Table of Contents
Degenerative Knee Arthritis
- Knee Arthritis
- Knee OA (arthrosis) is the m/c symptomatic OA with 240 cases per 100,000, 12.5% of people >45 y.o.
- Modifiable risk factors: trauma, obesity, lack of fitness, muscle weakness
- Non-modifiable: women>men, aging, genetics, race/ethnicity
- Pathology:
disease of the articular cartilage. Continuing mechanical stimulation follows byinitial increase in water and cartilage thickness. Gradual loss of proteoglycans and ground substance. Fissuring/splitting. Chondrocytes are damaged and release enzymes into the joint. Cystic progression and further cartilage loss. Subchondral bone is denuded and exposed to mechanical stresses. It becomes hypervascular forming osteophytes. Subchondral cysts and bone thickening/sclerosis develop. - Imaging plays a crucial role in Dx/grading and management
- Clinically: pain on walking/rest, crepitus, swelling d/t synovitis, locking/catching d/t osseocartilaginous fragments and gradual functional loss. Knee OA typically presents as mono and
loigoarthritis . DDx: morning pain/stiffness is >30-min DDx from inflammatory arthritis - Treatment: in mild to moderate cases-conservative care. Severe OA-total knee
arthroplasy
OA: L.O.S.S. Radiologic Presentation
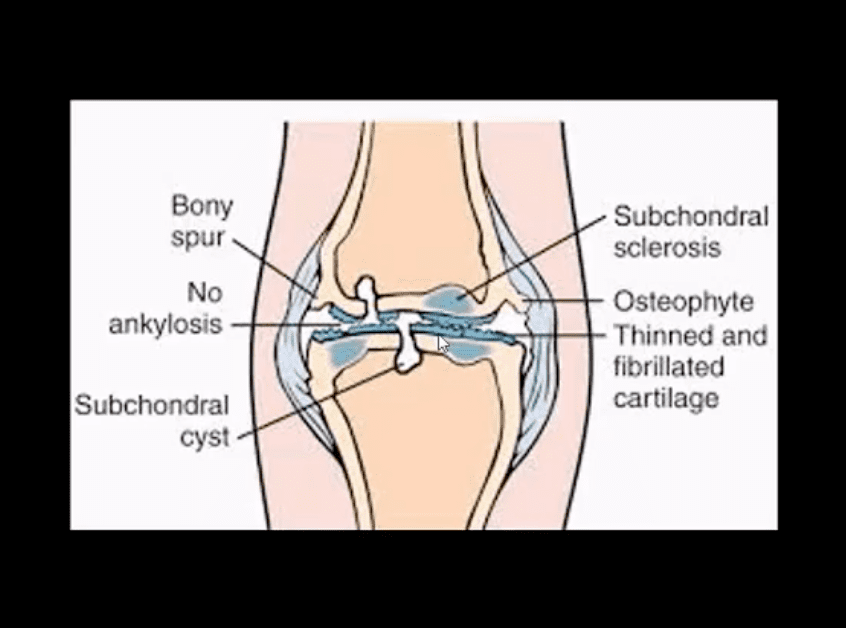
- Typical radiologic-pathologic presentation of OA: L.O.S.S.
- Loss of joint space (non-uniform/asymmetrical)
- Osteophytes
- Subchondral sclerosis
- Subchondral cysts
- Bone deformity: Genu Varum- is the m/c deformity d/t medial knee compartment affected more severely
- In addition: weakening of periarticular soft tissues, instability and other changes
Imaging
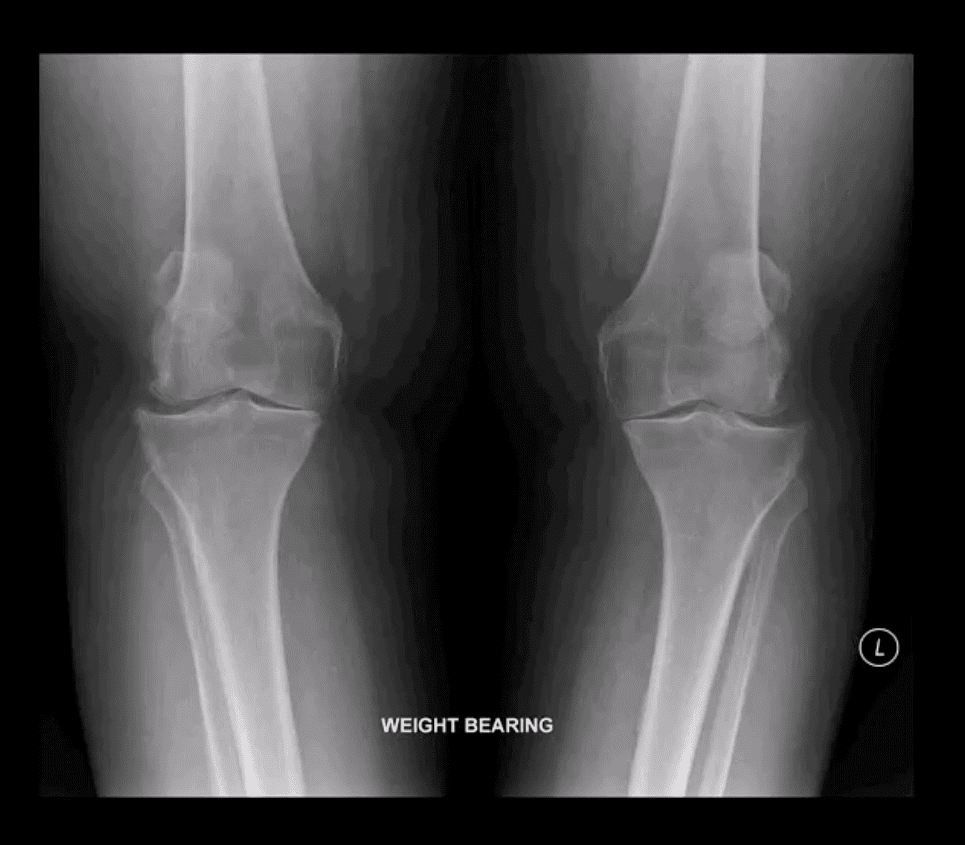
- Radiography is the modality of choice
- Views should include b/l weight bearing
- Evaluation of joint space is crucial. Normal joint space -3-mm
- Grading is based on the degree of joint space narrowing (JSN), osteophytes, bone deformation, etc.
- Grade 1: minimal JSN, suspicious osteophytes
- Grade 2: appreciable osteophytes and JSN on AP weight-bearing view
- Grade 3: multiple osteophytes, definite JSN, subchondral sclerosis
- Grade 4: severe JSN, large osteophytes, marked subchondral sclerosis and definite bony deformity
- Typical report language will state:
- Minor, mild, moderate or severe aka advanced arthrosis
Technique
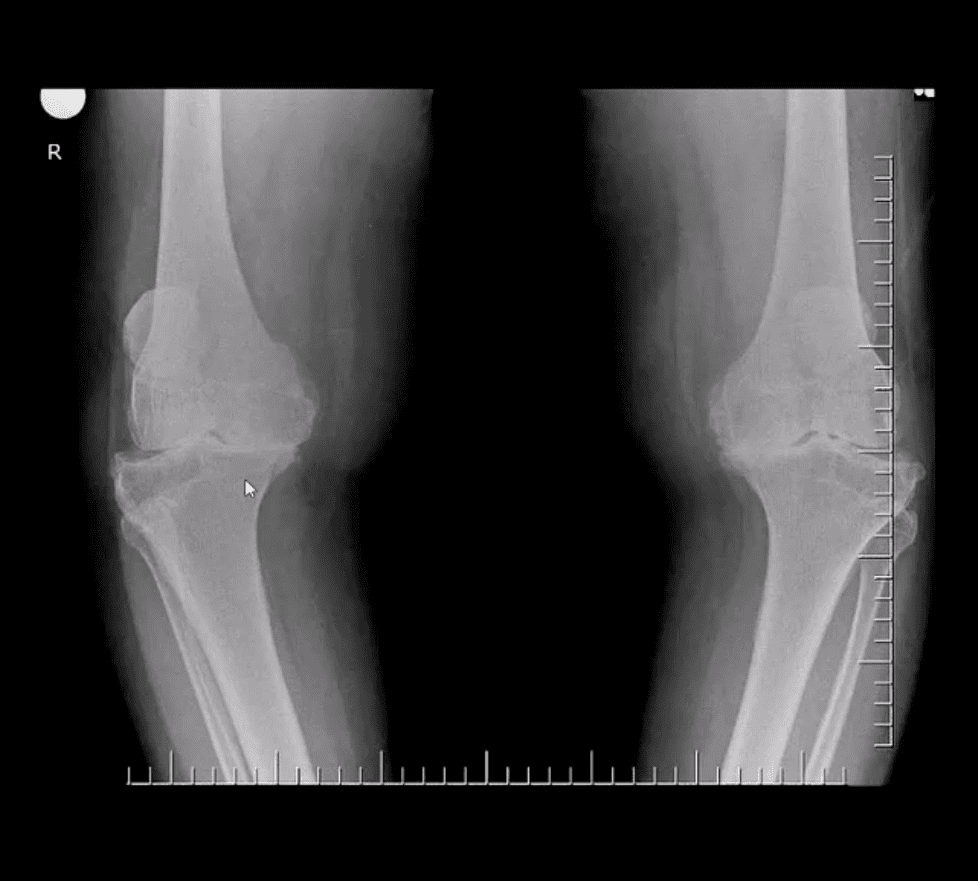
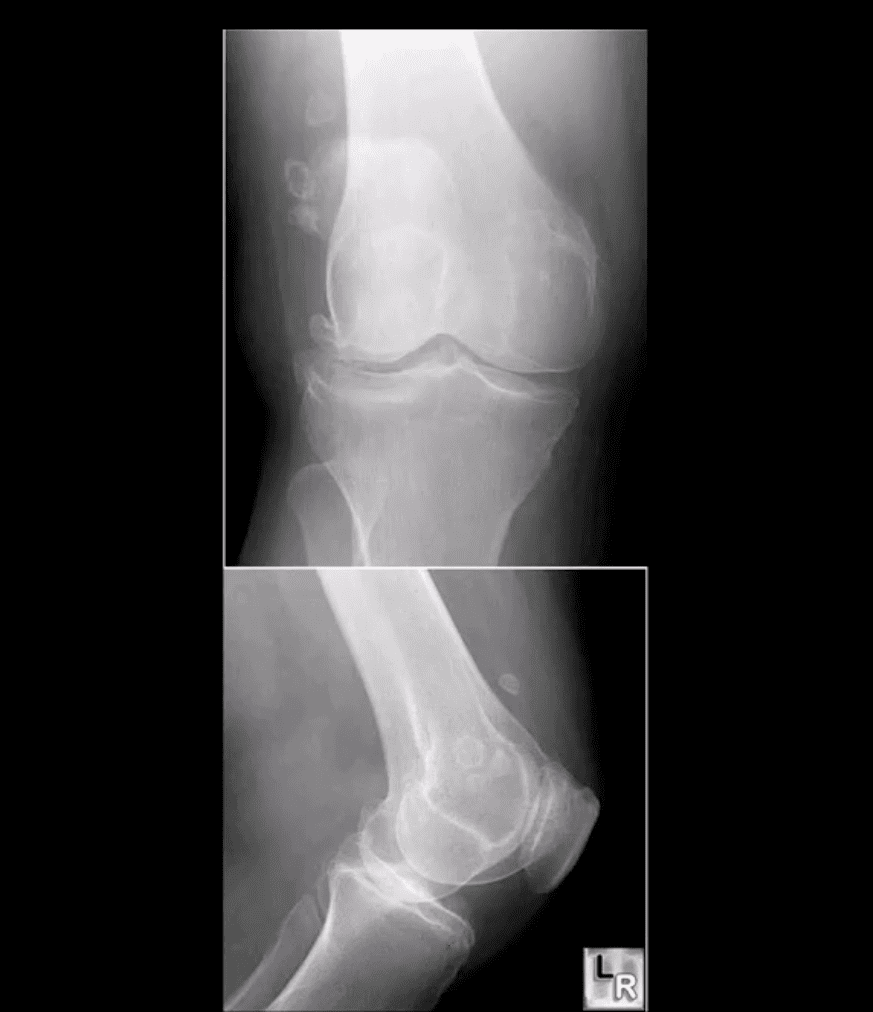
- Radiography: AP weight-bearing knees: note severe JSN of the medial compartment more severely with lateral knee compartment. Osteophytes and marked genu varum deformity and bone deformation
- Typically medial
femoro-tibial compartment is affected early and more severely Patellofemoral compartment is also affected and best visualized on the lateral and Sunrise views- Impressions: severe tri-compartmental knee arthrosis
- Recommendations: referral to the orthopedic surgeon
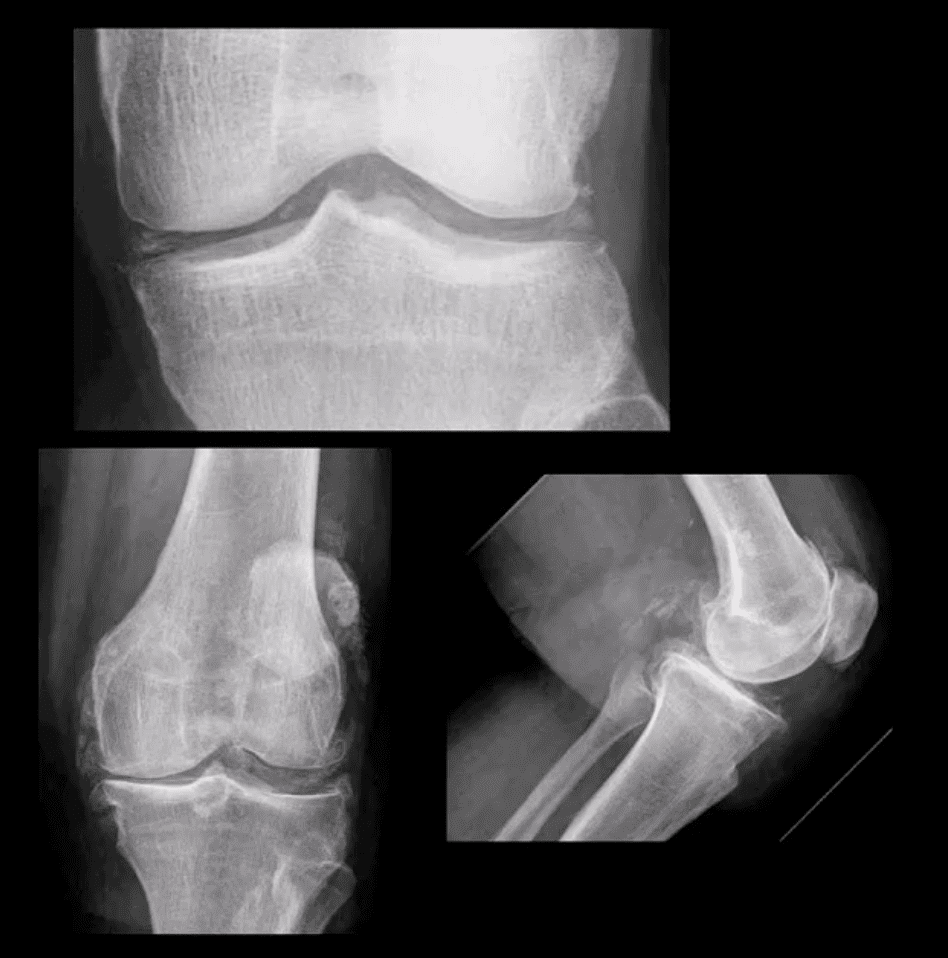
Moderate JSN
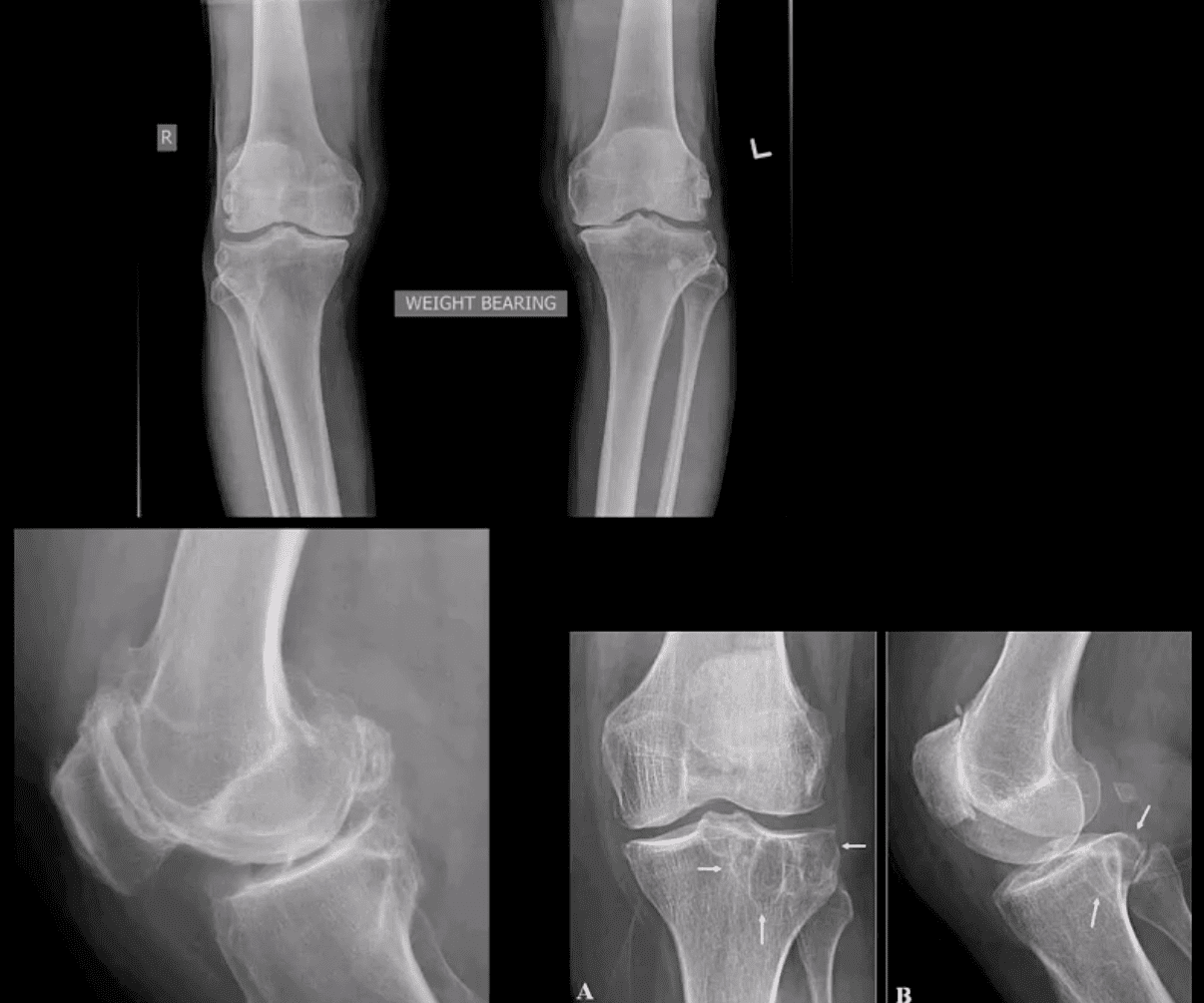
- B/L AP weight bearing view (above top image): Moderate JSN primarily of the medial femorotibial compartment. Osteophytosis, subchondral sclerosis and mild bone deformation (genu varum)
- Additional features: PF OA, intra-articular osteophytes, secondary osteo-cartilagenous loose bodies and subchondral cysts (above arrows)
Secondary Osteochondromatosis
- Intra-articular osteo-cartilagenous loose bodies known as secondary osteochondromatosis
- Typical in DJD especially of the large joints
- It may accelerate further cartilage destruction and progression of OA
- May worsen signs of synovitis
- Intra-articular locking, catching etc.
Management of Severe Knee OA
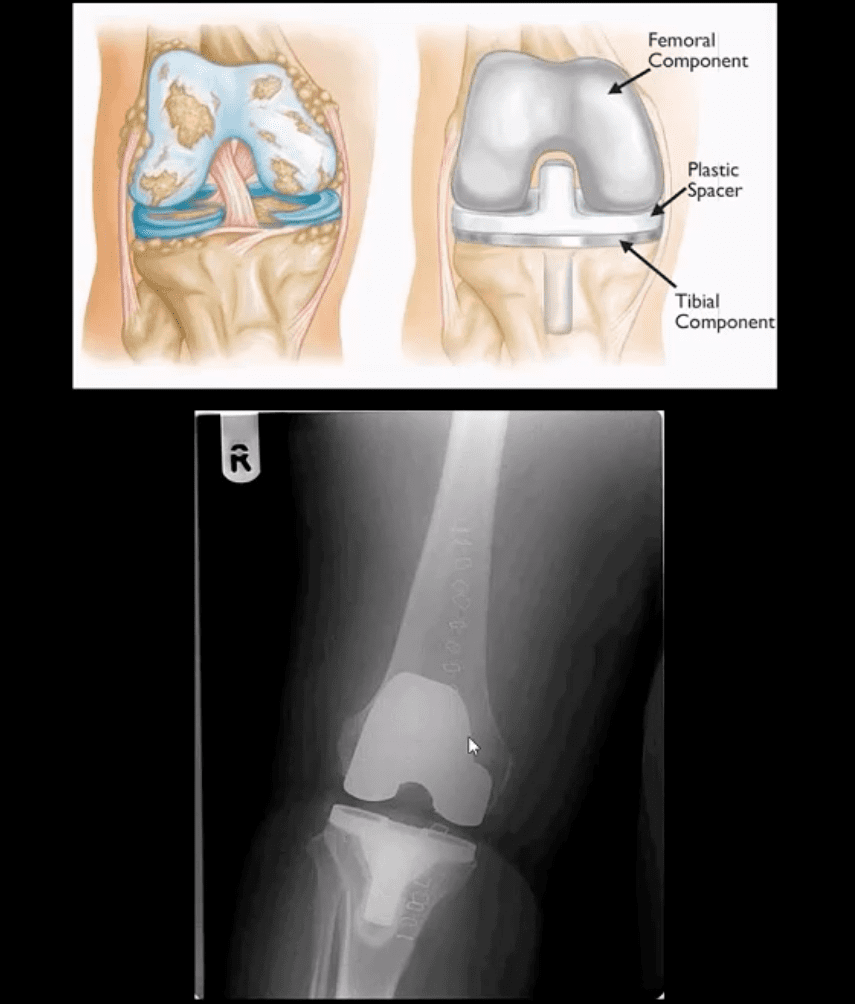
- Conservative care: NSAID, exercise, weight loss etc.
- Operative care should be used if conservative care failed or symptoms progress despite conservative efforts in severe OA cases
- Review article
- https://www.aafp.org/afp/2018/0415/p523.html
Calcium Pyrophosphate Dehydrate Deposition Disease
- CPPD arthropathy common in the knee
- May present as asymptomatic chondrocalcinosis, CPPD arthropathy resembling DJD with predominance of lare subchondral cysts. Often found as isolated PFJ DJD
- Pseudogout with acute attack of knee pain resembling gouty arthritis
- Radiography is the 1st step and often reveals the Dx
- Arthrocenthesis with polarized microscopy may be helpful to DDx between CPPD and Gouty arthritis
Rheumatoid Arthritis
- RA:
autoimmune systemic inflammatory disease that targets soft tissues of joints synovium, tendons/ligaments, bursae and extra-articular sites (e.g. eyes, lungs, cardiovascular system) - RA is the m/c inflammatory arthritis, 3% of women and 1% of men. Age: 30-50 F>M 3:1, but may develop at any age. True RA is uncommon in children and should not be confused with Juvenile Idiopathic Arthritis
- RA most often affects small joints of the hands and feet as symmetrical arthritis (2nd 3rd MCP, 3rd PIPs, wrists & MTPs, sparing DIPs of fingers and toes)
- Radiographically: RA presents with joint effusion leading to hyperemia and marginal erosions and periarticular osteoporosis. In the knee,
lateral compartment is affected more frequently leading to valgus deformity. Uniform aka concentric/symmetrical JSN affects all compartments and remains a key Dx clue Absence of subchondral sclerosis and osteophytes. Popliteal cyst (Baker’s cyst) may represent synovial pannus and inflammatory synovitis extending intopopliteal region that may rapture and extend into posterior leg compartment- N.B. Following initial RA joint destruction, it is not unusual to note superimposed 2nd OA
- Radiography is the 1st step but early joint involvement may be undetectable by x-rays and can be helped by US and/or MRI.
- Lab tests: RF, CRP, anti-cyclic citrullin peptide antibodies (anti-CCP Ab). CBC
- Final Dx is based on Hx, clinical exam, labs and radiology
- Clinical pearls: patients with RA may present with a single knee being affected
- Most patients are likely to have bilateral symmetrical hands/feet RA.
- Cervical spine, particularly C1-2 is affected in 75-90% of cases throughout the course of the disease
- N.B. Sudden exacerbation of joint pain in RA should not underestimate septic arthritis because patients with pre-existing RA are at higher risk of infectious arthritis. Joint aspiration may help with Dx.
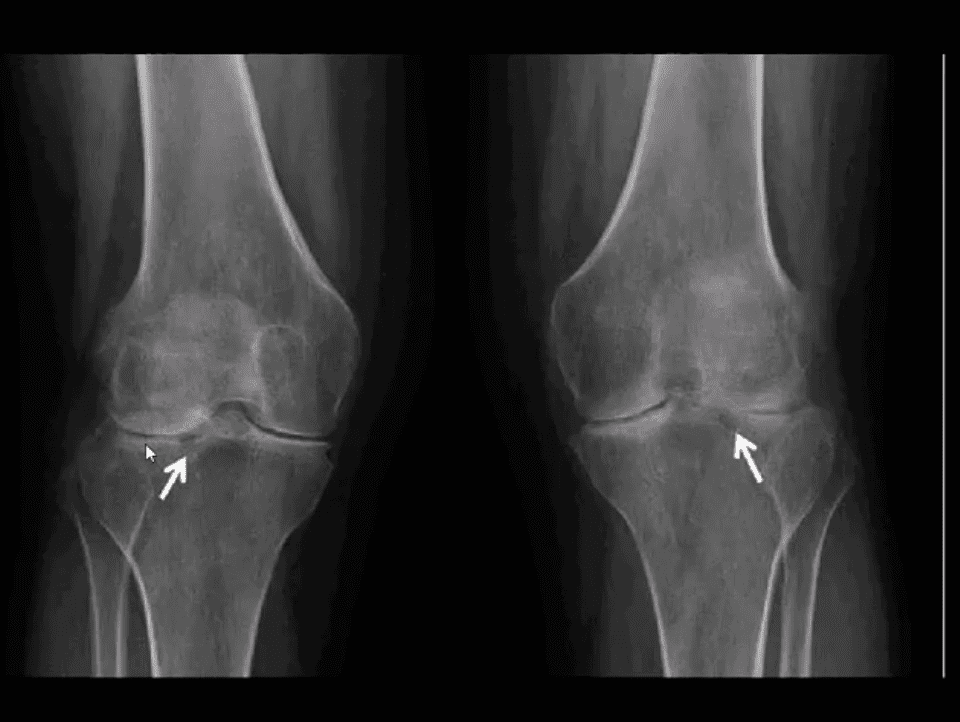
Radiographic DDx

- RA (above left) vs. OA (above right)
- RA: concentric (uniform) joint space loss, lack of osteophytes and juxta-articular osteopenia.
- Clinical Pearls: patients with RA may present radiographically with subchondral sclerosis d/t superimposed DJD. The latter feature should not be interpreted as OA but instead considered as secondary OA
AP Knee Radiograph
- Note marked uniform JSN, juxta-articular osteopenia and subchondral cystic changes
- Clinical Pearls: subcortical cysts in RA will characteristically lack of sclerotic rim noted in OA-associated subcortical cysts.
MRI Sensitivity

- MRI is very sensitive and may aid during early Dx of RA.
- T2 fat-sat or STIR and T1 + C gad contrast fat-suppressed sequences may be included
- MRI Dx of RA: synovial inflammation/effusion, synovial hyperplasia and pannus formation, decreased cartilage thickness, subchondral cysts and bone erosions
- MRI is very sensitive to reveal juxt-articular bone marrow edema, a precursor to erosions
- Intra-articular fibrinoid fragments known as “Rice bodies” are characteristic MR sign of RA
- Note: T2 fat-sat sagittal MRI revealing large inflammatory joint effusion and pannus synovial proliferation (above arrow heads). No evidence of radiographic or MRI bone erosions present. Dx: RA
STIR MR Slices
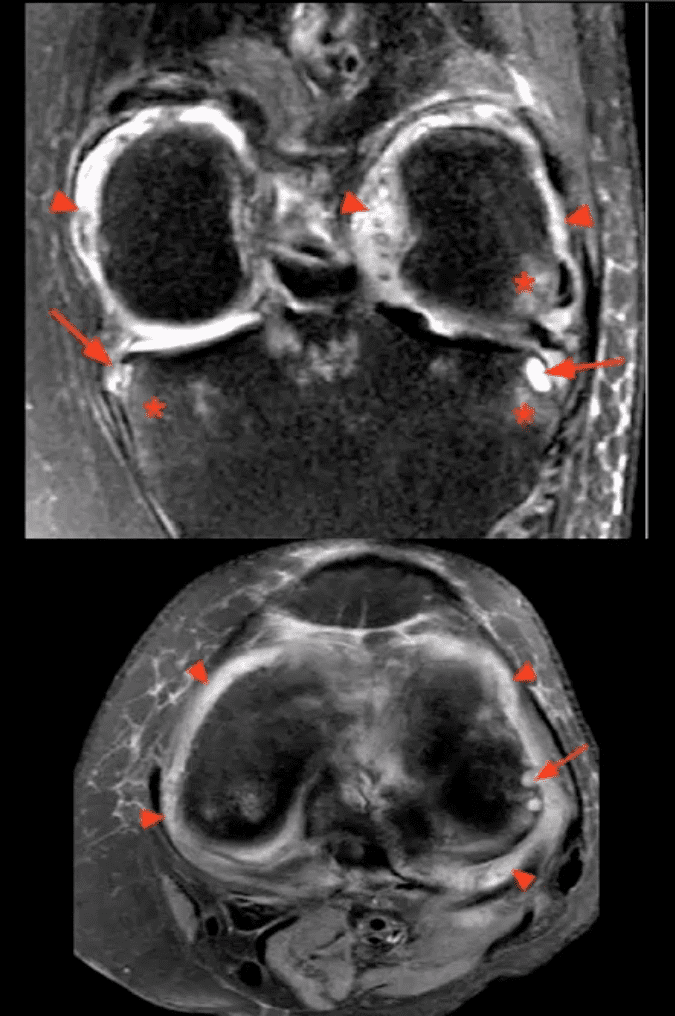
- Note: STIR MR slices in the axial (above bottom image) and coronal planes (above top image) demonstrate extensive synovitis/effusion (above arrowheads) and multiple erosions in the medial and lateral tibial
palteau (above arrows) - Additionally, scattered patchy areas of bone marrow edema are noted (above asterisks) such marrow edema changes are indicative and predictive of future osseous erosions.
- Additional features: note thinning and destruction of joint cartilage
Knee Arthritis
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


