Individuals with plantar fasciitis may experience consistent flare-ups. Can knowing the causes help to find pain relief?
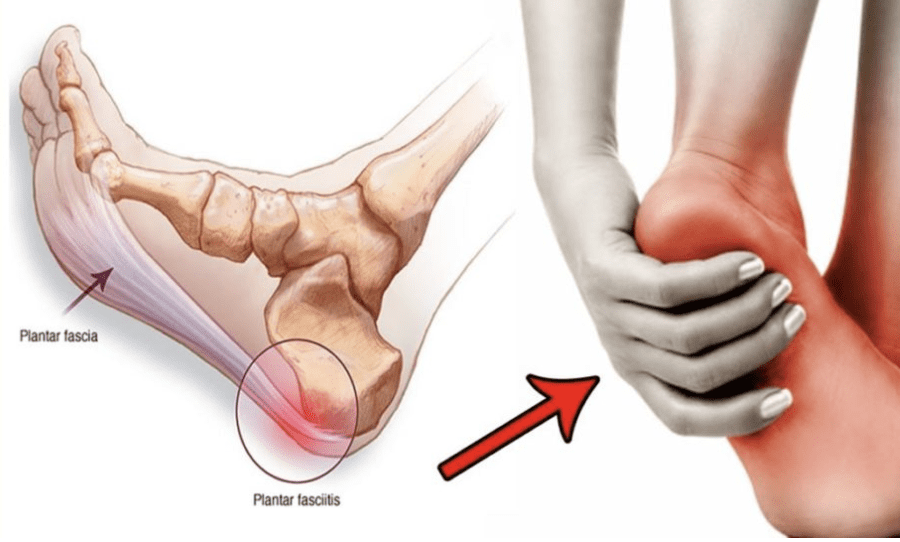
Table of Contents
Plantar Fasciitis Flare-Up
Plantar fasciitis is a common cause of heel and foot pain. The plantar fascia is a band of tissue that runs along the bottom of the foot and becomes inflamed. Certain factors can cause plantar fasciitis flare-ups, including:
- Increased levels of physical activity.
- Not stretching regularly.
- Wearing shoes without proper support.
- Weight gain.
Causes
A plantar fasciitis flare-up is often triggered by physical activity. (MedlinePlus. U.S. National Library of Medicine. 2022) It can also be brought on by underlying conditions, like increased body weight, arthritis, or the shape of the foot. (Johns Hopkins Medicine. 2023) Despite the root cause, there are activities and experiences that can contribute to and/or worsen the condition.
New Exercise Routine
- Being highly physically active can exacerbate plantar fasciitis symptoms.
- A plantar fasciitis flare-up can happen after a sudden increase in activity, like starting a new exercise program or adding new exercises to a routine. (MedlinePlus. U.S. National Library of Medicine. 2022)
- Walking or running on uneven surfaces or downhill can be a trigger. (Johns Hopkins Medicine. 2023)
- Minimizing physical activity and time standing can help.
- If this is not possible, wearing cushioned shoes with arch support can help minimize pain. (Johns Hopkins Medicine. 2023)
Weight Gain
- Individuals who have an increased or increasing body weight add more pressure to their feet, placing them at higher risk for plantar fasciitis. (MedlinePlus. U.S. National Library of Medicine. 2022)
- If experiencing consistent flare-ups, a healthcare provider may suggest an appropriate weight loss program combined with a treatment plan.
Pregnancy
- Rapid weight gain can cause a plantar fasciitis flare-up, including during pregnancy. (Boston Children’s Hospital. 2023)
Shoes Without Support
- Wearing shoes without arch support can cause general foot pain and plantar flare-ups.
- Individuals should wear shoes with plenty of cushioning and arch support, like sneakers. (Ortho Info. Academy of Orthopaedic Surgeons. 2022)
- Shoes that are not recommended include:
- Flip-flops
- Shoes that are flat.
- High heels, boots, or shoes that raise the heel above the toes.
- Worn-out shoes like exercise workout shoes.
Not Stretching Properly or At All
- Tight calves can increase pressure on the plantar fascia.
- Stretching the calves, Achilles tendon/heel, and the bottom of the feet is highly recommended to help treat and prevent the condition. (Johns Hopkins Medicine. 2023)
- Not stretching thoroughly or skipping stretches can worsen symptoms.
- Individuals with plantar fasciitis are recommended to stretch before and after physical activities, exercise, before going to bed, and after waking up.
Working Through the Pain
- Individuals may try to continue physical activities during a flare-up.
- This is not recommended as doing so can cause more pain and worsen the condition.
- When pain presents, it’s recommended to:
- Stop all activities that strain the feet
- Stay off the feet for at least a week.
Tearing the Plantar Fascia
- The plantar fascia rarely tear completely from repeated stress known as a plantar fascia rupture.
- If this happens, sudden severe pain will present and individuals are advised to call their healthcare provider. (Stephanie C. Pascoe, Timothy J. Mazzola. 2016)
- However, individuals can recover relatively fast, and pain alleviates quickly.
- Individuals with tears will be recommended to wear a foot orthotic as the foot may have flattened more.
Risk Factors
Plantar fasciitis can happen to anyone, but individuals who have the following characteristics are at an increased risk: (Ortho Info. Academy of Orthopaedic Surgeons. 2022)
- A high-foot arch.
- Jobs or hobbies that place added strain on the feet.
- Tight calf muscles.
- A sudden increase in physical activity.
- A new exercise regimen.
- Increased body weight.
- Sudden weight gain like during pregnancy.
How Long Does a Flare Last?
- Plantar fasciitis can become chronic if untreated.
- With treatment, 90% of cases will improve within 10 months. (Ortho Info. Academy of Orthopaedic Surgeons. 2022)
- During a flare-up, stay off the feet as much as possible.
Treatment
In addition to rest treatments for plantar fasciitis can include: (Ortho Info. Academy of Orthopaedic Surgeons. 2022)
Ice
- Icing the bottom of the foot for 15 minutes a few times a day decreases inflammation.
Nonsteroidal anti-inflammatory drugs – NSAIDs
- Over-the-counter NSAIDs like ibuprofen and naproxen, can reduce pain and inflammation.
- It is recommended to consult a healthcare provider for short-term use and dosage.
Proper Shoes
- Shoes with arch supports are highly recommended.
- A healthcare provider can order custom orthotics for more support.
Stretching
- Stretches are essential for treatment.
- Stretching the calf and bottom of the foot daily will keep the tissue relaxed.
Massages
- Massaging the area with a therapeutic massage ball soothes the tissues.
- Using a percussive massager can increase circulation.
What is Plantar Fasciitis?
References
MedlinePlus. National Library of Medicine. (2022) U.S. Plantar fasciitis.
Johns Hopkins Medicine. (2023) Plantar fasciitis.
Boston Children’s Hospital. (2023) Plantar fasciitis.
Ortho Info. Academy of Orthopaedic Surgeons. (2022) Plantar fasciitis and bone spurs.
Pascoe, S. C., & Mazzola, T. J. (2016). Acute Medial Plantar Fascia Tear. The Journal of orthopaedic and sports physical therapy, 46(6), 495. https://doi.org/10.2519/jospt.2016.0409
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


