Muscle Fasciculations:
Key indexing terms:
- Fasciculation
- muscular
- Gluten
- Celiac disease
- Chiropractic
- Food hypersensitivity
Abstract
Objective: The purpose of this case report is to describe a patient with chronic, multisite muscle fasciculations who presented to a chiropractic teaching clinic and was treated with dietary modifications.
Clinical features: A 28-year-old man had muscle fasciculations of 2 years. The fasciculations began in his eye and progressed to the lips and lower extremities. In addition, he had gastrointestinal distress and fatigue. The patient was previously diagnosed as having wheat allergy at the age of 24 but was not compliant with a gluten-free diet at that time. Food sensitivity testing revealed immunoglobulin G–based sensitivity to multiple foods, including many different grains and dairy products. The working diagnosis was gluten neuropathy.
Intervention and outcome: Within 6 months of complying with dietary restrictions based on the sensitivity testing, the patient’s muscle fasciculations completely resolved. The other complaints of brain fog, fatigue, and gastrointestinal distress also improved.
Conclusions: This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary changes. There is strong suspicion that this case represents one of gluten neuropathy, although testing for celiac disease specifically was not performed.
Table of Contents
Introduction: Muscle Fasciculations
 There are 3 known types of negative reactions to wheat proteins, collectively known as wheat protein reactivity: wheat allergy (WA), gluten sensitivity (GS), and celiac disease (CD). Of the 3, only CD is known to involve autoimmune reactivity, generation of antibodies, and intestinal mucosal damage. Wheat allergy involves the release of histamine by way of immunoglobulin (Ig) E cross-linking with gluten peptides and presents within hours after ingestion of wheat proteins. Gluten sensitivity is considered to be a diagnosis of exclusion; sufferers improve symptomatically with a gluten-free diet (GFD) but do not express antibodies or IgE reactivity.1
There are 3 known types of negative reactions to wheat proteins, collectively known as wheat protein reactivity: wheat allergy (WA), gluten sensitivity (GS), and celiac disease (CD). Of the 3, only CD is known to involve autoimmune reactivity, generation of antibodies, and intestinal mucosal damage. Wheat allergy involves the release of histamine by way of immunoglobulin (Ig) E cross-linking with gluten peptides and presents within hours after ingestion of wheat proteins. Gluten sensitivity is considered to be a diagnosis of exclusion; sufferers improve symptomatically with a gluten-free diet (GFD) but do not express antibodies or IgE reactivity.1
The reported prevalence of WA is variable. Prevalence ranges from 0.4% to 9% of the population.2,3 The prevalence of GS is somewhat difficult to determine, as it does not have a standard definition and is a diagnosis of exclusion. Gluten sensitivity prevalence of 0.55% is based on National Health and Nutrition Examination Survey data from 2009 to 2010.4 In a 2011 study, a GS prevalence of 10% was reported in the US population.5 In contrast to the above 2 examples, CD is well defined. A 2012 study examining serum samples from 7798 patients in the National Health and Nutrition Examination Survey database from 2009 to 2010 found an overall prevalence of 0.71% in the United States.6
Neurologic manifestations associated with negative reactions to wheat proteins have been well documented. As early as 1908, “peripheral neuritis” was thought to be associated with CD.7 A review of all published studies on this topic from 1964 to 2000 indicated that the most common neurologic manifestations associated with GS were ataxia (35%), peripheral neuropathy (35%), and myopathy (16%). 8 Headaches, paresthesia, hyporeflexia, weakness, and vibratory sense reduction were reported to be more prevalent in CD patients vs controls.9 These same symptoms were more prevalent in CD patients who did not strictly follow a GFD vs those who were compliant with GFD.
At present, there are no case reports describing the chiropractic management of patient with gluten neuropathy. Therefore, the purpose of this case study is to describe a patient presentation of suspected gluten neuropathy and a treatment protocol using dietary modifications.
Case Report
 A 28-year-old man presented to a chiropractic teaching clinic with complaints of constant muscle fasciculations of 2 years’ duration. The muscle fasciculations originally started in the left eye and remained there for about 6 months. The patient then noticed that the fasciculations began to move to other areas of his body. They first moved into the right eye, followed by the lips, and then to the calves, quadriceps, and gluteus muscles. The twitching would sometimes occur in a single muscle or may involve all of the above muscles simultaneously. Along with the twitches, he reports a constant “buzzing” or “crawling” feeling in his legs. There was no point during the day or night when the twitches ceased.
A 28-year-old man presented to a chiropractic teaching clinic with complaints of constant muscle fasciculations of 2 years’ duration. The muscle fasciculations originally started in the left eye and remained there for about 6 months. The patient then noticed that the fasciculations began to move to other areas of his body. They first moved into the right eye, followed by the lips, and then to the calves, quadriceps, and gluteus muscles. The twitching would sometimes occur in a single muscle or may involve all of the above muscles simultaneously. Along with the twitches, he reports a constant “buzzing” or “crawling” feeling in his legs. There was no point during the day or night when the twitches ceased.
The patient originally attributed the muscle twitching to caffeine intake (20 oz of coffee a day) and stress from school. The patient denies the use of illicit drugs, tobacco, or any prescription medication but does drink alcohol (mainly beer) in moderation. The patient ate a diet high in meats, fruits, vegetables, and pasta. Eight months after the initial fasciculations began, the patient began to experience gastrointestinal (GI) distress. Symptoms included constipation and bloating after meals. He also began to experience what he describes as “brain fog,” a lack of concentration, and a general feeling of fatigue. The patient noticed that when the muscle fasciculations were at their worst, his GI symptoms correspondingly worsened. At this point, the patient put himself on a strict GFD; and within 2 months, the symptoms began to alleviate but never completely ceased. The GI symptoms improved, but he still experienced bloating. The patient’s diet consisted mostly of meats, fruit, vegetables, gluten-free grains, eggs, and dairy.
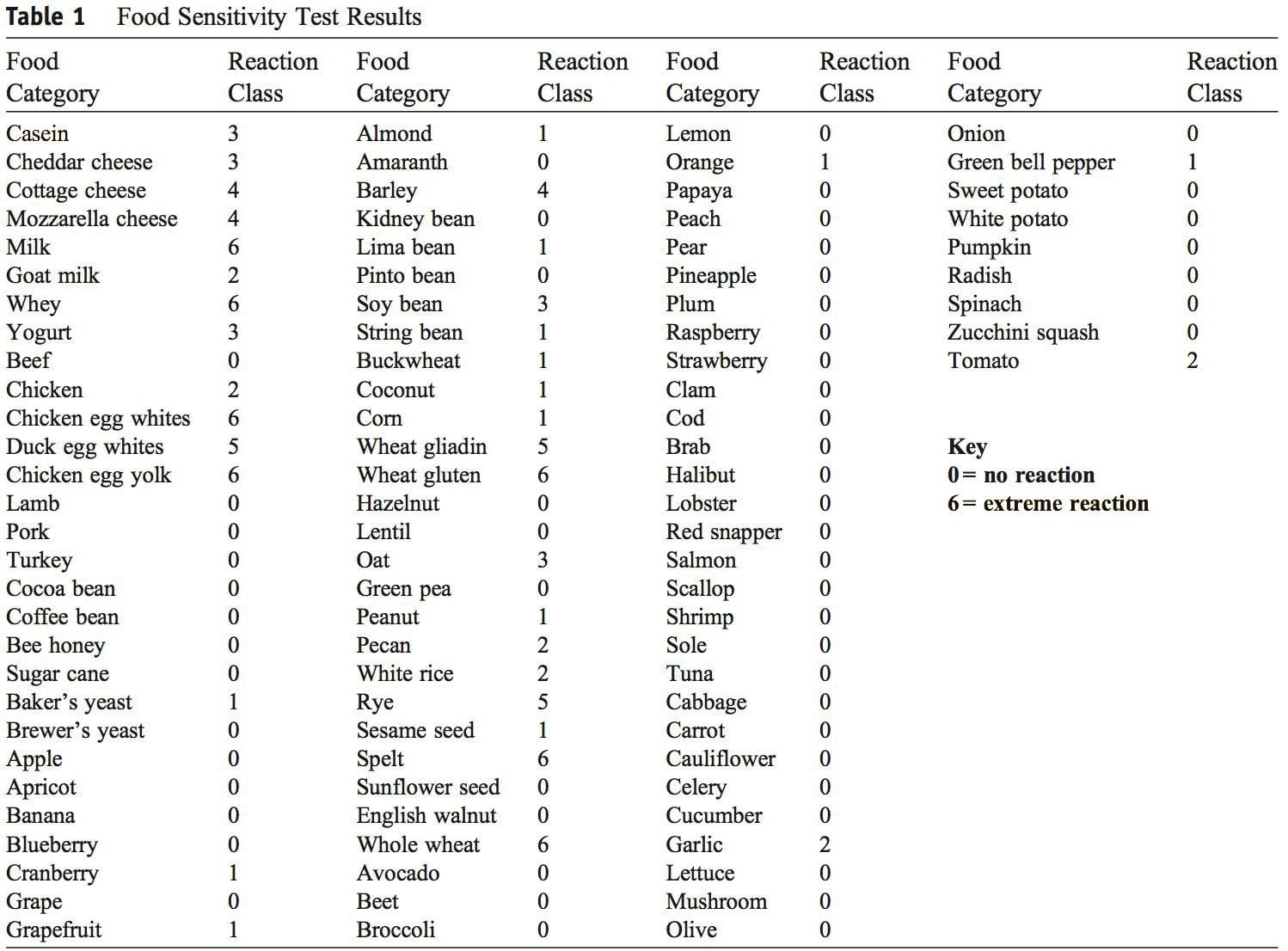
At the age of 24, the patient was diagnosed with WA after seeing his physician for allergies. Serum testing revealed elevated IgE antibodies against wheat, and the patient was advised to adhere to a strict GFD. The patient admits to not following a GFD until his fasciculations peaked in December 2011. In July of 2012, blood work was evaluated for levels of creatine kinase, creatine kinase–MB, and lactate dehydrogenase to investigate possible muscle breakdown. All values were within normal limits. In September of 2012, the patient under- went food allergy testing once again (US Biotek, Seattle, WA). Severely elevated IgG antibody levels were found against cow’s milk, whey, chicken egg white, duck egg white, chicken egg yolk, duck egg yolk, barley, wheat gliadin, wheat gluten, rye, spelt, and whole wheat (Table 1). Given the results of the food allergy panel, the patient was recommended to remove this list of foods from his diet. Within 6 months of complying with the dietary changes, the patient’s muscle fasciculations completely resolved. The patient also experienced much less GI distress, fatigue, and lack of concentration.
 Discussion
Discussion
 The authors could not find any published case studies related to a presentation such as the one described here. We believe this is a unique presentation of wheat protein reactivity and thereby represents a contribution to the body of knowledge in this field.
The authors could not find any published case studies related to a presentation such as the one described here. We believe this is a unique presentation of wheat protein reactivity and thereby represents a contribution to the body of knowledge in this field.
This case illustrates an unusual presentation of a widespread sensorimotor neuropathy that seemed to respond to dietary changes. Although this presentation is consistent with gluten neuropathy, a diagnosis of CD was not investigated. Given the patient had both GI and neurologic symptoms, the likelihood of gluten neuropathy is very high.
There are 3 forms of wheat protein reactivity. Because there was confirmation of WA and GS, it was decided that testing for CD was unnecessary. The treatment for all 3 forms is identical: GFD.
The pathophysiology of gluten neuropathy is a topic that needs further investigation. Most authors agree it involves an immunologic mechanism, possibly a direct or indirect neurotoxic effect of antigliadin anti- bodies. 9,10 Briani et al 11 found antibodies against ganglionic and/or muscle acetylcholine receptors in 6 of 70 CD patients. Alaedini et al12 found anti-ganglioside antibody positivity in 6 of 27 CD patients and proposed that the presence of these antibodies may be linked to gluten neuropathy.
It should also be noted that both dairy and eggs showed high responses on the food sensitivity panel. After reviewing the literature, no studies could be located linking either food with neuromuscular symp- toms consistent with the ones presented here. There- fore, it is unlikely that a food other than gluten was responsible for the muscle fasciculations described in this case. The other symptoms described (fatigue, brain fog, GI distress) certainly may be associated with any number of food allergies/sensitivities.
Limitations
One limitation in this case is the failure to confirm CD. All symptoms and responses to dietary change point to this as a likely possibility, but we cannot confirm this diagnosis. It is also possible that the symptomatic response was not due directly to dietary change but some other unknown variable. Sensitivity to foods other than gluten was documented, including reactions to dairy and eggs. These food sensitivities may have contributed to some of the symptoms present in this case. As is the nature of case reports, these results cannot necessarily be generalized to other patients with similar symptoms.
Conclusion: Muscle Fasciculations
 This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary change. There is strong suspicion that this case represents one of gluten neuropathy, although testing for CD specifically was not performed.
This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary change. There is strong suspicion that this case represents one of gluten neuropathy, although testing for CD specifically was not performed.
Brian Anderson DC, CCN, MPHa,?, Adam Pitsinger DCb
Attending Clinician, National University of Health Sciences, Lombard, IL Chiropractor, Private Practice, Polaris, OH
Acknowledgment
This case report is submitted as partial fulfillment of the requirements for the degree of Master of Science in Advanced Clinical Practice in the Lincoln College of Post-professional, Graduate, and Continuing Education at the National University of Health Sciences.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References:
1. Sapone A, Bai J, Ciacci C, et al. Spectrum of gluten-related
disorders: consensus on new nomenclature and classification.
BMC Med 2012;10:13.
2. Matricardi PM, Bockelbrink A, Beyer K, et al. Primary versus
secondary immunoglobulin E sensitization to soy and wheat in
the Multi-Centre Allergy Study cohort. Clin Exp Allergy
2008;38:493–500.
3. Vierk KA, Koehler KM, Fein SB, Street DA. Prevalence of
self-reported food allergy in American adults and use of food
labels. J Allergy Clin Immunol 2007;119:1504–10.
4. DiGiacomo DV. Prevalence and characteristics of non-celiac
gluten sensitivity in the United States: results from the
continuous National Health and Nutrition Examination Survey
2009-2010. Presented at: the 2012 American College of
Gastroenterology Annual Scientific Meeting; Oct. 19-24, Las
Vegas.; 2012.
5. Sapone A, Lammers KM, Casolaro V. Divergence of gut
permeability and mucosal immune gene expression in two
gluten-associated conditions: celiac disease and gluten sensitivity.
BMC Med 2011;9:23.
6. Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA,
Everhart JE. The prevalence of celiac disease in the United
States. Am J Gastroenterol 2012 Oct;107(10):1538–44.
7. Hadjivassiliou M, Grunewald RA, Davies-Jones GAB. Gluten
sensitivity as a neurological illness. J Neurol Neurosurg
Psychiatr 2002;72:560–3.
8. Hadjivassiliou M, Chattopadhyay A, Grunewald R, et al.
Myopathy associated with gluten sensitivity. Muscle Nerve
2007;35:443–50.
9. Cicarelli G, Della Rocca G, Amboni C, et al. Clinical and
neurological abnormalities in adult celiac disease. Neurol Sci
2003;24:311–7.
10. Hadjivassiliou M, Grunewald RA, Kandler RH. Neuropathy
associated with gluten sensitivity. J Neurol Neurosurg
Psychiatry 2006;77:1262–6.
11. Briani C, Doria A, Ruggero S, et al. Antibodies to muscle and
ganglionic acetylcholine receptors in celiac disease. Autoimmunity
2008;41(1):100–4.
12. Alaedini A, Green PH, Sander HW, et al. Ganglioside reactive
antibodies in the neuropathy associated with celiac disease.
J Neuroimmunol 2002;127(1–2):145–8.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


