Multiple sclerosis, or MS, is a chronic disease of the central nervous system, or CNS. While the etiology of the disease remains unknown, research studies have found that environmental factors, such as nutrition may impact the occurrence and development of MS. Other research studies specifically analyzed the association between certain dietary factors in multiple sclerosis cases, such as fat, dairy, and meat consumption. Multiple sclerosis, or MS, epidemiology suggests that dairy is primarily involved in the clinical expression of the disease. The purpose of the following article is to show the effects of cow’s milk allergy in multiple sclerosis patients.
Table of Contents
Abstract
Background: Exposure to some environmental agents such as different nutrition and contact with allergens may have a role in developing multiple sclerosis (MS). The present study was aimed to evaluate the cow’s milk allergy (CMA) in MS patients compared to healthy controls.
Materials and Methods: Between March 2012 and July 2012, 48 MS patients were selected and compared with 48 healthy subjects to assess the frequency of CMA in MS patients compared to healthy control. Immuno CAP determined cow’s milk-specific immunoglobin E (IgE). Sex and the frequency of CMA were compared between study groups by Chi-square test.
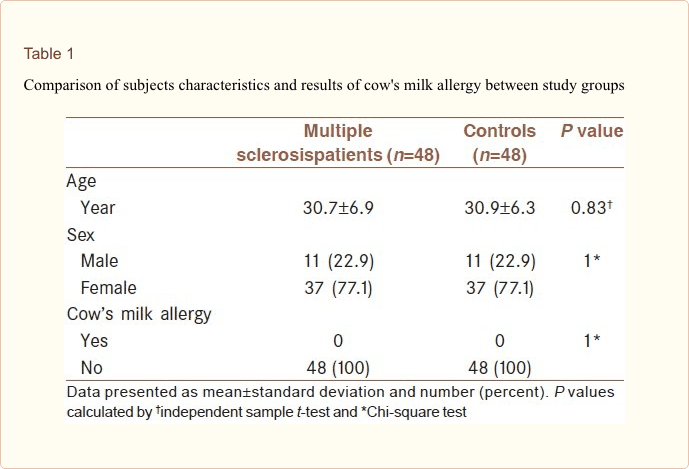
Results: A total of 96 subjects were assessed (22% male and 78% female). The mean age of the study subjects was 30.8 ± 6.6 years. The mean age of the case and control groups was 30.7 (±6.9) versus 30.9 ± 6.3, respectively (P-value = 0.83). There were no detection of cow’s milk-specific IgE in serum of MS patients and healthy subjects.
Conclusion: There was no difference between MS and healthy subjects regarding CMA.
Keywords: Allergy, cow’s milk, multiple sclerosis
Introduction
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease of the central nervous system (CNS)[1], and it is one among the common causes of neurological disability in young adults especially, women.[2] Autoimmune processes due to defects in regulatory T cells and failing of suppression auto-reactive CD4+ and CD8+ cells are suggested to have a role in the pathogenesis of the disease.[3]
Although the etiology of MS is unknown, there are some shreds of evidence for convolution with both genetic and environmental influences on susceptibility. Relative vitamin D deficiency,[4,5] Epstein-Barr virus,[6] and smoking[7] are among environmental factors that all have been associated with increased susceptibility to MS. Nutrition is another environmental factor that is possibly involved in the pathogenesis of MS.[8] Furthermore, dietary factors are frequently mentioned as a possible cause. There are very few clinical trials based on specific diets or dietary supplements in MS, and there is no evidence in this respect.[9] Higher intake of different food compounds was considered to be associated with increased risk of MS[9] such as sweets,[10] alcohol,[11,12,13] smoked meat products,[10] coffee, tea,[11] and yet, none of these data were approved by subsequent studies. In 1991, in a study, it had been reported that dietary factors or food allergies might be among the major causes of MS beginning and progression.[14] On the other hand, vitamin D has been implicated as a risk factor in MS [15,16,17], and it is reported that decreased levels of 25-hydroxyvitamin D are associated with an increased risk of developing MS.[18] Furthermore, the totality of evidence for a protective role of vitamin D in MS has been supposed strong enough by some to warrant recommending vitamin D supplementation to people with MS.[19] Cow’s milk allergy (CMA) has an indirect potential to cause 25-hydroxyvitamin D deficiency from affected individuals who tend to avoid dairy or cow’s milk products.[20]
In infancy, cow’s milk is the most frequently encountered dietary allergen, and CMA incidence varies with age.[21] In infants and adults, the reported prevalence of CMA varies between studies; however, it is clear that CMA is a common allergy in early childhood, with a prevalence of 2-6% [22] and decreases with age.[23]
It is believed that exposure to some environmental agent that occurs before puberty may begin the autoimmune process and pre-dispose a genetically susceptible person to develop MS later on. Based on this fact, the hypothesis of a link between milk consumption and MS was considered many years ago, and epidemiological studies were carried out to support this correlation.[24]
It is considered that the improvement of immunological defenses affects the treatment of MS patients. Therefore, detection of allergens and elimination of them from the diet could decrease the disability of patients,
The present study was aimed to evaluate the CMA in MS patients compared to healthy controls.
Materials and Methods
Between March 2012 and July 2012, 48 MS patients (referring to MS clinic of the referral university hospital in Isfahan) were selected and compared with 48 healthy subjects (among patients’ companions and acquaintances as a control group) to assess the association between CMA and MS. MS patients were diagnosed to develop MS according to the McDonald Criteria definitely.[25] Patients were eligible if they had not received corticosteroids during last month and immunosuppressants over the last 3 months. This study was investigated and approved by the ethics committee at the Isfahan University of Medical Sciences. All subjects were explained about the aim and the purposes of the study, and written informed consent was obtained from all of them.
Controls were matched with the patients regarding age and gender. To determine the allergen-specific immunoglobin E (IgE) of cow’s milk, blood samples were taken from both groups of subjects, and serum samples were transferred to the laboratory of Immunology.
ImmunoCAP (Phadia, Uppsala, Sweden) was used for allergen-specific IgE antibodies in the subjects’ serum to be obtained. This technique is approved by Food and Drug Administration in the US and has high sensitivity and many good features[26,27,28]. Also, in Iran is applicable only in the Asthma and Allergy Research Institute, Tehran University of Medical Sciences. Moreover, a specific IgE antibody against cow’s milk was determined and applying statistical techniques, calculations were performed, and results were extracted.
Data are presented as means ± standard deviation or number (%) as appropriate. An independent sample t-test was used to compare age between groups. Furthermore, sex and the frequency of CMA were compared between study groups by Chi-square test. The Statistical Package carried out all analysis for the Social Sciences (SPSS)-20, and statistical significance was accepted at P < 0.05.
Multiple sclerosis, or MS, is a multifactorial, inflammatory, and neurodegenerative disease of the central nervous system which has been demonstrated to be closely associated with environmental factors like nutrition. Recent research studies on the role of diet in MS provided evidence that certain dietary factors, such as the consumption of dairy products like cow’s milk, influence multiple sclerosis incidence, disease course and symptomatology. According to these research studies, particular types of proteins found in cow’s milk have been demonstrated to stimulate the immune system of people with MS.
Dr. Alex Jimenez D.C., C.C.S.T.
Results
A total of 96 subjects were assessed, and the results of all blood samples were analyzed. Of the total subjects, 22% were male, and 78% were female, and the mean age of the study subjects was 30.8 ± 6.6 years. Table 1 shows the comparison of age, gender, and the frequency of CMA between study groups. As shown mean age of in case and control groups was similar, and there was no statistically significant difference between groups (30.7 ± 6.9 vs. 30.9 ± 6.3 respectively, P-value = 0.83). Of 22 male subjects, 50% were MS patients, and 50% were controlled. There was no significant difference between study groups regarding gender composition. The CAP technique to determine allergen-specific IgE antibodies against cow’s milk in MS patients and healthy subjects showed no positive CMA in these subjects, and there was no difference between MS patients and healthy subjects.
Discussion
Since many years ago, the effect of diet such as fat intake in MS has been postulated.[29] There is a higher extent consumption of saturated fat, dairy products, and cornflakes (cereals) and a decrease in the consumption of unsaturated fat in areas with a high prevalence of MS.[29]
Though many case-control studies did not confirm the findings of these studies, epidemiological studies have proposed the association between MS prevalence and animal fat consumption.[11,12,13] Because MS is believed to have an autoimmune basis, many factors such as diet can induce autoimmunity and myelin breakdown by molecular mimicry.[30]
It seems that molecular mimicry may disrupt immunological self-tolerance to CNS myelin antigens in genetically susceptible individuals. CMA is one of the most common food allergens in infancy. It seems that the immune system identifies some of the proteins of milk as harmful and makes IgE antibodies neutralize them. IgE antibodies recognize these proteins in the next contact and signal the immune system to release some chemicals.[31]
Therefore, cow’s milk as a dietary protein has potential molecular mimicry with myelin autoantigens and may induce autoimmune process, so milk consumption in MS patients may have a possible role in progression or relapse of disease. Furthermore, as mentioned earlier, vitamin D has been implicated as a risk factor in MS patients[18]. CMA transmits nutritional implications as affected individuals tend to evade dairy products and be lacking in 25-hydroxyvitamin D.[20]
Measurement of specific IgE confirmed an IgE-mediated sensitivity to cow’s milk and is a prognostic marker for the persistence of CMA.[31]
In the present study, we evaluated the cow’s milk IgE to find allergy to milk in MS patients compared to control as a marker of persistence CMA. The result of the study did not show positive CMA in the MS group and no difference between MS patients and control subjects.
Our findings were similar to the result of the Ramagopalan et al. study.[32] Ramagopalan, in a population-based cohort in 2010, investigated whether or not childhood CMA influences the subsequent risk to develop MS. They collected data by telephone interview from mothers of 6638 MS index cases and 2509 spouse controls in Canada and compared the frequency of CMA between index cases and controls and could not find any significant differences. Therefore, the author concluded that childhood CMA does not appear to be a risk factor for MS.
Another study suggested that factors of liquid cow milk influence the clinical appearance of MS.[25]
Although medical interest in the influence of diet on the rate and severity of MS disease were carried out,[33] as our best knowledge, there are few studies in food allergens and MS, so further studies are suggested to be carried out to investigate food allergens, in a large number of MS patients. Healthy individuals based on individuals recall, then positive responses assess using advanced technique and results compared between MS patients and healthy subjects.
In summary, the findings of our study investigated that there is no difference between subjects developing MS and healthy subjects regarding CMA, and we could not find any association between CMA and MS.
Conclusion
This study evaluated the frequency distribution of cow milk allergy in MS patients compared to healthy controls. Although there was no significant difference between the two groups, the small sample size of MS patients may affect the association of this hypothesis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Multiple sclerosis, or MS, is a chronic disease of the central nervous system, or CNS, which is believed to be associated with environmental factors, such as nutrition. Research studies analyzing the association between certain dietary factors in multiple sclerosis demonstrated that dairy is primarily involved in the clinical expression of multiple sclerosis. The article’s purpose above was to show the effects of cow’s milk allergy in multiple sclerosis patients. According to the research study, dairy may affect the prevalence of MS, although further research studies are still required to conclude these findings further. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic and spinal health issues. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900.
Curated by Dr. Alex Jimenez
1. Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG. Multiple sclerosis. N Engl J Med. 2000;343:938–52. [PubMed] 2. Farinotti M, Simi S, Di Pietrantonj C, McDowell N, Brait L, Lupo D, et al. Dietary interventions for multiple sclerosis. Cochrane Database Syst Rev. 2007;24:CD004192. [PubMed] 3. Viglietta V, Baecher-Allan C, Weiner HL, Hafler DA. Loss of functional suppression by CD4+ CD25+ regulatory T cells in patients with multiple sclerosis. J Exp Med. 2004;199:971–9. [PMC free article] [PubMed] 4. Islam T, Gauderman WJ, Cozen W, Mack TM. Childhood sun exposure influences risk of multiple sclerosis in monozygotic twins. Neurology. 2007;69:381–8. [PubMed] 5. Munger KL, Zhang SM, O’Reilly E, Hernán MA, Olek MJ, Willett WC, et al. Vitamin D intake and incidence of multiple sclerosis. Neurology. 2004;62:60–5. [PubMed] 6. Handel AE, Williamson AJ, Disanto G, Handunnetthi L, Giovannoni G, Ramagopalan SV. An updated meta-analysis of risk of multiple sclerosis following infectious mononucleosis. PLoS One. 2010;5:1249. [PMC free article] [PubMed] 7. Hawkes CH. Smoking is a risk factor for multiple sclerosis: A metanalysis. MultScler. 2007;13:610–5. [PubMed] 8. Schwarz S, Leweling H. Multiple sclerosis and nutrition. MultScler. 2005;11:24–32. [PubMed] 9. Riccio P, Rossano R, Liuzzi GM. May diet and dietary supplements improve the wellness of multiple sclerosis patients? A molecular approach. Autoimmune Dis. 2011;2010:249842. [PMC free article] [PubMed] 10. Antonovsky A, Leibowitz U, Smith HA, Medalie JM, Balogh M, Kats R, et al. Epidemiologic study of multiple sclerosis in Israel. I. An overall review of methods and findings. Arch Neurol. 1965;13:183–93. [PubMed] 11. Tola MR, Granieri E, Malagù S, Caniatti L, Casetta I, Govoni V, et al. Dietary habits and multiple sclerosis. A retrospective study in Ferrara, Italy. Acta Neurol (Napoli) 1994;16:189–97. [PubMed] 12. Zhang SM, Willett WC, Hernán MA, Olek MJ, Ascherio A. Dietary fat in relation to risk of multiple sclerosis among two large cohorts of women. Am J Epidemiol. 2000;152:1056–64. [PubMed] 13. Sepci? J, Mesaros E, Materljan E, Sepi?-Grahovac D. Nutritional factors and multiple sclerosis in GorskiKotar, Croatia. Neuroepidemiology. 1993;12:234–40. [PubMed] 14. Sampson HA. Immunologic mechanisms in adverse reactions to foods. ImmunolAllergy Clin North Am. 1991;11:701–16. 15. Ramagopalan SV, Maugeri NJ, Handunnetthi L, Lincoln MR, Orton SM, Dyment DA, et al. Expression of the multiple sclerosis-associated MHC class II allele HLA-DRB1*1501 is regulated by vitamin D. PLoS Genet. 2009;5:e1000369. [PMC free article] [PubMed] 16. Correale J, Ysrraelit MC, Gaitán MI. Immunomodulatory effects of vitamin D in multiple sclerosis. Brain. 2009;132:1146–60. [PubMed] 17. Ascherio A, Munger KL. Environmental risk factors for multiple sclerosis. Part II: Noninfectious factors. Ann Neurol. 2007;61:504–13. [PubMed] 18. Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296:2832–8. [PubMed] 19. Pierrot-Deseilligny C. Clinical implications of a possible role of vitamin D in multiple sclerosis. J Neurol. 2009;256:1468–79. [PMC free article] [PubMed] 20. Yu JW, Pekeles G, Legault L, McCusker CT. Milk allergy and vitamin D deficiency rickets: A common disorder associated with an uncommon disease. Ann Allergy Asthma Immunol. 2006;96:615–9. [PubMed] 21. Wood RA. The natural history of food allergy. Pediatrics. 2003;111:1631–7. [PubMed] 22. Crittenden RG, Bennett LE. Cow’s milk allergy: A complex disorder. J Am Coll Nutr. 2005;24:582S–91. [PubMed] 23. Woods RK, Thien F, Raven J, Walters EH, Abramson M. Prevalence of food allergies in young adults and their relationship to asthma, nasal allergies, and eczema. Ann Allergy Asthma Immunol. 2002;88:183–9. [PubMed] 24. Malosse D, Perron H, Sasco A, Seigneurin JM. Correlation between milk and dairy product consumption and multiple sclerosis prevalence: A worldwide study. Neuroepidemiology. 1992;11:304–12. [PubMed] 25. McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–7. [PubMed] 26. Bernstein JA, Bernstein IL, Bucchini L, Goldman LR, Hamilton RG, Lehrer S, et al. Clinical and laboratory investigation of allergy to genetically modified foods. Environ Health Perspect. 2003;111:1114–21. [PMC free article] [PubMed] 27. Pastorello EA, Incorvaia C, Pravettoni V, Bonini S, Canonica GW, Ortolani C, et al. A multicentric study on sensitivity and specificity of a new in vitro test for measurement of IgE antibodies. Ann Allergy. 1991;67:365–70. [PubMed] 28. Paganelli R, Ansotegui IJ, Sastre J, Lange CE, Roovers MH, de Groot H, et al. Specific IgE antibodies in the diagnosis of atopic disease. Clinical evaluation of a new in vitro test system, UniCAP, in six European allergy clinics. Allergy. 1998;53:763–8. [PubMed] 29. Swank RL, Dugan BB. Effect of low saturated fat diet in early and late cases of multiple sclerosis. Lancet. 1990;336:37–9. [PubMed] 30. Wekerle H, Hohlfeld R. Molecular mimicry in multiple sclerosis. N Engl J Med. 2003;349:185–6. [PubMed] 31. Ahrens B, Lopes de Oliveira LC, Grabenhenrich L, Schulz G, Niggemann B, Wahn U, et al. Individual cow’s milk allergens as prognostic markers for tolerance development? Clin Exp Allergy. 2012;42:1630–7. [PubMed] 32. Ramagopalan SV, Dyment DA, Guimond C, Orton SM, Yee IM, Ebers GC, et al. Childhood cow’s milk allergy and the risk of multiple sclerosis: A population based study. J Neurol Sci. 2010;291:86–8. [PubMed] 33. Payne A. Nutrition and diet in the clinical management of multiple sclerosis. J Hum Nutr Diet. 2001;14:349–57. [PubMed]

Additional Topic Discussion: Acute Back Pain
Back pain is one of the most prevalent causes of disability and missed days at work worldwide. Back pain attributes to the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience back pain at least once throughout their life. The spine is a complex structure made up of bones, joints, ligaments, and muscles, among other soft tissues. Injuries and/or aggravated conditions, such as herniated discs, can eventually lead to back pain symptoms. Sports injuries or automobile accident injuries are often the most frequent cause of back pain. However, sometimes the simplest of movements can have painful results. Fortunately, alternative treatment options, such as chiropractic care, can help ease back pain through the use of spinal adjustments and manual manipulations, ultimately improving pain relief.

EXTRA EXTRA | IMPORTANT TOPIC: Recommended El Paso, TX Chiropractor?
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card