Cardiovascular disease, also called heart disease, involves numerous issues, including diseased vessels, structural problems, and blood clots. High blood pressure, or hypertension, occurs when your blood pressure increases to unhealthy levels. Your blood pressure measurement takes into account how quickly blood is passing through your veins and the amount of resistance the blood meets while it’s pumping.
Table of Contents
What are the leading causes of cardiovascular disease and hypertension?
Oxidative stress, inflammation and autoimmune dysfunction initiate and propagate hypertension and cardiovascular disease. In a series of research studies correlated to cardiovascular disease and hypertension, Dr. Mark C. Houston, MD, discussed the role that oxidative stress, inflammation and autoimmune dysfunction plays in relation to treatment of hypertension and cardiovascular disease.
Oxidative Stress
Oxidative stress, with an imbalance between the defense mechanisms and RNS as well as ROS, contributes to the etiology of hypertension in humans and animals. Radical oxygen species and RNS are generated by numerous mobile sources, such as nicotinamide adenine dinucleotide phosphate hydrase (NADPH) oxidase, mitochondria, xanthine oxidase, uncoupled endothelium-derived nitric oxide (NO) synthase (U-eNOS), cyclo-oxygenase and lipo-oxygenase. Superoxide anion is your predominant ROS species produced with these tissues, which inhibits NO and also leads to downstream production of additional ROS (As seen in Figure 3).
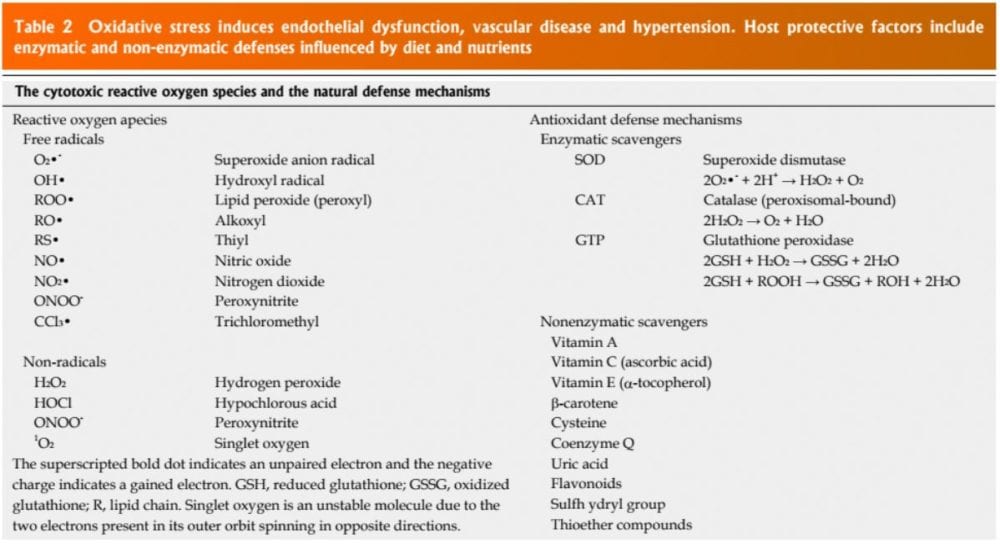
Patients have impaired an oxidative stress reaction to several stimuli, an elevated plasma oxidative stress and exogenous and endogenous antioxidant defense mechanisms. Hypertensive subjects also have lower plasma ferric reducing ability of plasma vitamin C levels and increased plasma 8-isoprostanes, which correlate with both diastolic and systolic BP. Different single-nucleotide polymorphisms (SNP’s) in genes that codify for antioxidant enzymes are directly linked to hypertension. These include NADPH oxidase, xanthine oxidase, superoxide dismutase 3 (SOD 3), catalase, glutathione peroxidase 1 (GPx 1) and thioredoxin. Antioxidant deficiency and excess free radical production have been implicated in human hypertension in several epidemiologic, observational and interventional studies (Table 2).
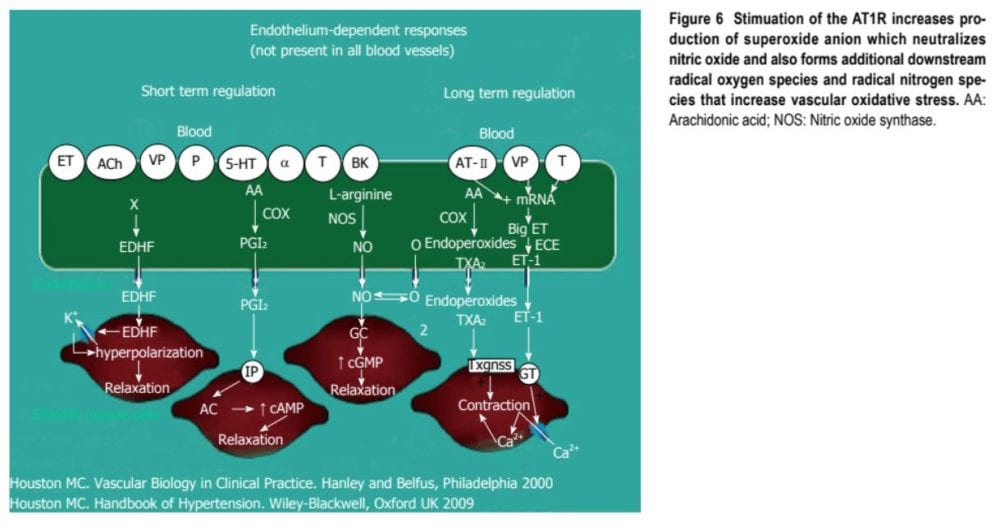
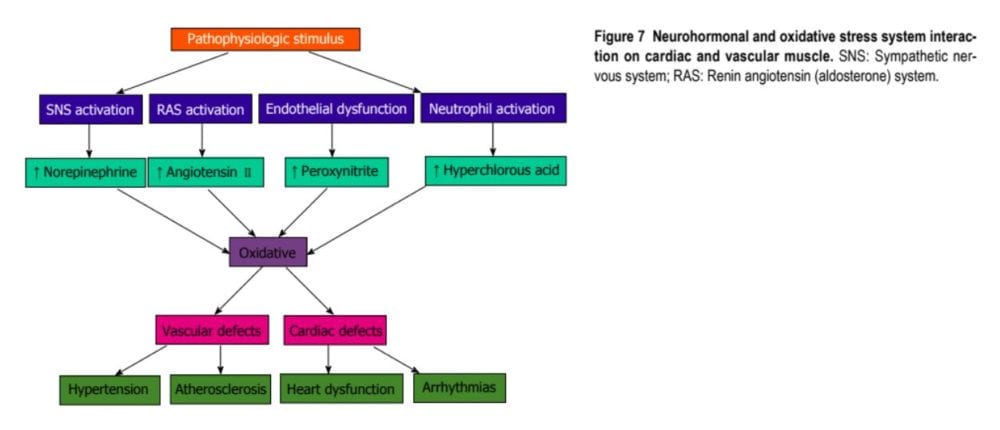
Radical oxygen species directly damage endothelial cells, degrade NO, influence eicosanoid metabolism, oxidize LDL, lipids, proteins, proteins, DNA and natural molecules, boost catecholamines, harm the genetic machinery, affect gene expression and transcription factors. The interrelations of systems, oxidative stress and cardiovascular disease are shown in Figures 6 and 7. The increased oxidative stress, inflammation and autoimmune vascular dysfunction in human hypertension results in a combination of an response to ROS and RNS increased generation of ROS and RNS and a decreased antioxidant reserve. Increased oxidative stress from the rostral ventrolateral medulla (RVLM) enhances glutamatergic excitatory inputs and attenuates GABA-ergic inhibitory inputs into the RVLM which contributes to increased sympathetic nervous system (SNS) activity from the paraventricular nucleus. Activation of this AT1R in the RVLM raises NADPH oxidase and increases oxidative stress and superoxide anion, increases SNS outflow causing an imbalance of SNS/PNS action with elevation of BP, increased heartbeat and alterations in heart rate variability and heart rate recovery time, which can be obstructed by AT1R blockers.
Inflammation
The link between hypertension and inflammation was suggested in both longitudinal and cross-sectional studies. Raised in high sensitivity C-reactive protein (HS-CRP) and other inflammatory cytokines such as interleukin-1B, (IL-1B), IL-6, tumor necrosis alpha (TNF-?) and chronic leukocytosis occur in hypertension and hypertensive-related TOD, such as increased carotid IMT. HS-CRP predicts CV events. Elevated HS-CRP is risk factor and a risk marker for hypertension and CVD. Increases in HS-CRP of over 3 ?g/mL can increase BP in only a couple of days that is directly proportional to the increase in HS-CRP. ENOS and nitric oxide are inhibited by HS-CRP. HS-CRP, down-regulates the AT2R, that counterbalances AT1R. Angiotensin II (A-II) upregulates many of those cytokines, notably IL-6, CAMs and chemokines by activating nuclear factor Kappa B (NF-?B) resulting in vasoconstriction. These events, as well as the increases in endothelin-1 and oxidative stress, elevate BP.
Autoimmune Dysfunction
Innate and adaptive immune responses are associated with hypertension and hypertension-induced CVD through at least three mechanisms: central nervous system stimulation cytokine generation and renal impairment. This includes salt-sensitive hypertension with dysregulation of both CD4+ and CD8+ lymphocytes increased inflammation because of T cell imbalance and chronic leukocytosis with increased neutrophils and lymphocytes that are decreased. Leukocytosis, especially neutrophils and decreased lymphocyte count raise BP in Blacks by. Macrophages and invade the wall, trigger TLRs, various subtypes govern BP and cause autoimmune vascular damage. Angiotensin II activates immune cells (T cells, macrophages and dendritic cells) and promotes cell infiltration into target organs. CD4+ T lymphocytes express AT1R and PPAR gamma receptors, and release TNF-?, interferon and interleukins inside the vascular wall when triggered (Figure 5). May play a role in the genesis of hypertension brought on by Angiotensin II. Patients have higher TLR 4 mRNA in monocytes in comparison to normal. Intensive decrease in BP to systolic BP (SBP) less than 130 mmHg vs SBP to just 140 mmHg reduces the TLR 4 longer. A-II activates the TLR expression resulting in inflammation and activation of the innate immune system. When TLR 4 is triggered there is downstream macrophage activation, increase metalloproteinase 9, migration, vascular remodeling, collagen accumulation in LVH the gut and cardiac fibrosis. The autonomic nervous system is essential in either increasing or decreasing inflammation and immune dysfunction. Efferent cholinergic pathways through the nerve innervate the spleen, nicotine acetylcholine receptor subunits and cytokine producing immune cells to BP and affect vasoconstriction. Nearby CNS inflammation or ischemia may mediate vascular hypertension and inflammation.
Aldosterone is correlated with increased adaptive immunity and autoimmune responses with CD4+ T cell activation and Th 17 polarization with improved IL 17, TGF-? and TNF-? which modulate over 30 inflammatory genes. Serum aldosterone is also an independent risk factor for CVD and CHD via non-hemodynamic effects as well as through increased BP. Blockade of receptors in brain, the heart, blood vessels and immune cells reduces CV danger even with the persistence of hypertension.
In conclusion, cardiovascular disease and hypertension have been associated with numerous issues, however, oxidative stress, inflammation and autoimmune dysfunction have been regarded as the most prevalent causes behind cardiovascular disease and hypertension. Oxidative stress, defined as a disturbance in the balance between the production of reactive oxygen species (free radicals) and antioxidant defenses, inflammation and autoimmune dysfunction, occurs when the body’s immune system attacks and destroys healthy body tissue by mistake. Cardiovascular disease and hypertension is an indication of cardiovascular issues which should be addressed by a healthcare professional.
The scope of our information is limited to chiropractic and spinal injuries and conditions. To discuss options on the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 . 
By Dr. Alex Jimenez
Additional Topics: Wellness
Overall health and wellness are essential towards maintaining the proper mental and physical balance in the body. From eating a balanced nutrition as well as exercising and participating in physical activities, to sleeping a healthy amount of time on a regular basis, following the best health and wellness tips can ultimately help maintain overall well-being. Eating plenty of fruits and vegetables can go a long way towards helping people become healthy.

TRENDING TOPIC: EXTRA EXTRA: About Chiropractic
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


