Table of Contents
Ischemic Osteonecrosis
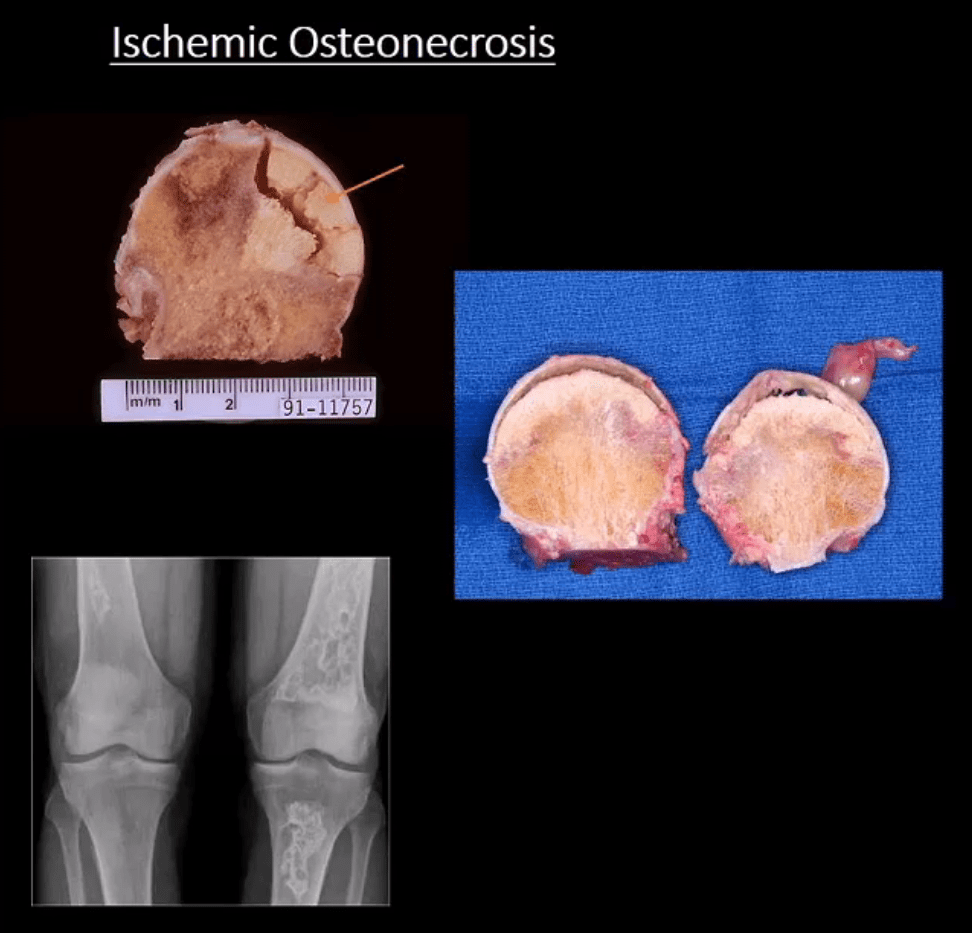
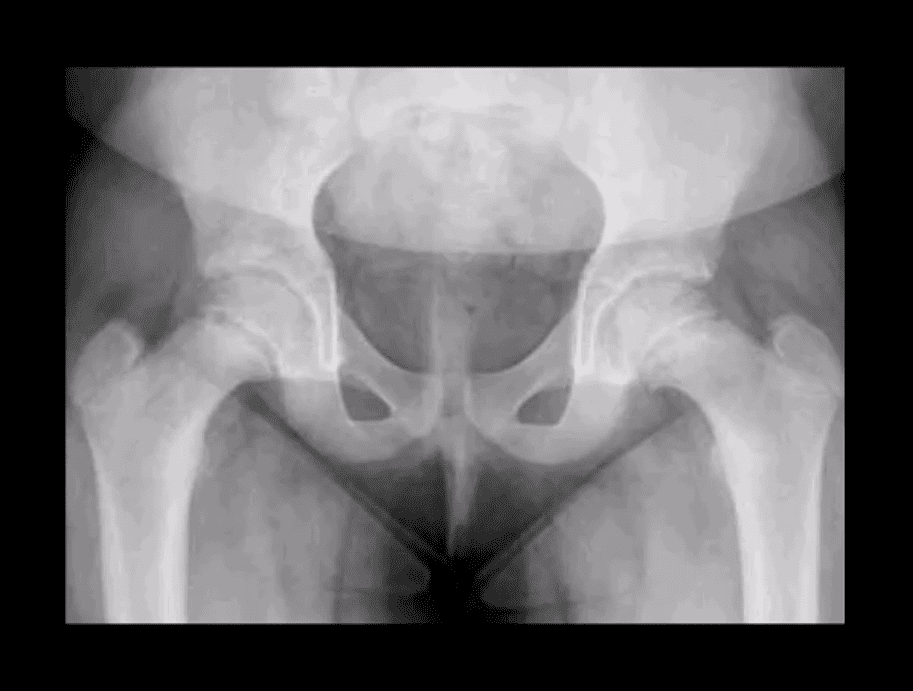
- Ischemic Osteonecrosis (More accurate term) aka avascular necrosis AVN: this term describes subarticular (subchondral) bone death
- Intramedullary bone infarct: describes osteonecrosis within the medullary cavity of the bone (above x-ray image)
- Causes: m/c: trauma, systemic corticosteroids, diabetes, vasculitis in SLE. The list is long. Other important causes: Sickle cell disease, Gaucher disease, alcohol, caisson disease, SCFE, LCP, etc.
- Pathology: ischemia and bone infarct with resultant devitalized center surrounded by ischemia and edema with normal bone on the outer periphery (MRI double line sign)
- Sub-articular necrotic bone eventually collapses and fragments leading to progressive bone and cartilage destruction and rapidly progressing DJD
- Early Dx often missed but crucial to prevent svere DJD
M/C Sites

- Hips, shoulders, talus, scaphoid bone. Many peripheral idiopathic AVN sites are known by their eponyms (e.g. Kienbock aka AVN of the lunate bone, Preisier aka scaphoid AVN)
- Radiography is insensitive to early AVN and may only present as subtle osteopenia
- Some of the early appreciable rad features are increased patchy bone sclerosis followed by sub-articular bone collapse or “crescent sign” signifying stage-3 on Ficat
calssification (above) - Earliest detection and early intervention can be
acheived by MRI (most sensitive modality) - If MRI contraindicated or unavailable, 2nd most sensitive modality is radionuclide bone scan (
scinthigraphy ) - X-ray and CT scanning are of equal value
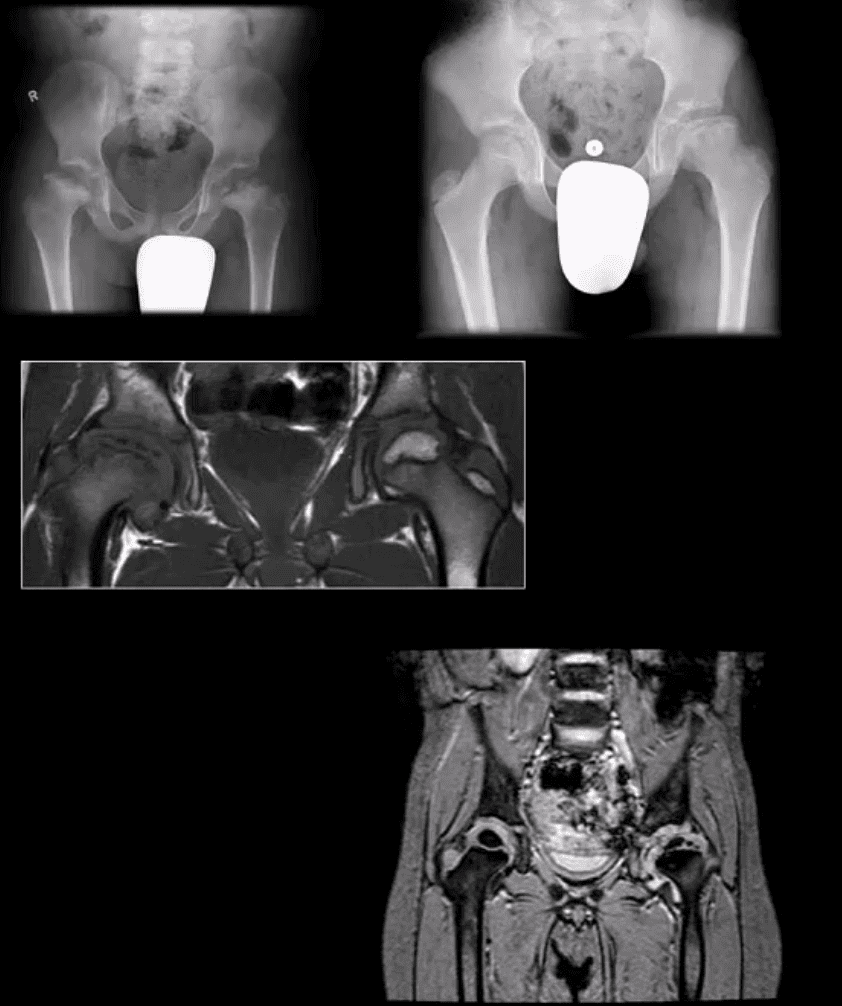
Coronal MRI Slice
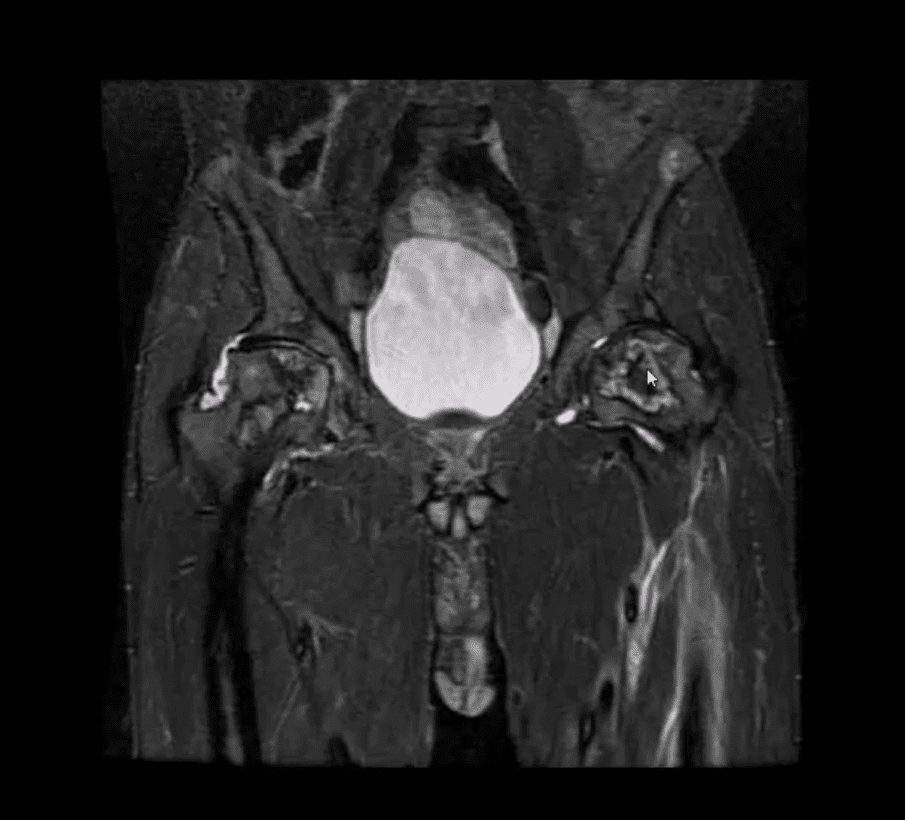
- Fluid sensitive sensitive coronal MRI slice revealing bill ischemic osteonecrosis of the femoral head
- MRI findings: l
Tc99-MMDP Radionuclide Bone
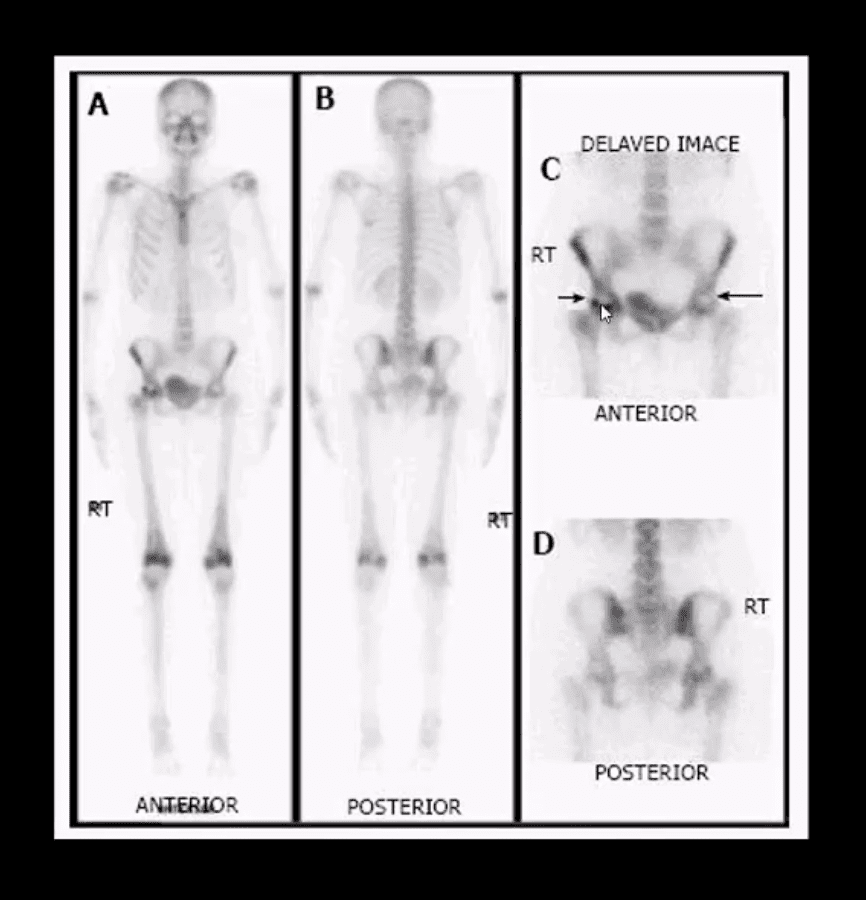
- Bone scan reveals central area of photopenia (cold spot) d/t necrotic fragment surrounded by increased osteoblastic activity as increased uptake of Tc-99 MDP in the right hip
- The patient is a 30-year-old female with breast cancer and chemotherapy treatment who suddenly presented with right hip pain
Radiographic Progression of AVN
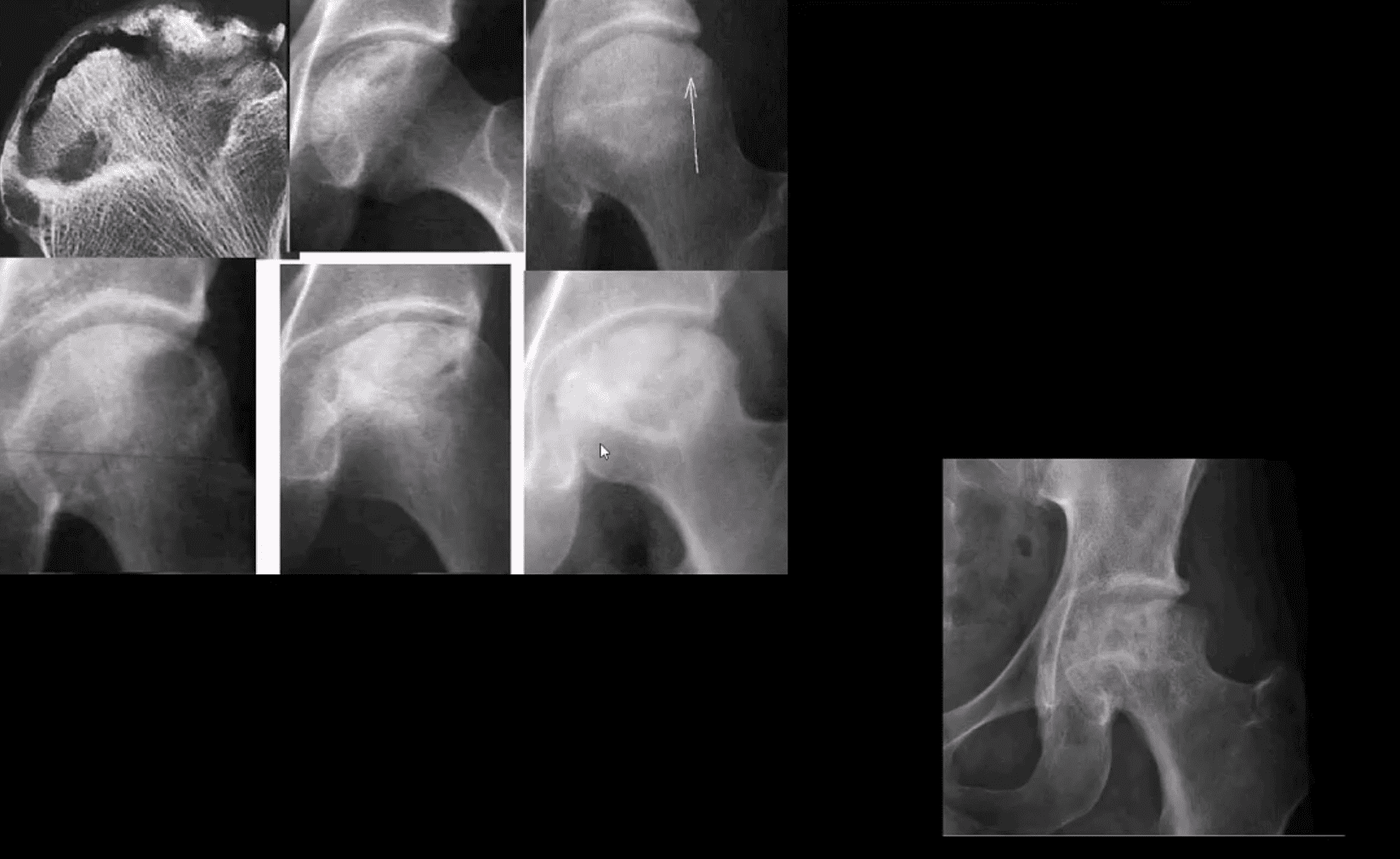
- Later stages present with articular collapse, subarticular cysts, increased patchy sclerosis and complete flattening of the femoral head with resultant severe DJD. Rx: THA
Management
- Early imaging Dx with MRI or bone scintigraphy is essential
- Referral to the Orthopedic surgeon
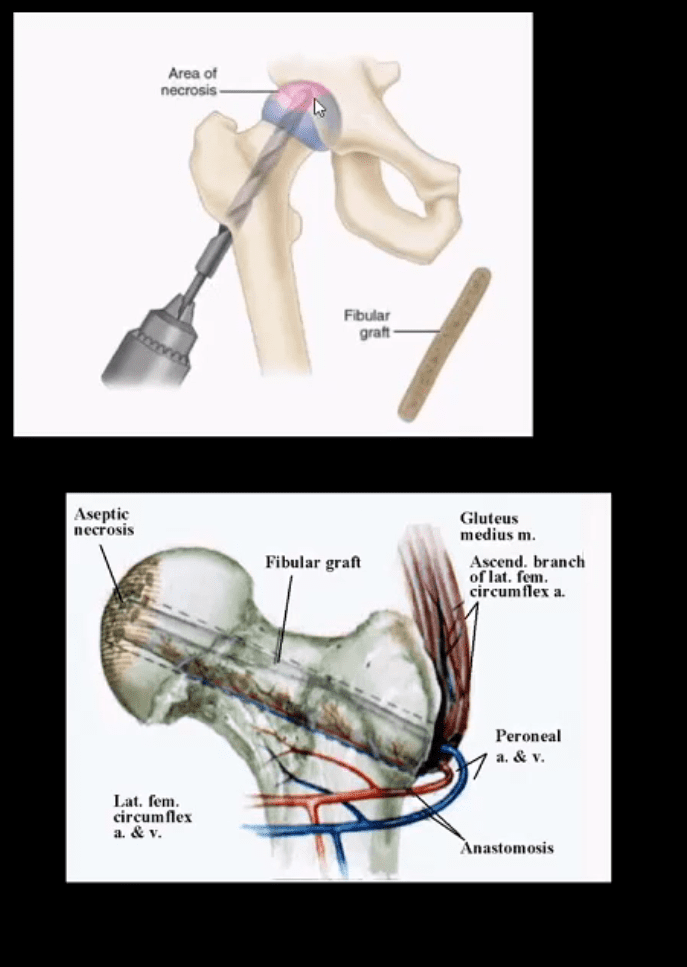
- Core decompression (above) can be used to revascularize the affected bone during earlier stages but produces mixed results
- Delayed changes of AVN: THA as IN severe DJD cases
B/L THA
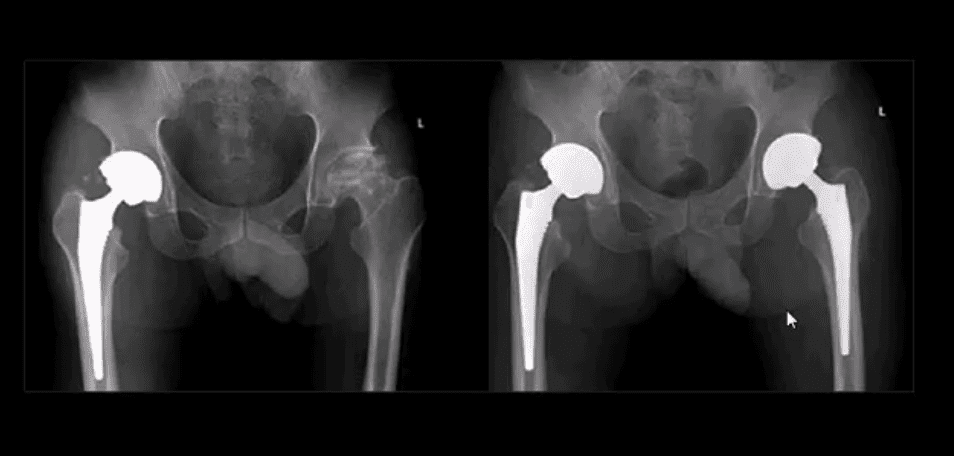
- B/L THA in the patient with ischemic osteonecrosis of the right and later left hip
- When B/L hip AVN is present, typically consider systemic causes (corticosteroids, diabetes)
Inflammatory Arthritis Affecting the Hip
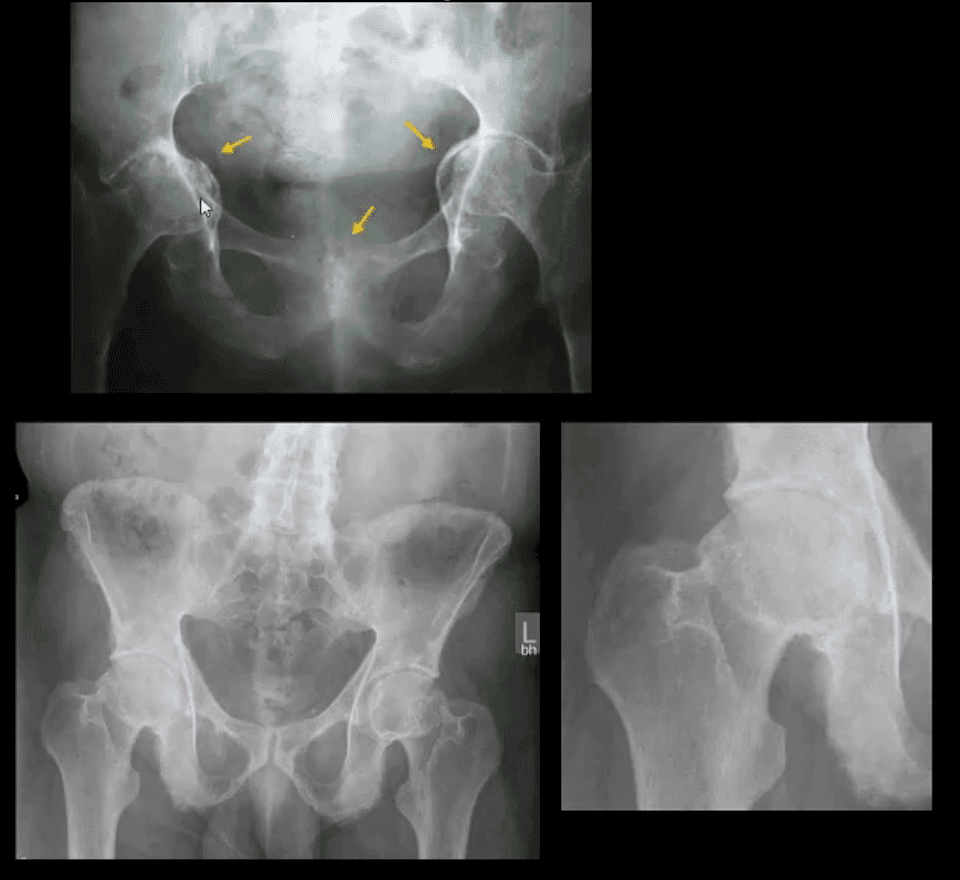
- Consider common systemic inflammatory condition such as RA and AS/EnA
- Hip RA may develop in 30% of patients with RA
- Key features to DDx inflammatory arthritis vs. DJD is symmertical/uniform aka concentric joint loss often leading to axial migration and Protrusion Acetabule in advanced cases
- Key feature between RA vs. AS: presence of RA bone erosion w/o productive bone changes or enthesitis in AS d/t inflammatory subperiosteal bone proliferation, whiskering/fluffy periostitis (collar-type enthesitis circumferentially affecting head-neck junction)
- Dx: Hx, PE, labs: CRP, RH, anti-CCP Ab (RA)
- CRP, HLA-B27, RF- (AS)
Septic Arthritis
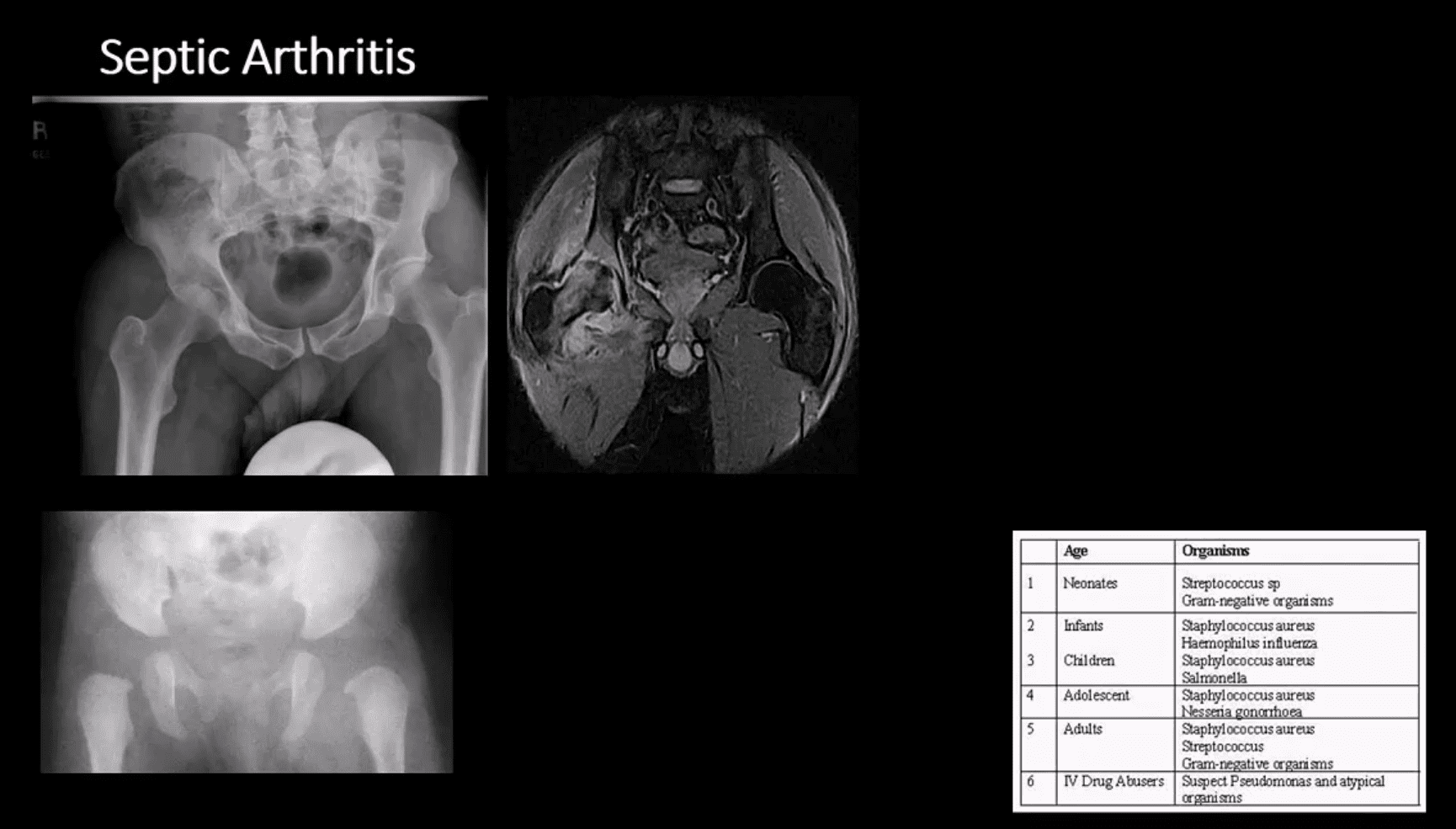
- Gonococcal infections, iatrogenic causes, I.V. drug use
and some others - Routes:
haematogenous ,adjecent spread, direct inoculation (e.g. iatrogenic) - Clinically: pain and reduced ROM presented as
mononarthritis , generalized signs/symptoms. CBC, ESR, CRP changes. ARthrocentesis and culture are crucial - M/C pathogen Staph. Aureus & Neisseria Gonorrhea
- 1st step: radiography, often unrewarding in the early stage. Later (4-10 days) indistinctness of
white cortical line at the femoral articular epiphysis, loss of joint space, effusion aswidening of medial joint space (Waldenstrom sign) - MRI – best at early DX: T1, T2, STIR, T1+C may help with early. Early I.V. antibiotics crucial to prevent rapid joint destruction
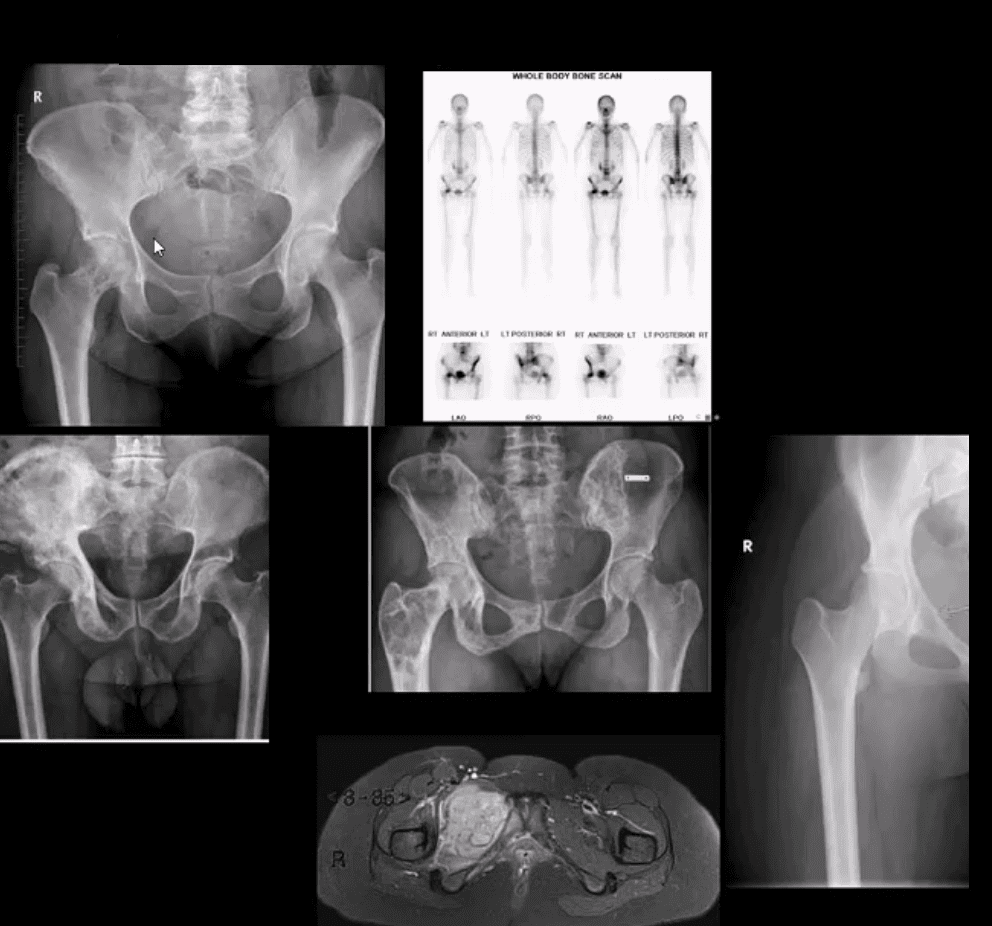
Slipped Capital Femoral Epiphysis (SCFE)
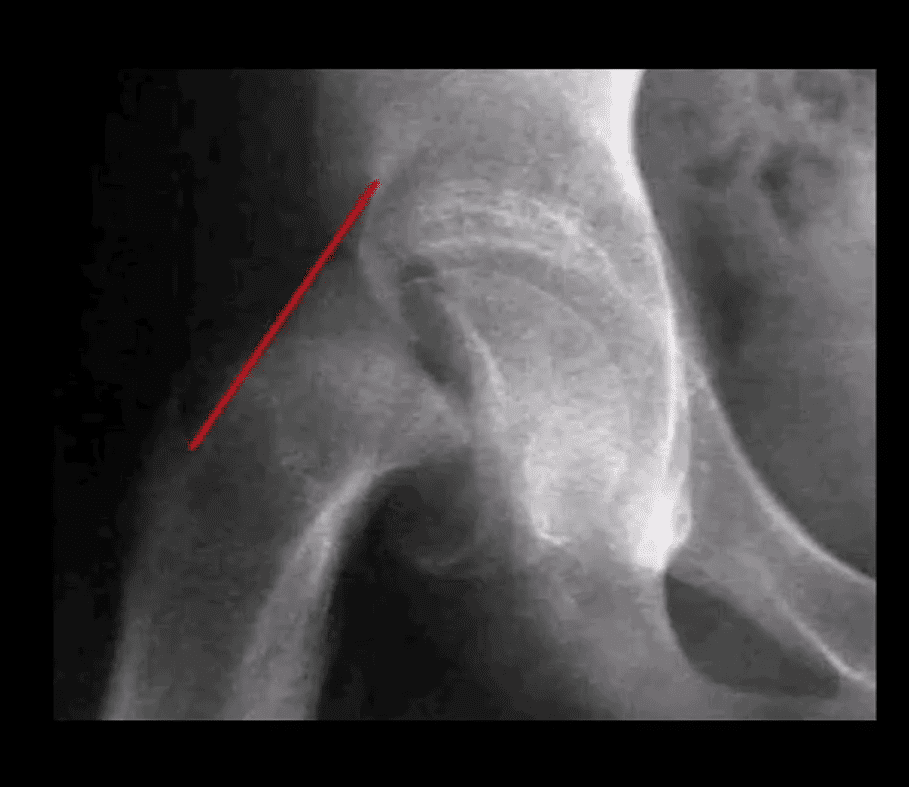
- Important to diagnose but easily missed potentially leading to Ischemic Osteonecrosis of the femoral head aka AVN
- Presents typically in overweight children (more often boys), age over 8 years. Greater incidence in African-American boys
- 1st step: radiography, especially look for a widened physeal growth plate (so-called pre-slip). Later, slip and disturbed Klein’s line (above image). MRI – best modality for early Dx and early intervention
- The frog lateral view often demonstrates the medial slip better than the AP view
Clinically Limping Child or Adolescent
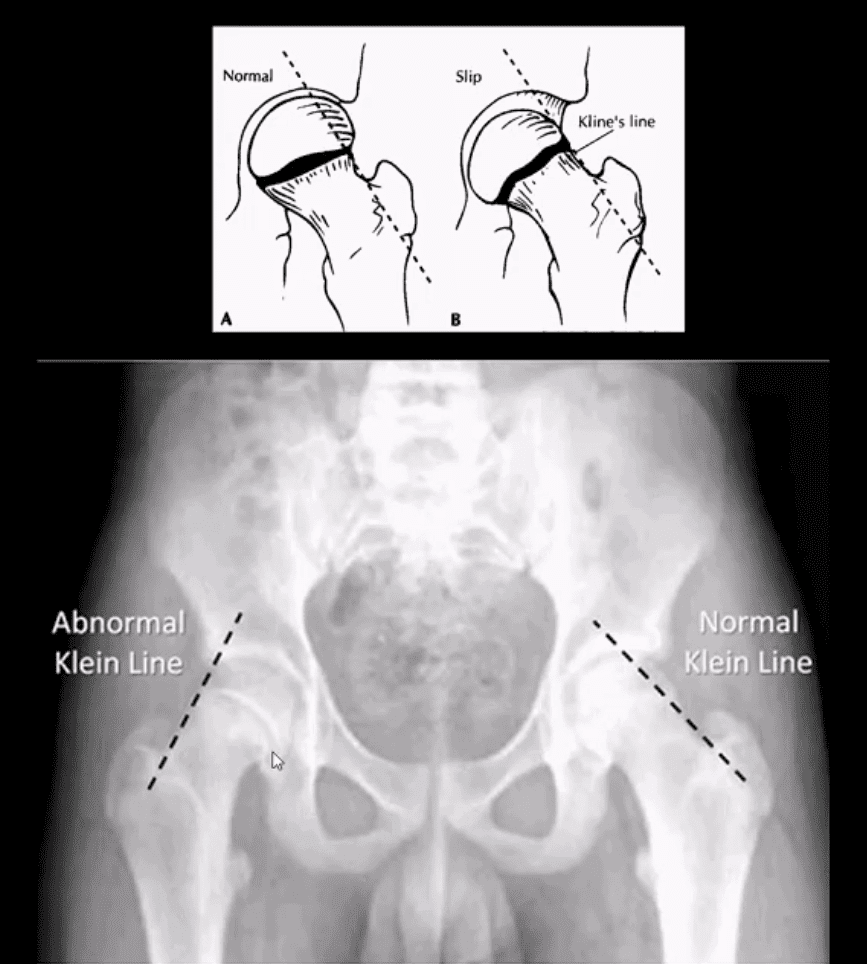
- M>F (10-18 years). African-Americans are at greater risk. 20% cases of SCFE are B/L. Complications: AVN >>DJD
- Radiography: AP pelvis, spot and frog leg may reveal slippage as Klein line failed to cross through the lateral aspect of the femoral head
- Additional features: physis may appear widened
- MRI w/o gad, is required for the earliest Dx and prevention of complications (AVN)
Normal and Abnormal Klein Line
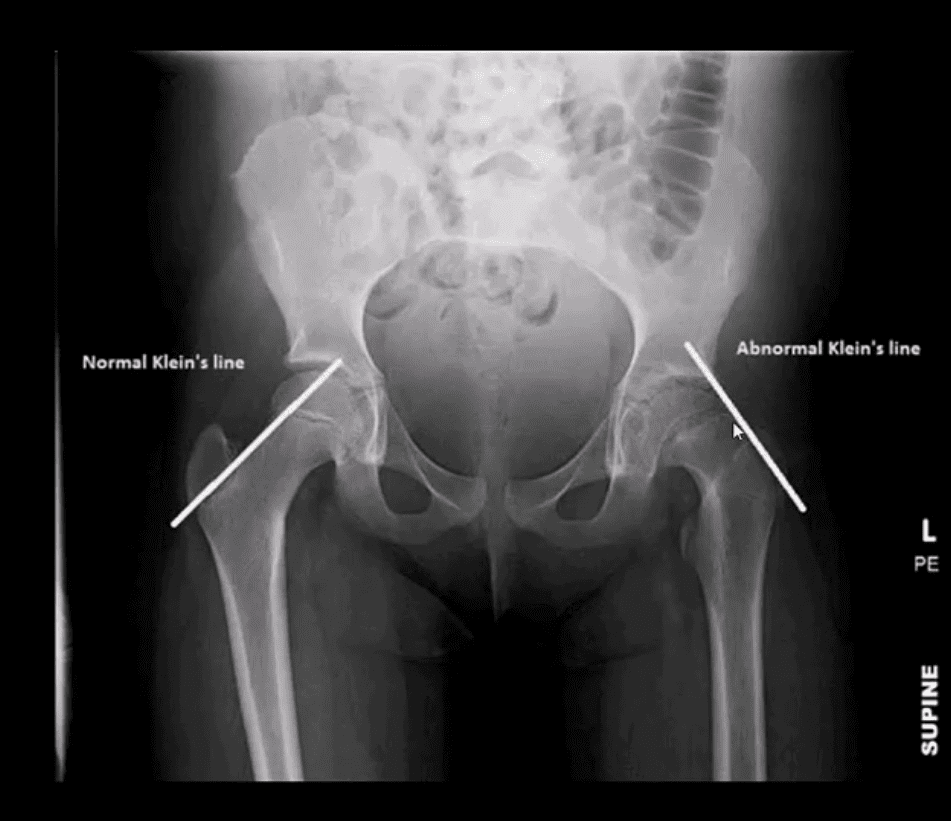
- Consistent with SCFE. The physis is also widened. Dx: SCFE
- Urgent referral to the pediatric Orthopedic surgeon
Subtle Changes in Left Hip
- Note suspected subtle changes in the left hip that may require MR examination to confirm the Dx
- Delay in care may result in major complications
Perthes’ Disease
- aka Legg-Calves-Perthes Disease (LCP)
- Refers to Osteochondritis of the femoral head with osteonecrosis likely d/t disturbed vascularization of the femoral head
- Presents typically in children (more often boys) aged under 8 years as atraumatic “limping child.” 15% may have B/L Perthe’s
- Imaging steps: 1st step x-radiography, followed by MRI especially in stage 1 (early) w/o x-ray abnormalities
- Unspecific signs: joint effusion with Waldenstrome sign+ (>2-mm increase in medial joint space compared to the opposite side). Past approach: Fluoroscopic Arthrography (replaced by MRI)
- Pathologic-Radiologic Correlation: in well-established cases, the femoral head characteristically becomes sclerotic, flattened and fragmented due to avascular necrosis (AVN). Later on, an occasional Coxa Magna changes may develop (>10% femoral head enlargement)
- Management: symptoms control, bracing. Boys at younger ate show better prognosis d/t more immaturity and better chances of bone/cartilage reparir mechansisms. In advanced cases, operative care: osteotomy, hip arthrpoplasty in adulthood if advanced DJD develops
Common Neoplasms & Other Conditions Affecting Hip/Pelvis
- M/C hip & pelvis neoplasms in adults: bone metatasis ( above far left), 2nd m/c Multiple Myeloma (M/C primary bone malignancy in adults). Tips: remember Red Marrow distribution. Less frequent: Chondrosarcoma
- Paget’s disease of bone (above-bottom left image) is m/c detected in the pelvis and Femurs
- Children and young adults ‘limping child’ benign neoplasms: Fibrous Dysplasia (above middle image), Solitary Bone Cyst (21%), Osteoid Osteoma, Chondroblastoma. Malignant pediatric neoplasms: m/c Ewing Sarcoma (above middle right and bottom images) vs. Osteosarcoma. >2y.o-consider Neuroblastoma
- Imaging: 1st step: radiography followed by MRI are most appropriate.
- If Mets are suspected: Tc99 bone scintigraphy is most sensitive
Multiple Myeloma
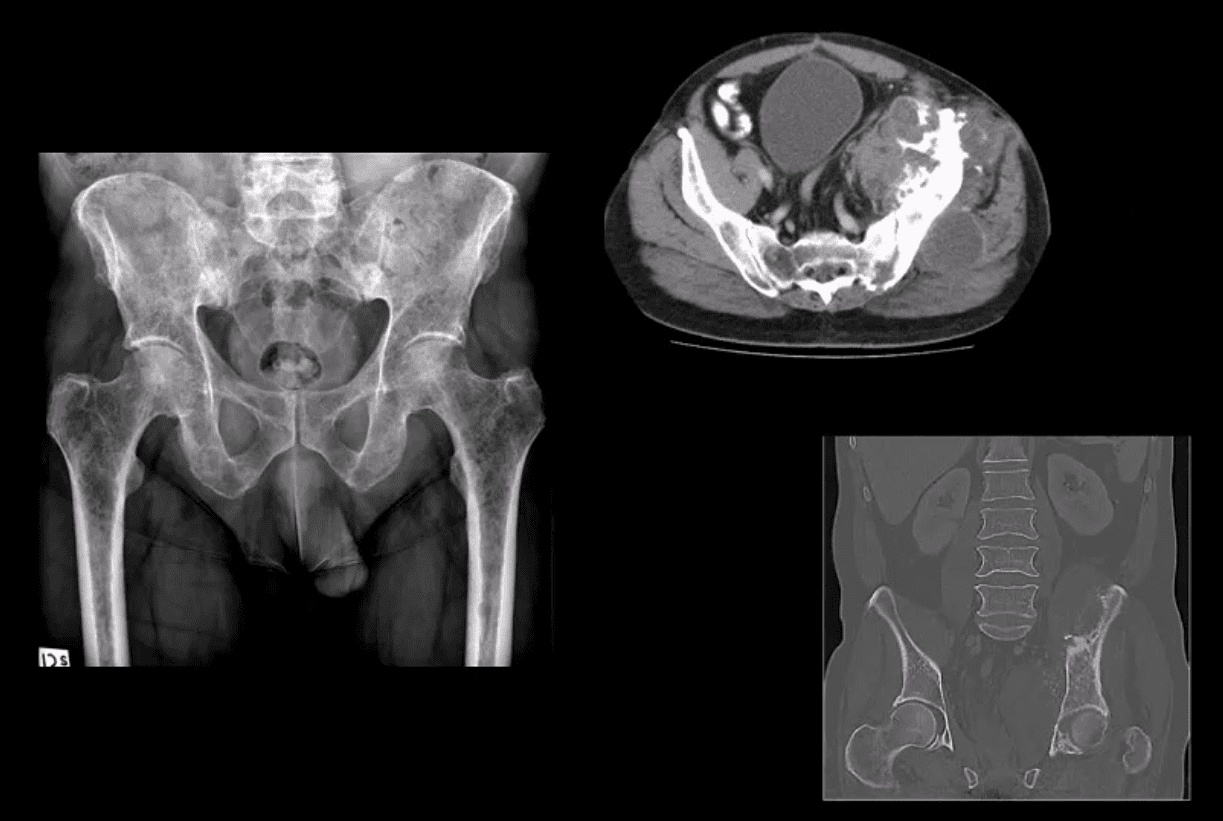
- Multiple Myeloma in a 75-y.o male (AP pelvis view)
- Chondrosarcoma in a 60-y.o male (axial and coronal reconstructed CT+C slices in bone window)
Hip Pelvis Arthritis & Neoplasms
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card