Table of Contents
Opportunities For Clinical Intervention
Even though the effects of overweight and obesity on diabetes, cardiovascular disease, all-cause mortality, and other health outcomes are widely known, there is less awareness that overweight, obesity, and weight gain are associated with an increased risk of certain cancers. A recent review of more than 1000 studies concluded that sufficient evidence existed to link weight gain, overweight, and obesity with 13 cancers, including adenocarcinoma of the esophagus; cancers of the gastric cardia, colon and rectum, liver, gallbladder, pancreas, corpus uteri, ovary, kidney, and thyroid; postmenopausal female breast cancer; meningioma; and multiple myeloma.1 An 18-year follow-up of almost 93?000 women in the Nurses’ Health Study revealed a dose-response association of weight gain and obesity with several cancers.2
Obesity Increase
 The prevalence of obesity in the United States has been increasing for almost 50 years. Currently, more than two-thirds of adults and almost one-third of children and adolescents are overweight or obese. Youths who are obese are more likely to be obese as adults, compounding their risk for health consequences such as cardiovascular disease, diabetes, and cancer. Trends in many of the health consequences of overweight and obesity (such as type 2 diabetes and coronary heart disease) also are increasing, coinciding with prior trends in rates of obesity. Furthermore, the sequelae of these diseases are related to the severity of obesity in a dose-response fashion.2 It is therefore not surprising that obesity accounts for a significant portion of health care costs.
The prevalence of obesity in the United States has been increasing for almost 50 years. Currently, more than two-thirds of adults and almost one-third of children and adolescents are overweight or obese. Youths who are obese are more likely to be obese as adults, compounding their risk for health consequences such as cardiovascular disease, diabetes, and cancer. Trends in many of the health consequences of overweight and obesity (such as type 2 diabetes and coronary heart disease) also are increasing, coinciding with prior trends in rates of obesity. Furthermore, the sequelae of these diseases are related to the severity of obesity in a dose-response fashion.2 It is therefore not surprising that obesity accounts for a significant portion of health care costs.
Cancers
A report released on October 3, 2017, by the US Centers for Disease Control and Prevention assessed the incidence of the 13 cancers associated with overweight and obesity in 2014 and the trends in these cancers over the 10-year period from 2005 to 2014.3 In 2014, more than 630?000 people were diagnosed as having a cancer associated with overweight and obesity, comprising more than 55% of all cancers diagnosed among women and 24% of cancers among men. Most notable was the finding that cancers related to overweight and obesity were increasingly diagnosed among younger people.
 From 2005 to 2014, there was a 1.4% annual increase in cancers related to overweight and obesity among individuals aged 20 to 49 years and a 0.4% increase in these cancers among individuals aged 50 to 64 years. For example, if cancer rates had stayed the same in 2014 as they were in 2005, there would have been 43?000 fewer cases of colorectal cancer but 33?000 more cases of other cancers related to overweight and obesity. Nearly half of all cancers in people younger than 65 years were associated with overweight and obesity. Overweight and obesity among younger people may exact a toll on individuals’ health earlier in their lifetimes.2 Given the time lag between exposure to cancer risk factors and cancer diagnosis, the high prevalence of overweight and obesity among adults, children, and adolescents may forecast additional increases in the incidence of cancers related to overweight and obesity.
From 2005 to 2014, there was a 1.4% annual increase in cancers related to overweight and obesity among individuals aged 20 to 49 years and a 0.4% increase in these cancers among individuals aged 50 to 64 years. For example, if cancer rates had stayed the same in 2014 as they were in 2005, there would have been 43?000 fewer cases of colorectal cancer but 33?000 more cases of other cancers related to overweight and obesity. Nearly half of all cancers in people younger than 65 years were associated with overweight and obesity. Overweight and obesity among younger people may exact a toll on individuals’ health earlier in their lifetimes.2 Given the time lag between exposure to cancer risk factors and cancer diagnosis, the high prevalence of overweight and obesity among adults, children, and adolescents may forecast additional increases in the incidence of cancers related to overweight and obesity.
Clinical Intervention

Since the release of the landmark 1964 surgeon general’s report on the health consequences of smoking, clinicians have counseled their patients to avoid tobacco and on methods to quit and provided referrals to effective programs to reduce their risk of chronic diseases including cancer. These efforts, coupled with comprehensive public health and policy approaches to reduce tobacco use, have been effective—cigarette smoking is at an all-time low. Similar efforts are warranted to prevent excessive weight gain and treat children, adolescents, and adults who are overweight or obese. Clinician referral to intense, multicomponent behavioral intervention programs to help patients with obesity lose weight can be an important starting point in improving a patient’s health and preventing diseases associatedwith obesity. The benefits of maintaining a healthy weight throughout life include improvements in a wide variety of health outcomes, including cancer. There is emerging but very preliminary data that some of these cancer benefits may be achieved following weight loss among people with overweight or obesity.4
The US Preventive Services Task Force (USPSTF)
 The US Preventive Services Task Force (USPSTF) recommends screening for obesity and intensive behavioral interventions delivered over 12 to 16 visits for adults and 26 or more visits for children and adolescents with obesity.5,6 Measuring patients’ weight, height, and body mass index (BMI), consistent with USPSTF recommendations, and counseling patients about maintaining a healthy weight can establish a foundation for preventive care in clinical care settings. Scientific data continue to emerge about the negative health effects of weight gain, including an increased risk of cancer.1 Tracking patients’ weight over time can identify those who could benefit from counseling and referral early and help them avoid additional weight gain. Yet less than half of primary care physicians regularly assess the BMI of their adult, child, and adolescent patients. Encouraging discussions about weight management in multiple health care settings, including physicians’ offices, clinics, emergency departments, and hospitals, can provide multiple opportunities for patients and reinforce messages across contexts and care environments.
The US Preventive Services Task Force (USPSTF) recommends screening for obesity and intensive behavioral interventions delivered over 12 to 16 visits for adults and 26 or more visits for children and adolescents with obesity.5,6 Measuring patients’ weight, height, and body mass index (BMI), consistent with USPSTF recommendations, and counseling patients about maintaining a healthy weight can establish a foundation for preventive care in clinical care settings. Scientific data continue to emerge about the negative health effects of weight gain, including an increased risk of cancer.1 Tracking patients’ weight over time can identify those who could benefit from counseling and referral early and help them avoid additional weight gain. Yet less than half of primary care physicians regularly assess the BMI of their adult, child, and adolescent patients. Encouraging discussions about weight management in multiple health care settings, including physicians’ offices, clinics, emergency departments, and hospitals, can provide multiple opportunities for patients and reinforce messages across contexts and care environments.
Weight Loss Programs
 Implementation of clinical interventions, including screening, counseling, and referral, has major challenges. Since 2011, Medicare has covered behavioral counseling sessions for weight loss in primary care settings. However, the benefit has not been widely utilized.7 Whether the lack of utilization is a consequence of lack of clinician or patient knowledge or for other reasons remains uncertain. Few medical schools and residency programs provide adequate training in prevention and management of obesity or in understanding how to make referrals to such services. Obesity is a highly stigmatized condition; many clinicians find it difficult to initiate a conversation about obesity with patients, and some may inadvertently use alienating language when they do. Studies indicate that patients with obesity prefer the use of terms such as unhealthy weight or increased BMI rather than overweight or obesity and improved nutrition and physical activity rather than diet and exercise.8 However, it is unknown if switching to these terms will lead to more effective behavioral counseling. Effective clinical decision support tools to measure BMI and guide physicians through referral and counseling interventions can provide clinicians needed support within the patient-clinician encounter. Inclusion of recently developed competencies for prevention and management of obesity into the curricula of health care professionals may improve their ability to deliver effective care. Because few primary care clinicians are trained in behavior change strategies like cognitive behavioral therapy or motivational interviewing, other trained health care professionals, such as nurses, pharmacists, psychologists, and dietitians could assist by providing counseling and appropriate referrals and help people manage their own health.
Implementation of clinical interventions, including screening, counseling, and referral, has major challenges. Since 2011, Medicare has covered behavioral counseling sessions for weight loss in primary care settings. However, the benefit has not been widely utilized.7 Whether the lack of utilization is a consequence of lack of clinician or patient knowledge or for other reasons remains uncertain. Few medical schools and residency programs provide adequate training in prevention and management of obesity or in understanding how to make referrals to such services. Obesity is a highly stigmatized condition; many clinicians find it difficult to initiate a conversation about obesity with patients, and some may inadvertently use alienating language when they do. Studies indicate that patients with obesity prefer the use of terms such as unhealthy weight or increased BMI rather than overweight or obesity and improved nutrition and physical activity rather than diet and exercise.8 However, it is unknown if switching to these terms will lead to more effective behavioral counseling. Effective clinical decision support tools to measure BMI and guide physicians through referral and counseling interventions can provide clinicians needed support within the patient-clinician encounter. Inclusion of recently developed competencies for prevention and management of obesity into the curricula of health care professionals may improve their ability to deliver effective care. Because few primary care clinicians are trained in behavior change strategies like cognitive behavioral therapy or motivational interviewing, other trained health care professionals, such as nurses, pharmacists, psychologists, and dietitians could assist by providing counseling and appropriate referrals and help people manage their own health.
 Achieving sustainable weight loss requires comprehensive strategies that support patients’ efforts to make significant lifestyle changes. The availability of clinical and community programs and services to which to refer patients is critically important. Although such programs are available in some communities, there are gaps in availability. Furthermore, even when these programs are available, enhancing linkages between clinical and community care could improve patients’ access. Linking community obesity prevention, weight management, and physical activity programs with clinical services can connect people to valuable prevention and intervention resources in the communities where they live, work, and play. Such linkages can give individuals the encouragement they need for the lifestyle changes that maintain or improve their health.
Achieving sustainable weight loss requires comprehensive strategies that support patients’ efforts to make significant lifestyle changes. The availability of clinical and community programs and services to which to refer patients is critically important. Although such programs are available in some communities, there are gaps in availability. Furthermore, even when these programs are available, enhancing linkages between clinical and community care could improve patients’ access. Linking community obesity prevention, weight management, and physical activity programs with clinical services can connect people to valuable prevention and intervention resources in the communities where they live, work, and play. Such linkages can give individuals the encouragement they need for the lifestyle changes that maintain or improve their health.
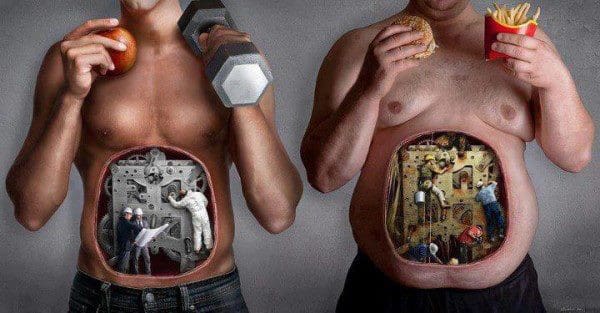 The high prevalence of overweight and obesity in the United States will continue to contribute to increases in health consequences related to obesity, including cancer. Nonetheless, cancer is not inevitable; it is possible that many cancers related to overweight and obesity could be prevented, and physicians have an important responsibility in educating patients and supporting patients’ efforts to lead healthy lifestyles. It is important for all health care professionals to emphasize that along with quitting or avoiding tobacco, achieving and maintaining a healthy weight are also important for reducing the risk of cancer.
The high prevalence of overweight and obesity in the United States will continue to contribute to increases in health consequences related to obesity, including cancer. Nonetheless, cancer is not inevitable; it is possible that many cancers related to overweight and obesity could be prevented, and physicians have an important responsibility in educating patients and supporting patients’ efforts to lead healthy lifestyles. It is important for all health care professionals to emphasize that along with quitting or avoiding tobacco, achieving and maintaining a healthy weight are also important for reducing the risk of cancer.
Targeting Obesity
Greta M. Massetti, PhD1; William H. Dietz, MD, PhD2; Lisa C. Richardson, MD, MPH1
Author Affiliations
Corresponding Author: Greta M. Massetti, PhD, Centers for Disease Control and Prevention, 4770 Buford Hwy NE, Atlanta, GA 30341 (gmassetti@cdc.gov).
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflict of Interest. Dr Dietz reports receipt of scientific advisory board fees from Weight Watchers and consulting fees from RTI. No other disclosures were reported.
Disclaimer: The findings and conclusions in this report are those of the authors and not necessarily the official position of the Centers for Disease Control and Prevention.
References
1. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K; International Agency for Research on Cancer Handbook Working Group. Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794-798. PubMed Article
2. Zheng Y, Manson JE, Yuan C, et al. Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA. 2017;318(3):255-269. PubMed Article
3. Steele CB, Thomas CC, Henley SJ, et al. Vital Signs: Trends in Incidence of Cancers Related to Overweight and Obesity—United States, 2005-2014. October 3, 2017. https://www.cdc.gov/mmwr/volumes/66/wr/mm6639e1.htm?s_cid=mm6639e1_w.
4. Byers T, Sedjo RL. Does intentional weight loss reduce cancer risk? Diabetes Obes Metab. 2011;13(12):1063-1072. PubMed Article
5. Grossman DC, Bibbins-Domingo K, Curry SJ, et al; US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2017;317(23):2417-2426. PubMed Article
6. US Preventive Services Task Force. Final Recommendation Statement: Obesity in Adults: Screening and Management. December 2016. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/obesity-in-adults-screening-and-management. Accessed September 21, 2017.
7. Batsis JA, Bynum JPW. Uptake of the centers for Medicare and Medicaid obesity benefit: 2012-2013. Obesity (Silver Spring). 2016;24(9):1983-1988. PubMed Article
8. Puhl R, Peterson JL, Luedicke J. Motivating or stigmatizing? public perceptions of weight-related language used by health providers. Int J Obes (Lond). 2013;37(4):612-619. PubMed Article
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card