Fibromyalgia is a condition that causes pain throughout the whole body. It causes sleep problems, fatigue, and mental/emotional distress. It affects around four million adults in the United States. Individuals with Fibromyalgia tend to be more sensitive to pain. This is referred to as abnormal/altered pain perception processing. Research currently leans towards a hyperactive nervous system as one of the most plausible causes.
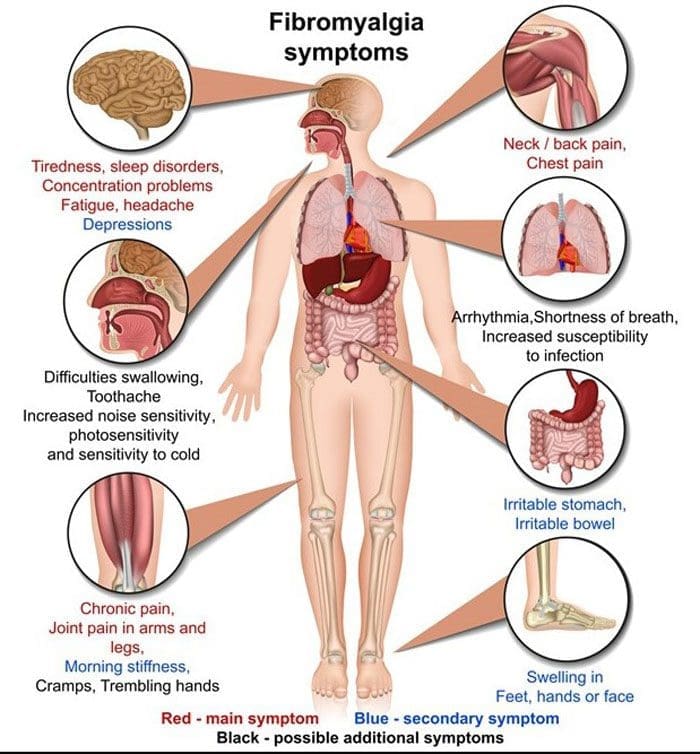
Table of Contents
Symptoms and Related Conditions
Individuals with fibromyalgia/fibromyalgia syndrome/FMS may have:
- Fatigue
- Sleep issues
- Headaches
- Concentration, Memory issues, or Fibro Fog
- Stiffness
- Tender points
- Pain
- Numbness and tingling in hands, arms, legs, and feet
- Anxiety
- Depression
- Irritable bowel syndrome
- Urinating issues
- Abnormal menstrual cramps
Altered Central Pain Processing
Central sensitization means that the central nervous system, composed of the brain and spinal cord, processes pain differently and more sensitively. For example, individuals with Fibromyalgia could interpret physiological stimuli, like heat, coldness, and pressure, as pain sensations. Mechanisms that cause altered pain processing include:
- Pain signal dysfunction
- Modified opioid receptors
- Substance P increase
- Increased activity in the brain where pain signals are interpreted.
Pain Signal Dysfunction
When a painful stimulus is felt, the brain signals the release of endorphins, the body’s natural painkillers that block the transmission of pain signals. Individuals with Fibromyalgia could have a pain-blocking system that is altered and/or not functioning correctly. There is also the inability to block repetitive stimuli. This means that the individual keeps feeling and experiencing the stimuli even as they try to block them out, suggesting a failure in the brain to filter out irrelevant sensory information.
Modified Opioid Receptors
Research has found that individuals with fibromyalgia have a reduced number of opioid receptors in the brain. Opioid receptors are where endorphins bind so the body can use them when necessary. With fewer available receptors, the brain is less sensitive to endorphins, as well as opioid pain medication like:
- Hydrocodone
- Acetaminophen
- Oxycodone
- Acetaminophen
Substance P Increase
Individuals with fibromyalgia have been found to have elevated levels of substance P in their cerebrospinal fluid. This chemical is released when nerve cells detect a painful stimulus. Substance P is involved with the body’s pain threshold, or the point when a sensation turns into pain. High levels of substance P could explain why the pain threshold is low in individuals with fibromyalgia.
Increased Activity in the Brain
Brain imaging tests, like magnetic resonance imaging or MRI, have shown that fibromyalgia is associated with greater than regular activity in areas of the brain that interpret pain signals. This can suggest that pain signals are overwhelming those areas or that the pain signals are being processed dysfunctionally.
Triggers
Certain factors can trigger a flare-up. These include:
- Diet
- Hormones
- Physical stress
- Too much exercise
- Not enough exercise
- Psychological stress
- Stressful events
- Sleep Patterns changed
- Treatment changes
- Temperature changes
- Weather changes
- Surgery
Chiropractic
Chiropractic focuses on whole-body wellness. 90% of the central nervous system goes through the spinal cord. A misaligned vertebral bone can create interference and irritation on the nerves. Fibromyalgia is a condition related to the hyperactivity of the nerves; therefore, any vertebral subluxations will complicate and aggravate fibromyalgia symptoms. Realigning the misaligned vertebrae releases stress off the spinal cord and spinal nerve root. That is why individuals with fibromyalgia are recommended to add a chiropractor to their healthcare team.
Body Composition
Dietary Supplement Quality Guide
References
Clauw, Daniel J et al. “The science of fibromyalgia.” Mayo Clinic proceedings vol. 86,9 (2011): 907-11. doi:10.4065/mcp.2011.0206
Cohen H. Controversies and challenges in fibromyalgia: a review and a proposal. Ther Adv Musculoskelet Dis. 2017 May;9(5):115-27.
Garland, Eric L. “Pain processing in the human nervous system: a selective review of nociceptive and biobehavioral pathways.” Primary care vol. 39,3 (2012): 561-71. doi:10.1016/j.pop.2012.06.013
Goldenberg DL. (2017). Pathogenesis of fibromyalgia. Schur PH, (Ed). UpToDate. Waltham, MA: UpToDate Inc.
Kamping S, Bomba IC, Kanske P, Diesch E, Flor H. Deficient modulation of pain by a positive emotional context in fibromyalgia patients. Pain. 2013 Sep;154(9):1846-55.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


