All disease starts in the gut, but how? Intestinal permeability is a great contributor to metabolic and chronic conditions, as it allows bacterial translocation. Furthermore, this triggers local and systemic inflammation. However, these two factors, combined with the presence of gut-derived metabolites, like trimethylamine N-oxide (TMAO), have recently been associated with heart failure. Nevertheless, discovering this new contributor of disease creates more opportunity areas for preventing chronic diseases by measuring this marker as a sign of metabolic health and dysbiosis.
Table of Contents
CVD and Heart Failure:
The end-stage of cardiovascular disease is heart failure (HF). It encompasses many pathological mechanisms such as elevated inflammatory response, activation of the neuroendocrine system, abnormal hemodynamics, and cardiac remodeling. HF has an inferior prognosis despite all the therapeutic drugs.
Indeed, the HF pathophysiology is still not understood to its fullest extent, and so its progression. Nonetheless, the impaired cardiac output and systemic circulation reflect on bowel hypoperfusion, causing mucosal ischemia. Consequently, mucosal ischemia may increase gut permeability, facilitating bacterial and microbial metabolites into the blood circulation. Finally, the combination of these factors results in chronic low-grade inflammation.
Intestinal permeability induced by systemic congestion:
- C-reactive protein and interleukin-6 levels rise when bacterial translocation is present.
- Intestinal permeability allows lipopolysaccharide (LPS) to enter the systemic circulation, upregulating the immunologic response.
- The LPS presence also triggers the production and release of proinflammatory cytokines. In turn, these cytokines act directly on cardiomyocytes and cardiac fibroblasts.
- Elevated serum levels of proinflammatory cytokines (IL-1, IL-6, and TNF-a) play a fundamental role in cardiomyocyte apoptosis, hypertrophy, and the fibrosis process.
Trimethylamine N-oxide: TMAO
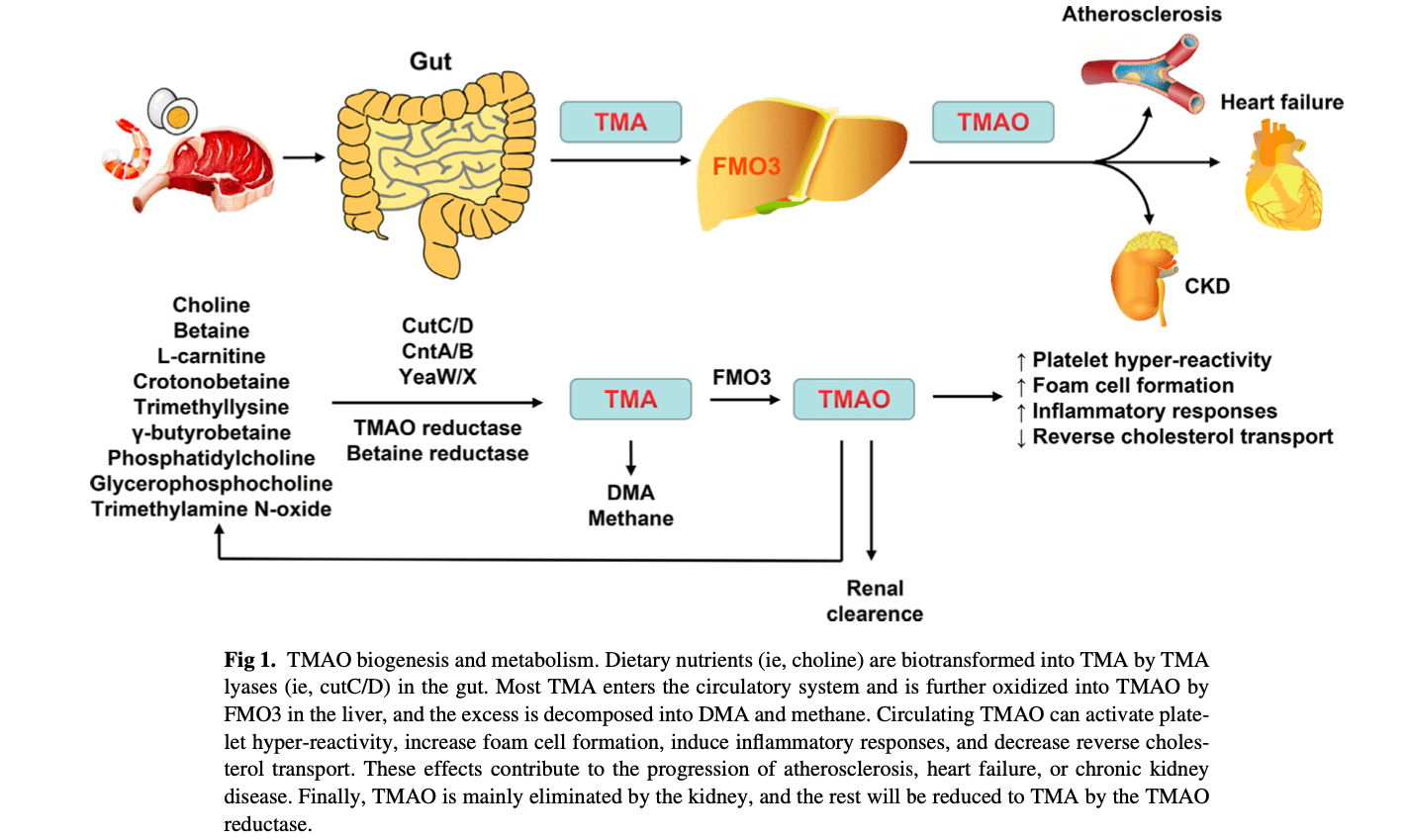
Trimethylamine N-oxide is a molecular metabolite produced by the gut’s microbiota, associated mainly with an increased risk of cardiovascular events. However, TMAO is a metabolite from trimethylamine (TMA) conversion via flavin-containing mono-oxygenase (FMO). Nowadays, TMAO is a potent mediator closely associated with the prevalence of atherosclerosis, hypertension, myocardial infarction, and diabetes. Consequently, these same characteristics allow TMAO to be a powerful prognostic marker delineating cardiac conditions’ progression leading to HF. The elevated levels of TMAO are present when harmful gut microbiota proliferates under an unbalanced state.
TMA-O metabolism:
In the gut, microbiota converts multiple dietary components into TMA. Indeed, fish, meat, eggs, dairy contain nutrients such as L-carnitine, choline, betaine, phosphatidylcholines, and TMAO, which are TMA precursors.
TMA gets synthesized when these precursors interact with specific intestinal microbial enzymes.
Microbial enzyme systems:
As mentioned before, TMA enters the circulatory system and finally turns into TMAO through the hepatic enzyme FMO3.
FMO3: Hepatic enzyme, with a rate-limiting capacity to convert TMA into TMAO.
However, when FMO3 is insufficient and fails to convert TMA excess into TMAO, it promotes a disease called trimethylaminuria. This condition is present with a strong “fishy odor” caused by TMA excretion in the urine, sweat, and respiration. On the other hand, excessive TMAO can accumulate in the kidneys, heart, and other tissues, leading to increased cell foam formation, platelet aggregation, and reverse cholesterol transport.
Studies consistently show a close relationship between specific microbiota strains in patients with HF and those with increased circulating TMAO levels. Furthermore, the patient’s genotype is another contributing factor since it directly affects the gut’s microbiome composition, the immunomodulatory pathways, and metabolic phenotypes.
TMAO and myocardial hypertrophy and fibrosis:
Elevated levels of TMAO are typical in mouse models with transverse aortic constriction, a pressure-overloaded HF model. In contrast with the lower TMAO levels found in the sham-operated groups.
Besides this, TMAO promotes fibrosis and myocardial hypertrophy via Smad3 signaling pathways, in vivo, and in vitro. To prove this mechanism, 3,3-dimethyl-1-butanol (DMB) inhibited the TMA synthesis and prevented myocardial hypertrophy and fibrosis. Also, 3,3-dimethyl-1-butanol (DMB) downregulates transforming growth factor-b1 (TGF-b1)/Smad3 and p65 nuclear factor-kB (NF-kB) signaling pathways, involved in ventricular remodelling.
TMAO and the inflammatory response:
As aforementioned, choline is a precursor of TMAO. Therefore in mice models fed with choline, the TMAO production upregulates inflammatory pathways, such as NF-kB. The translocation of NF-kB results in the inflammation of vascular smooth muscle cells.
Also, TMAO elevated levels can result in sirtuin inhibition (SIRT3) and lower superoxide dismutase 2 (SOD2)activity. Consequently, this results in the accumulation of mitochondrial reactive oxygen species. Furthermore, this cascade triggers the NLRP3 inflammasome activation, promoting the synthesis and release of proinflammatory cytokines IL-1b and IL-18. Finally, the elevated levels of these cytokines result in epithelial cell inflammation.
TMAO reduces self-healing capacity by upregulating vascular cell adhesion molecule (VCAM)-1, leading to endothelial dysfunction.
Overall, TMAO presence is an alarming metabolic marker which we can in our favor. The new AHA guidelines recommend measuring TMAO levels to prevent heart failure. TMAO presence can be indicative of gut microbial dysbiosis and mucosal ischemia. Therefore, treating the gut should always be the first step in preventing and reversing metabolic conditions.
After reading this article, you might feel the urge to quit animal protein sources but relax; there are other ways to reduce TMAO production. Remember that the gut microbiome and hepatic enzymes play an essential role in TMA and TMAO production. Therefore, promoting healthy gut colonization and an antioxidant diet may lower TMAO production and contribute to our heart health. – Ana Paola Rodríguez Arciniega, MS
References:
Zhang, Yixin et al. “TMAO: how gut microbiota contributes to heart failure.” Translational research: the journal of laboratory and clinical medicine vol. 228 (2021): 109-125. doi:10.1016/j.trsl.2020.08.007
Additional Online Links & Resources (Available 24/7)
Online Appointments or Consultations: https://bit.ly/Book-Online-Appointment
Online Physical Injury / Accident Intake Form: https://bit.ly/Fill-Out-Your-Online-History
Online Functional Medicine Assessment: https://bit.ly/functionmed
Disclaimer
The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional, licensed physician, and not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the musculoskeletal system’s injuries or disorders. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and issues that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us 915-850-0900. Read More.
Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, CTG*
email: coach@elpasofunctionalmedicine.com
phone: 915-850-0900
Licensed in Texas & New Mexico
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


