Medial tibial stress syndrome, commonly referred to as shin splints, is not considered to be a medically serious condition, however, it can challenge an athlete’s performance. Approximately 5 percent of all sports injuries are diagnosed as medial tibial stress syndrome, or MTSS for short.

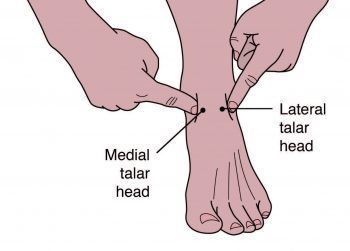
Shin splints, or MTSS, occurs most frequently in specific groups of the athletic population, accounting for 13-20 percent of injuries in runners and up to 35 percent in military service members. Medial tibial stress syndrome is characterized as pain along the posterior-medial border of the lower half of the tibia, which is active during exercise and generally inactive during rest. Athletes describe feeling discomfort along the lower front half of the leg or shin. Palpation along the medial tibia can usually recreate the pain.
Table of Contents
Causes of Medial Tibial Stress Syndrome
There are two main speculated causes for medial tibial stress syndrome. The first is that contracting leg muscles place a repeated strain upon the medial portion of the tibia, producing inflammation of the periosteal outer layer of bone, commonly known as periostitis. While the pain of a shin splint is felt along the anterior leg, the muscles located around this region are the posterior calf muscles. The tibialis posterior, flexor digitorum longus, and the soleus all emerge from the posterior-medial section of the proximal half of the tibia. As a result, the traction force from these muscles on the tibia probably aren’t the cause of the pain generally experienced on the distal portion of the leg.
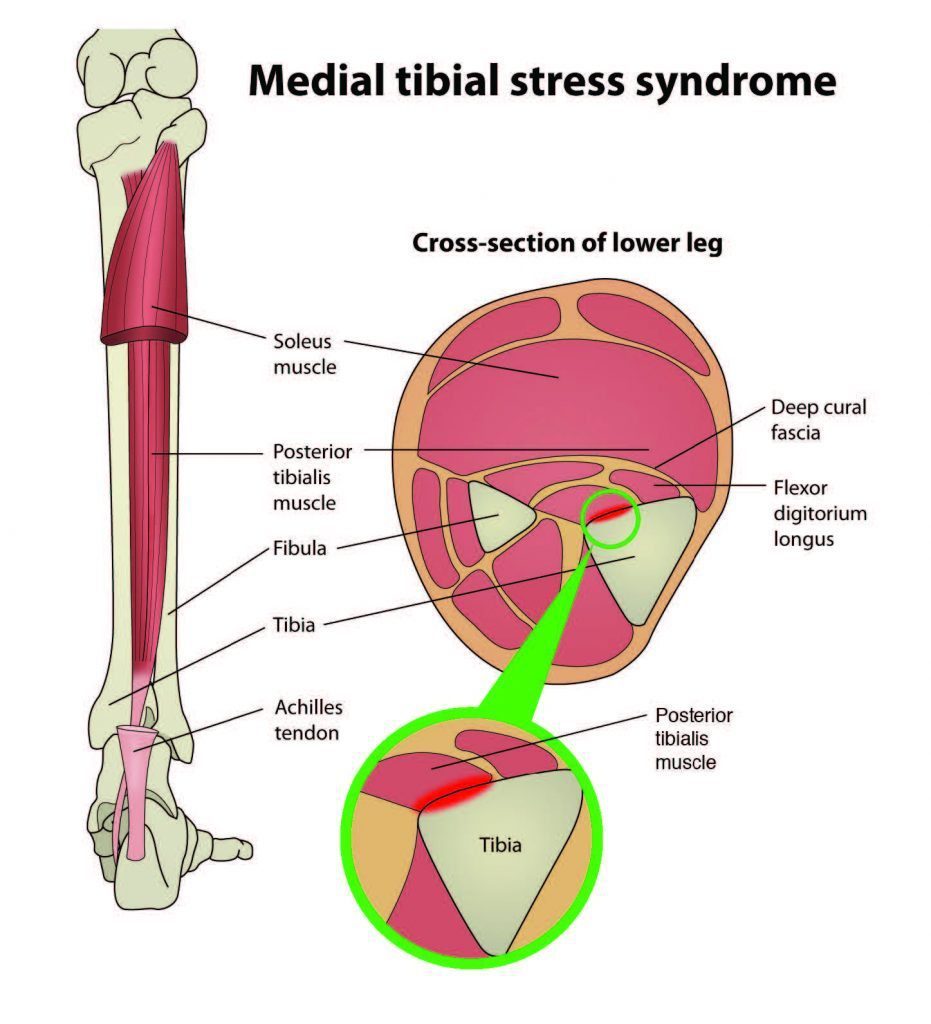
Another theory of this tension is that the deep crural fascia, or the DCF, the tough, connective tissue which surrounds the deep posterior muscles of the leg, may pull excessively on the tibia, causing trauma to the bone. Researchers at the University of Honolulu evaluated a single leg from 5 male and 11 female adult cadavers. Through the study, they confirmed that in these specimens, the muscles of the posterior section of muscles was introduced above the portion of the leg that is usually painful in medial tibial stress syndrome and the deep crural fascia did indeed attach on the entire length of the medial tibia.
Doctors at the Swedish Medical Centre in Seattle, Washington believed that, given the anatomy, the tension from the posterior calf muscles could produce a similar strain on the tibia at the insertion of the DCF, causing injury.
In a laboratory study conducted using three fresh cadaver specimens, researchers concluded that strain at the insertion site of the DCF along the medial tibia advanced linearly as tension increased in the posterior leg muscles. The study confirmed that an injury caused by tension at the medial tibia was possible. However, studies of bone periosteum on individuals with MTSS have yet to find inflammatory indicators to confirm the periostitis theory.
The second theory believed to cause medial tibial stress syndrome is that repetitive or excessive loading may cause a bone-stress reaction in the tibia. When the tibia is unable to properly bear the load being applied against it, it will bend during weight bearing. The overload results in micro damage within the bone, not just along the outer layer. If the repetitive loading exceeds the bone’s ability to repair, localized osteopenia can occur. Because of this, some researchers consider a tibial stress fracture to be the result of a continuum of bone stress reactions that include MTSS.
Utilizing magnetic resonance imaging, or MRI, on the affected leg can often display bone marrow edema, periosteal lifting, and areas of increased bony resorption in athletes with medial tibial stress syndrome. This supports the bone-stress reaction theory. An MRI of an athlete with a diagnosis of MTSS can also help rule out other causes of lower leg pain, such as a tibial stress fracture, deep posterior compartment syndrome, and popliteal artery entrapment syndrome.
Risk factors for MTSS
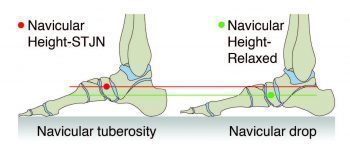
While the cause, set of causes or manner of causation of MTSS is still only a hypothesis, the risk factors for athletes developing it are well-known. As determined by the navicular drop test, or NDT, a large navicular drop considerably corresponds with a diagnosis of medial tibial stress syndrome. The NDT measures the difference in height position of the navicular bone, from a neutral subtalar joint position in supported non-weight bearing, to full weight bearing. The NDT explains the degree of arch collapse during weight bearing. Results of more than 10 mm is considered excessive and can be a considerable risk factor for the development of MTSS.
Research studies have proposed that athletes with MTSS are most frequently female, have a higher BMI, less running experience, and a previous history of MTSS. Running kinematics for females can be different from that of males and has often been demonstrated to leave individuals vulnerable to suffer anterior cruciate ligament tears and patellofemoral pain syndrome. This same biomechanical pattern may also incline females to develop medial tibial stress syndrome. Hormonal considerations and low bone density are believed to be contributing factors, increasing the risk of MTSS in the female athlete as well.
A higher BMI in an athlete demonstrates that they have more muscle mass rather than being overweight. The end result, however, is the same in that the legs bear a considerably heavy load. It’s been hypothesized that in these cases, the bone growth accelerated by the tibial bowing may not advance quickly enough and injury to the bone may occur. Therefore, those with a higher BMI may need to continue their training programs gradually in order to allow the body to adapt accordingly.
Athletes with less running experience are more likely to make training errors, which may be a common cause for medial tibial stress syndrome. These include but are not limited to: increasing distance too quickly, changing terrain, overtraining, poor equipment or footwear, etc. Inexperience may also lead the athlete to return to activity before the recommended time, accounting for the higher prevalence of MTSS in those who had previously experienced MTSS. A complete recovery from MTSS can take from six months up to ten months, and if the original injury does not properly heal or the athlete returns to training too soon, chances are, their pain and symptoms may return promptly.
Biomechanical Analysis
The NDT is used as a measurable indication of foot pronation. Pronation is described as a tri-planar movement consisting of eversion at the hindfoot, abduction of the forefoot and dorsiflexion of the ankle. Pronation is a normal movement of the body and it is absolutely essential in walking and running. When the foot impacts the ground at the initial contact phase of running, the foot begins to pronate and the joints of the foot acquire a loose-packed position. This flexibility helps the foot absorb ground reaction forces.
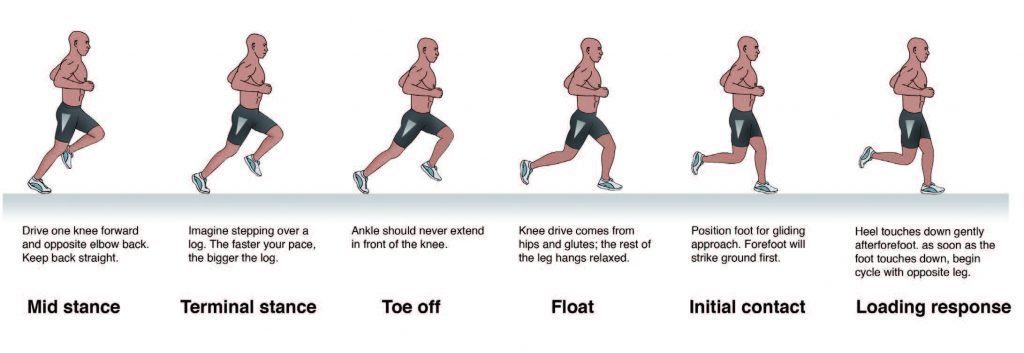
During the loading response phase, the foot further pronates, reaching peak pronation by approximately 40 percent during stance phase. In mid stance, the foot moves out of pronation and back to a neutral position. During terminal stance, the foot supinates, moving the joints into a fastened position, creating a rigid lever arm from which to generate the forces for toe off.
Starting with the loading response phase and throughout the rest of the single leg stance phase of running, the hip is stabilized and supported as it is extended, abducted and externally rotated by the concentric contraction of the hip muscles of the stance leg, including the gluteals, piriformis, obturator internus, superior gemellus and inferior gemellus. Weakness or fatigue in any of these muscles can develop an internal rotation of the femur, adduction of the knee, internal rotation of the tibia, and over-pronation. Overpronation therefore, can be a result of muscle weakness or fatigue. If this is the case, the athlete may have a completely normal NDT and yet, when the hip muscles don’t function as needed, these can overpronate.
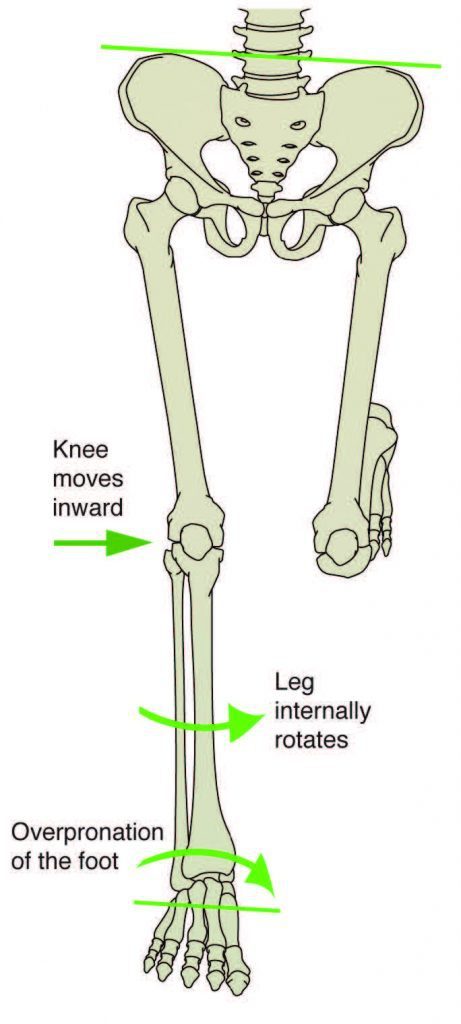
In a runner who has considerable overpronation, the foot may continue to pronate into mid stance, resulting in a delayed supination response, causing for there to be less power generation at toe off. The athlete can make the effort to apply two biomechanical fixes here that could contribute to the development of MTSS. First of all, the tibialis posterior will strain to prevent the overpronation. This can add tension to the DCF and strain the medial tibia. Second, the gastroc-soleus complex will contract more forcefully at toe off to improve the generation of power. However, it’s hypothesized that the increased force within these muscle groups can add further tension to the medial tibia through the DCF and possibly irritate the periosteum.
Evaluating Injury in Athletes
Once understood that overpronation is one of the leading risk factors for medial tibial stress syndrome, the athlete should begin their evaluation slowly and gradually progress through the procedure. Foremost, the NDT must be performed, making sure if the difference is more than 10mm. Then, it’s essential to analyze the athlete’s running gait on a treadmill, preferably when the muscles are fatigued, such as at the end of a training run. Even with a normal NDT, there may be evidence of overpronation in running.
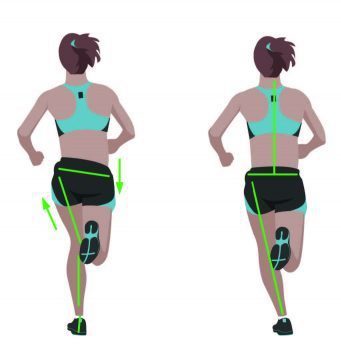
Next, the athlete’s knee should be evaluated accordingly. The specialist performing the evaluation should note whether the knee is adducted, whether the hip is leveled or if either hip is more than 5 degrees from level. These can be clear indications that there is probably weakness at the hip. Traditional muscle testing may not reveal the weakness; therefore, functional muscle testing may be required.
Additionally, it should be observed whether the athlete can perform a one-legged squat with arms in and arms overhead. The specialist must also note if the hip drops, the knee adducts and the foot pronates. Furthermore, the strength of the hip abductors should be tested in side lying, with the hip in a neutral, extended, and flexed position, making sure the knee is straight. All three positions with the hip rotated in a neutral position and at end ranges of external and internal rotation should also be tested. Hip extensions in prone with the knee straight and bent, in all three positions of hip rotation: external, neutral and internal can also be analyzed and observed to determine the presence of medial tibial stress syndrome, or MTSS. The position where a healthcare professional finds weakness after the evaluation is where the athlete should begin strengthening activities.

Treating the Kinetic Chain
In the presence of hip weakness, the athlete should begin the strengthening process by performing isometric exercises in the position of weakness. For example, if there is weakness during hip abduction with extension, then the athlete should begin isolated isometrics in this position. Until the muscles consistently activate isometrically in this position for 3 to 5 sets of 10 to 20 seconds should the individual progress to adding movement. Once the athlete achieves this level, begin concentric contractions, in that same position, against gravity. Some instances are unilateral bridging and side lying abduction. Eccentric contractions should follow, and then sport specific drills.
In the case that other biomechanical compensations occur, these must also be addressed accordingly. If the tibialis posterior is also displaying weakness, the athlete should begin strengthening exercises in that area. If the calf muscles are tight, a stretching program must be initiated. Utilizing any modalities possible might be helpful towards the rehabilitation process. Last but not least, if the ligaments in the foot are over stretches, the athlete should consider stabilizing footwear. Using a supported shoe for a temporary period of time during rehabilitation can be helpful to notify the athlete to embrace new movement patterns.
MTSS and Sciatica
Medial tibial stress syndrome, otherwise known as shin splints, ultimately is a painful condition that can greatly restrict an athlete’s ability to walk or run. As mentioned above, several evaluations can be performed by a healthcare professional to determine the presence of MTSS in an athlete, however, other conditions aside from shin splints may be causing the individuals leg pain and hip weakness. That is why it’s important to also visit additional specialists to ensure the athlete has received the correct diagnosis for their injuries or conditions.
Sciatica is best referred to as a set of symptoms that originate from the lower back and is caused by an irritation of the sciatic nerve. The sciatic nerve is the single, largest nerve in the human body, communicating with many different areas of the upper and lower leg. Because leg pain can occur without the presence of low back pain, an athlete’s medial tibial stress syndrome could really be sciatica originating from the back. Most commonly, MTSS can be characterized by pain that is generally worse when walking or running while sciatica is generally worse when sitting with an improper posture.
Regardless of the symptoms, it’s essential for an athlete to seek proper diagnosis to determine the cause of their pain and discomfort. Chiropractic care is a popular form of alternative treatment which focuses on musculoskeletal injuries and conditions as well as nervous system disorders. A chiropractor can help diagnose an athlete’s MTSS as well as overrule the presence of sciatica as a cause of the symptoms. In addition, chiropractic care can help restore and improve an athlete’s performance. By utilizing careful spinal adjustments and manual manipulations, a chiropractor can help strengthen the structures of the body and increase the individual’s mobility and flexibility. After suffering an injury, an athlete should receive the proper care and treatment they need and require to return to their specific sport activity as soon as possible.
Chiropractic and Athletic Performance
.video-container{position: relative; padding-bottom: 63%; padding-top: 35px; height: 0; overflow: hidden;}.video-container iframe{position: absolute; top:0; left: 0; width: 100%; height: 100%; border: none; max-width:100%!important;}
In conclusion, the best way to prevent pain from MTSS is to decrease the athlete’s risk factors. An athlete should have a basic running gait analysis and proper shoe fitting as well as include hip strengthening in functional positions as part of the strengthening program. Furthermore, one must ensure the athletes fully rehabilitate before returning to play because the chances of recurrence of medial tibial stress syndrome can be high.
For more information, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 . 
By Dr. Alex Jimenez
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


