Individuals walking with a limp that results in pain could have an antalgic gait, an abnormal walking pattern commonly seen in emergency clinics and primary care offices. Can recognizing the symptoms help healthcare providers develop an effective treatment for the underlying cause?
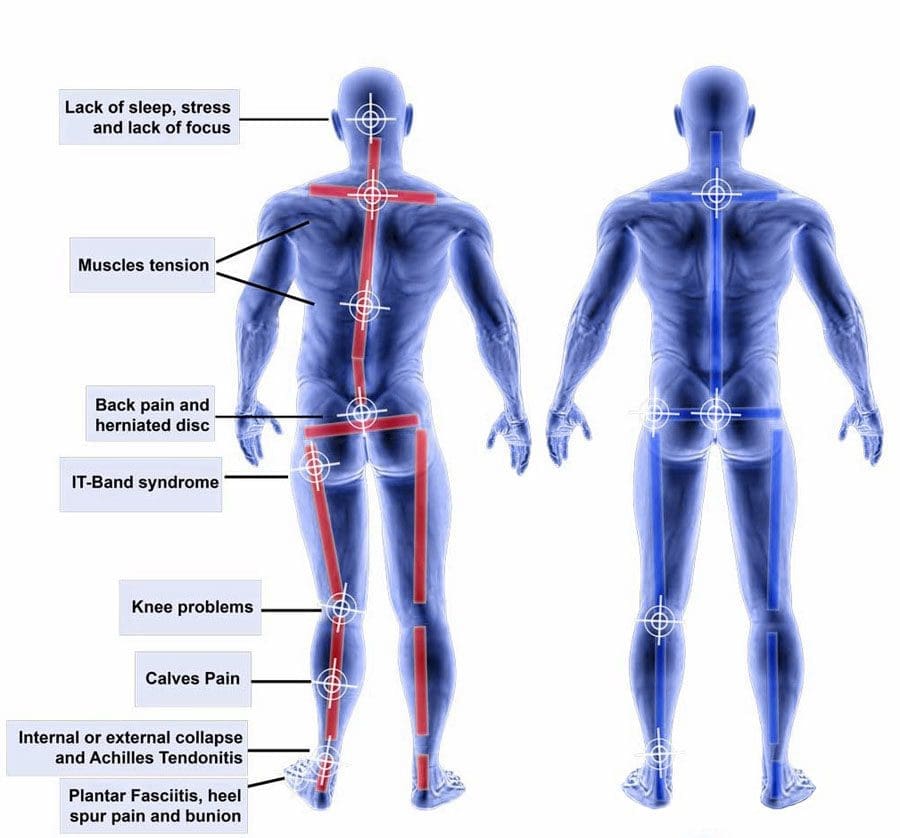
Table of Contents
Antalgic Gait
Limping and having an antalgic gait usually indicate a larger issue within the leg or lower back. It is the most common type of abnormal gait. There are various causes of antalgic gait, including acute injuries and gradually progressing medical conditions. The most common causes include osteoarthritis in one of the leg’s joints, lumbar radiculopathy, or an injury to a ligament or tendon. Paying attention to when the limping occurs, and any accompanying symptoms can help determine its origins.
Walking
When limping, the stance phase during walking is shorter than the swing phase. Individuals may widen their legs apart to provide a support base to compensate for the imbalance. In severe cases, an individual may swing their leg irregularly or take several side steps.
Causes and Symptoms
Antalgic gait can be caused by pain in any part of the lower extremity. Limping when walking may be a primary concern but is rarely the only complaint. Other associated symptoms may also be present, depending on the cause. These include:
- Limited range of motion
- Joint stiffness
- Muscular weakness
- Numbness and tingling
- Pain
- Swelling
- Leg instability or buckling
- Clicking or popping
Common Causes include:
Hip, knee, and/or Foot problems
When the hip, knee, ankle, or foot joints are injured or have some issue, walking can be painful and lead to a limp.
Sprains, Strains, or Soft-tissue Injuries
Sprains, strains, and soft-tissue injuries can result from acute injury or chronic, repetitive activities over time. (Pirker W. and Katzenschlager R. 2017) Sprains affect the body’s ligaments, while strains impact muscle tendons. However, sprains and strains occur when the impacted structure is overstretched or partially torn. The damage can lead to pain and antalgic gait. An injury to several other soft-tissue structures, including a bursa or fluid-filled sacs that reduce friction, meniscus, or fat pad, can also lead to limping. Symptoms typically include swelling, pain, and limited range of motion. More severe injuries can also make the leg feel unstable and cause it to give way when walking. Sometimes, bruising can also occur in the area of the injury. (American Academy of Orthopaedic Surgeons, 2020)
Osteoarthritis
Osteoarthritis occurs when the smooth, articular cartilage that lines the ends of bones begins to thin and deteriorate. This can alter the normal movement of a joint and lead to pain. Osteoarthritis symptoms gradually progress, affect individuals over 50, and worsen after periods of sedentary activity (Arthritis Foundation, Osteoarthritis, N.D.) Typically, it results in pain, stiffness, clicking, and occasionally swelling in the affected joint. These symptoms are usually worse in the morning and at the end of a long activity day. Moving around and warming the joint improves osteoarthritis symptoms. (Arthritis Foundation, Osteoarthritis, N.D.)
Lower Back Radiculopathy
Lumbar radiculopathy is when the nerve roots branching off the spine’s lower region become compressed or inflamed. This can occur because of disc issues like bulging, degeneration, herniation, bone spurring, or, rarely, a growth or tumor. (Johns Hopkins Medicine, 2024) Because these nerves control movement, sensation, and strength in the legs and feet, irritation in one can lead to limping. (Yokogawa N. et al., 2015) The antalgic gait from this condition frequently comes on suddenly and is commonly accompanied by back pain symptoms. This can include shooting pain and paresthesia in the leg. Depending on which nerve is involved, individuals may also experience muscular weakness in certain areas of the lower extremity. Sometimes, the affected leg feels like it will buckle while standing or walking. (Johns Hopkins Medicine, 2024)
Other causes include:
- Broken bones
- Tumors
- Infections
- Blood clots
- Vascular issues
Treatment
Treatment for antalgic gait depends on the underlying cause but can include:
- Rest, ice, and elevation are important for injuries. Individuals can control their initial symptoms by icing, elevating the leg, and resting from irritating activities.
- Activity modifications
- Antibiotics for infections
- Pain relievers
- Anti-inflammatories
- Physical therapy is also frequently initiated to strengthen the core and alleviate walking symptoms.
- Chiropractic realignment
- Non-surgical decompression
- Acupuncture
- A corticosteroid injection or joint replacement surgery may prove necessary in more advanced cases. (Arthritis Foundation, Osteoarthritis, N.D.)
- A spinal injection or surgery can reduce the pressure on the nerve root if conservative interventions fail to improve antalgic gait patterns. (Johns Hopkins Medicine, 2024)
- Crutches, canes, walkers, or assistive devices can reduce pressure traveling through an affected joint and improve overall walking quality. A study found that using a cane for two months helped reduce pain and improve function in individuals with knee osteoarthritis. (Fang M. A. et al., 2015)
Injury Medical Chiropractic and Functional Medicine Clinic
Though it can be tempting to ignore the limp and push through it, discussing the condition with a healthcare provider is important. A thorough medical exam and diagnostic tests, such as X-ray, MRI, or EMG, can help determine the underlying causes of a limp, help discover the cause of the problem, and help improve the quality of walking. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop personalized treatment programs. Using an integrated approach to treating injuries and chronic pain syndromes to improve flexibility, mobility, and agility and help individuals return to normal activities. Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers if other treatments are needed.
Chiropractic and Integrative Healthcare
References
Pirker, W., & Katzenschlager, R. (2017). Gait disorders in adults and the elderly : A clinical guide. Wiener klinische Wochenschrift, 129(3-4), 81–95. https://doi.org/10.1007/s00508-016-1096-4
Arthritis Foundation. (N.D.). Osteoarthritis. https://www.arthritis.org/diseases/osteoarthritis
American Academy of Orthopaedic Surgeons. (2020). Sprains, strains, and other soft-tissue injuries. https://orthoinfo.aaos.org/en/diseases–conditions/sprains-strains-and-other-soft-tissue-injuries/
Johns Hopkins Medicine. (2024). Radiculopathy. https://www.hopkinsmedicine.org/health/conditions-and-diseases/radiculopathy
Yokogawa, N., Toribatake, Y., Murakami, H., Hayashi, H., Yoneyama, T., Watanabe, T., & Tsuchiya, H. (2015). Differences in Gait Characteristics of Patients with Lumbar Spinal Canal Stenosis (L4 Radiculopathy) and Those with Osteoarthritis of the Hip. PloS one, 10(4), e0124745. https://doi.org/10.1371/journal.pone.0124745
Fang, M. A., Heiney, C., Yentes, J. M., Harada, N. D., Masih, S., & Perell-Gerson, K. L. (2015). Effects of contralateral versus ipsilateral cane use on gait in people with knee osteoarthritis. PM & R : the journal of injury, function, and rehabilitation, 7(4), 400–406. https://doi.org/10.1016/j.pmrj.2014.09.018
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


