Anyone can get a spinal infection. Individuals can have an infection:
- In vertebral bone tissue
- An intervertebral disc
- The spinal canal – space where the spinal cord runs through
- The spinal cord’s protective lining
These types of infections can happen anywhere along the spine, from the atlas at the base of the neck to the coccyx all the way to the lowest part of the back. Individuals should expect unpredictability if dealing with a spinal infection. During testing, lab results could be misleading or inaccurate. What can happen is white blood cell counts are normal, X-rays might not show any abnormalities, and sensitive diagnostic tests like a CT or MRI scan might not show positivity of infection for a week or more. What to know about spinal infections.

Table of Contents
Spinal Infection Types
They are classified according to the type of tissue they infect. The most common include:
Vertebral Osteomyelitis
This is a common infection type. Bacteria most often cause the cause. It can develop after trauma to the spine, post-surgery, or bacterial infections located in other body parts that travel via the blood to the vertebra. Symptoms include:
- Persistent, chronic back pain that can become severe worsens at night and becomes aggravated by moving.
- The pain radiates/spreads into the arms and legs
- Tingling, numbness, and burning sensations
- Inflammation
- Fever
- Weight loss
- Vomiting
- Post-surgery wound drainage, redness, and swelling near the surgical site
Treatment includes:
- Intravenous antibiotics
- Antibiotics
- Over-the-counter analgesics like nonsteroidal anti-inflammatory meds for pain relief.
- Prescription pain medications
- Back brace
- Surgery is recommended if antibiotic treatment fails, nerve damage develops, a spinal deformity develops, or to remove infected bone and/or soft tissues.
Discitis
This type of infection develops between the intervertebral discs. It is also rare but is more common in children and adolescents, but it can still happen in adults. Discitis can be potentially deadly, despite advanced treatment. The most common causes are bacterial and viral infections.
- The Staphylococcus aureus bacterium, known as staph, is the most common microbe that can cause discitis.
- Other forms of staph that cause discitis include:
- E. coli
- Salmonella
- Strep
- Fungi
- Autoimmune disorders
Symptoms
Individuals with discitis can present with minimal symptoms when the infection initializes, but it does worsen and can cause:
- Abdominal pain and discomfort
- Posture changes
- Mobility issues
- Difficulty performing everyday tasks
- Fever
- Severe back pain that worsens at night or by moving
Treatment options include:
- Antibiotics
- Anti-inflammatory medications
- Supportive devices
- Rest
- Steroids to alleviate inflammation in chronic and severe cases
- Severe cases could require surgery to restructure areas of the affected spine to improve function and mobility
Epidural Abscess
This is an infection that can develop in the spaces between the bones of the spine, the skull, or soft tissues surrounding the brain and spinal cord. This is a medical emergency that needs to be addressed immediately. The infection is often caused by a bacterial or fungal infection in or around the affected area. This is commonly a Staphylococcus aureus bacteria. An abscess can sometimes develop from an infection in another part of the body. This could be a urinary tract infection that spreads out to the spine. Symptoms include:
- Inflammation and swelling
- Mid to low back pain
- Headache
- Fever
- Nausea and/or vomiting
- Neurological weakness, numbness in the arms and legs, bowel or bladder incontinence
- Walking problems
Treatment consists of intravenous antibiotics to combat the infection that caused the abscess. In some cases, if there is difficulty moving around or experiencing numbness, surgery is required to drain the abscess or completely remove it.
Risk Factors
Spine infections can affect anyone. However, some individuals with certain chronic health problems have an increased risk. They include those with:
- Kidney disease
- Liver disease
- Auto-immune diseases
- Immune systems compromised like cancer and HIV
- Individuals that have undergone a spinal surgical procedure are at greater risk post-surgery
Risk factors include:
- Individuals that have had a spinal infection could be more susceptible to developing another.
- Age – older adults
- Malnutrition
- Diabetes mellitus
- Obesity
- Smoking
- Intravenous drug use
- Certain areas of the back are more prone to infection. This includes the cervical/back of the neck and the lumbar/low back.
Surgical risk factors:
- Long surgical procedure
- Massive loss of blood
- Multiple surgeries in the same area
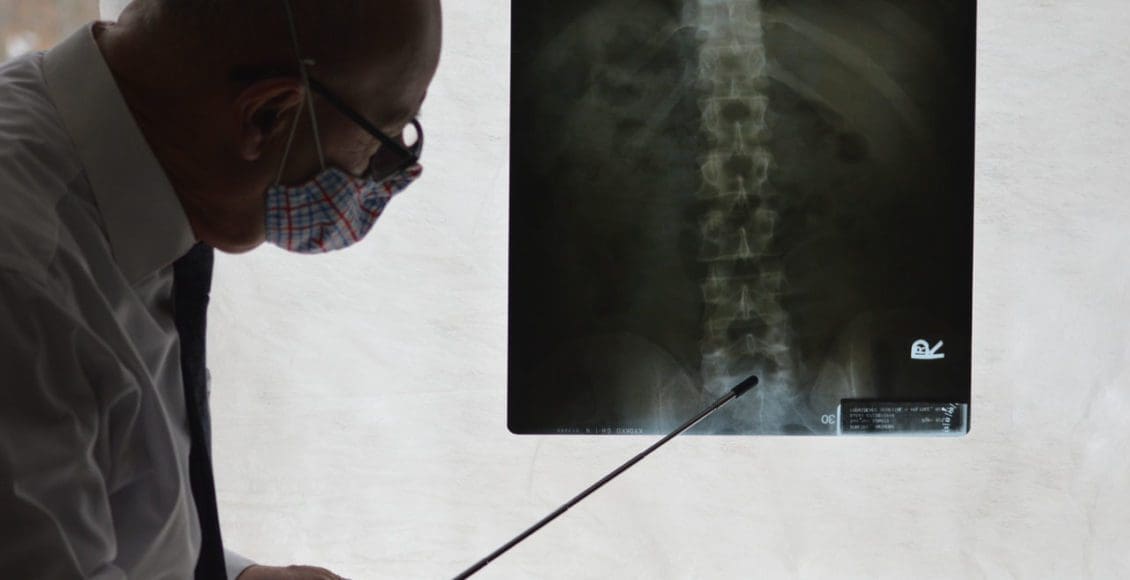
Diagnosis
Early diagnosis can be the difference in treating the infection before damage to the spine develops or before the damage worsens. They are diagnosed through a variety of lab and imaging tests. These include:
- Various lab tests
- Blood work to examine white blood cell counts and markers for inflammation
- X-Rays
- CT scan
- MRI
Outcome
These infections are rare but serious, and early treatment is recommended for optimal outcomes. Early diagnosis in the early stages can be successfully treated with antibiotics, rest, and spinal braces. Doctors, spine specialists, chiropractors, and physical therapists will work with the individual to provide a thorough diagnosis, personalized treatment plan, and long-term outcomes.
Body Composition
Practice Mindfulness
Practicing mindfulness can help identify triggers of negative thoughts and behavior. Mindfulness is unique to each individual. Sitting quietly and meditating for 20 minutes is not for everyone. Instead, try a five-minute guided meditation, writing, or music listening. The best time to meditate is in the morning after waking up. This helps set the day’s objectives, what’s important and what can wait in a clear fashion. Mindfulness practice has been shown to reduce stress and feelings of anxiety.
Journaling is a great way to find out about yourself. It can be done with a pencil/pen and paper on a computer, tablet, or phone. Take a few minutes to write some ideas, feelings, and emotions that can help put things in perspective. Examples could be, writing something that makes you happy/proud, something that you want to improve, and a goal. There is also mindful listening that can help reduce stress by focusing attention. Instead of turning on the news or checking email first thing, listen to a favorite podcast or music. The same applies to over-phone use. During some downtime, instead of scrolling through social media, etc., take a breath and listen to your mind and self.
References
American Association of Neurological Surgeons. Spinal Infections. www.aans.org/Patient%20Information/Conditions%20and%20Treatments/Spinal%20Infections.aspx. Published May 2016. Accessed December 29, 2016.
Stat Pearls. (2021). Diskitis. www.ncbi.nlm.nih.gov/books/NBK541047/
Stat Pearls. (2021). Spinal Epidural Abscess. www.ncbi.nlm.nih.gov/books/NBK441890/
Frontiers in Medicine. (2014). Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. www.frontiersin.org/articles/10.3389/fmed.2014.00007/full
Microorganisms. (2020). Spinal Infections: An Update. www.ncbi.nlm.nih.gov/pmc/articles/PMC7232330/
The Spine Journal. (2021.) “Long-term quality of life outcome after spondylodiscitis treatment.” www.thespinejournalonline.com/article/S1529-9430(21)00783-X/fulltext
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card