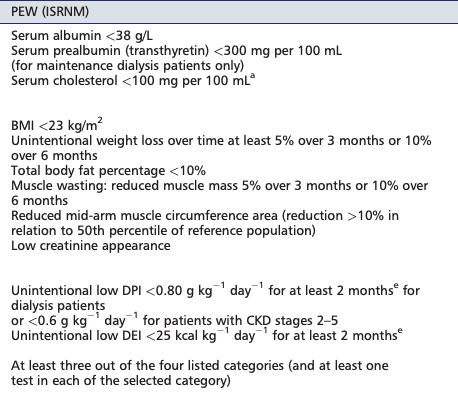
Protein-energy wasting syndrome (PEW) is commonly interchanged in the literature with cachexia, malnutrition, protein-energy malnutrition, and malnutrition-inflammation atherosclerosis. The PEW term is new in nutrition, and it was initially introduced in 2007 by the International Society on Renal Nutrition and Metabolism. Besides, PEW has a reported incidence of 11-54% in patients with stage 3-5 CKD and up to 80% in those treated with hemodialysis.
As mentioned before, the usage of different terms to diagnose PEW played a part in the definition process.
PEW: is a state of nutritional and metabolic derangements in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD) characterized by the simultaneous loss of systemic body protein and energy stores.
Since the malnutrition and PEW phenotype can be similar in patients with CKD, distinguishing clinical differences is essential to the practitioner. Nevertheless, the differences may provide better clinical treatment to reverse this condition.
The etiology of PEW is related to the hypercatabolic state induced by uremia, resulting in increased energy expenditure and acidosis. Besides, CKD patients often develop anorexia due to a poor appetite, inflammation due to chronic conditions such as diabetes, and autoimmune disorders that further add to ESRD development.
The hyper-catabolism of muscle and fat interacts with the decreased nutritional intake, loss of nutrients (via hemodialysis), loss of physical activity leading to frailty and inflammation are all contributing factors of PEW.
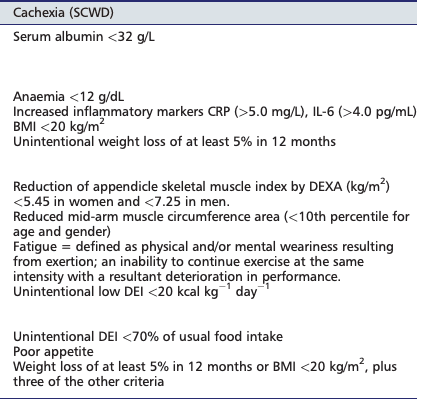
Cachexia
Cachexia is yet another term that is used as a generic state in CKD pathology. Similar to PEW, cachexia is also a new term. The Society first published it on Sarcopenia, Cachexia, and Wasting disorders in 2008.
Cachexia: a complex metabolic syndrome associated with underlying illness and characterized by a loss of muscle, with or without fat loss.
However, revisions on this definition by the International Society of Renal Nutrition and Metabolism proposed a specific classification of uremia-induced wasting disorders in which cachexia was the most severe stage of PEW.
Criteria for clinical diagnosis of cachexia in adults with CKD (SCWD)
Sarcopenia
Sarcopenia is a progressive and generalized skeletal muscle disorder associated with an increased likelihood of adverse outcomes, including falls, fractures, physical disability, and mortality.
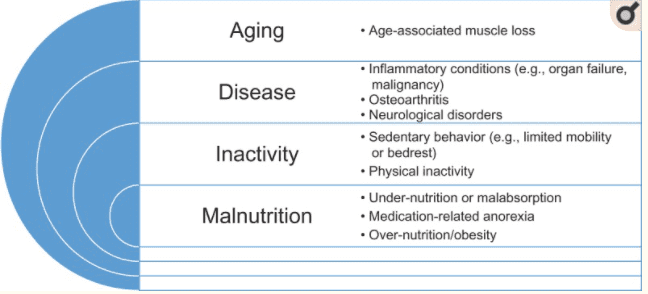
Nevertheless, muscle function is now part of sarcopenia’s diagnosis criteria. Therefore, muscle strength has become an essential factor in diagnosing this condition since it predicts adverse outcomes more accurately. Also, low muscle quality and quantity and low physical performance form part of sarcopenia’s actual definition. Furthermore, probable sarcopenia is identified if the patient presents low muscle strength. However, to diagnose sarcopenia, it is necessary to identify low muscle quality or quantity. Lastly, severe sarcopenia is considered when low muscle strength, low muscle quality, and quantity are accompanied by low physical performance.
Body composition measurements
The tools to identify the body composition, muscle quality, and physical performance are varied and depend on the clinical setting, technical resources, or the mobility of the patient in which the studies have been performed. Besides, sarcopenia has been commonly linked to the elderly population. Similarly, cachexia has been broadly studied in the elderly and cancer settings, CKD, long-term hospitalized patients, and malnutrition. On the other hand, PEW is commonly reported in the CKD population.
When diagnosing and tracking muscle quantity or muscle mass loss, a variety of assessments have been proposed. Body composition assessments such as DXA, magnetic resonance imaging (MRI), biopsy, computed tomography (CT), and bioelectrical impedance analysis (BIA) are validated in the diagnosis and monitoring of muscle loss conditions with reproducible results. However, in a clinical setting, the BIA assessment is considered a cost-effective test since it is non-invasive, reproducible, and can monitor these conditions’ progression or rehabilitation.
Function, quality and quantity assessments: muscle
On the other hand, handgrip strength is used to measure, monitor, and diagnose low muscle strength. Also, hand-grip strength is a simple measurement, and it’s inexpensive. This assessment is performed with a calibrated handheld dynamometer; after this quick test, the results are compared with interpretative data from an appropriate reference population. Another used test for muscle strength is the chair rise test. This test focuses on the strength of the leg muscles instead of the hand. Nevertheless, this test measures strength and endurance. This test measures the amount of time needed to rise from a chair without using the patient’s arms in a 30-second interval.
Lastly, the 4-m walk can be easily used in a clinical setting. This test is used to measure physical performance, which involves the muscles and the peripheral nervous center and balance.
In conclusion, the growing evidence of body composition and diagnostic criteria muscle loss conditions allows healthcare professionals to assess and diagnose each disease. Nevertheless, the diagnosis should not be the last part of the treatment. The right treatment should accompany the diagnosis.
The growing prevalence of chronic conditions, their complications, and the aging population is changing the type of patients that were commonly seen in nutritional practice. The implementation of a body composition assessment that provides us with a better diagnosing tool is vital to determine the patient’s nutritional and anthropometric. In addition, these assessments can allow us to provide a better integral and patient-centered treatment. – Ana Paola R. Arciniega. Master in clinical nutrition.
References:
Cruz-Jentoft, Alfonso J et al. “Sarcopenia: revised European consensus on definition and diagnosis.” Age and aging vol. 48,1 (2019): 16-31. doi:10.1093/ageing/afy169
Hanna, Ramy M et al. “A Practical Approach to Nutrition, Protein-Energy Wasting, Sarcopenia, and Cachexia in Patients with Chronic Kidney Disease.” Blood purification vol. 49,1-2 (2020): 202-211. doi:10.1159/000504240
Koppe, Laetitia, et al. “Kidney cachexia or protein?energy wasting in chronic kidney disease: facts and numbers.” Journal of cachexia, sarcopenia and muscle 10.3 (2019): 479-484.
Additional Online Links & Resources (Available 24/7)
Online Appointments or Consultations: https://bit.ly/Book-Online-Appointment
Online Physical Injury / Accident Intake Form: https://bit.ly/Fill-Out-Your-Online-History
Online Functional Medicine Assessment: https://bit.ly/functionmed
Disclaimer
The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the musculoskeletal system’s injuries or disorders. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us 915-850-0900. Read More…
Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, CTG*
email: coach@elpasofunctionalmedicine.com
phone: 915-850-0900
Licensed in Texas & New Mexico
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


