A bone graft is defined as using bone in fusion surgery. Fusion surgery’s purpose is to link or weld bones together, in this case, the spinal bones. There are a variety of spinal conditions that cause instability and pain:
- Degenerative disc disease
- Scoliosis
- Trauma from an auto accident, sports injuries, slip and fall accident
Spine surgeons use a bone graft to:
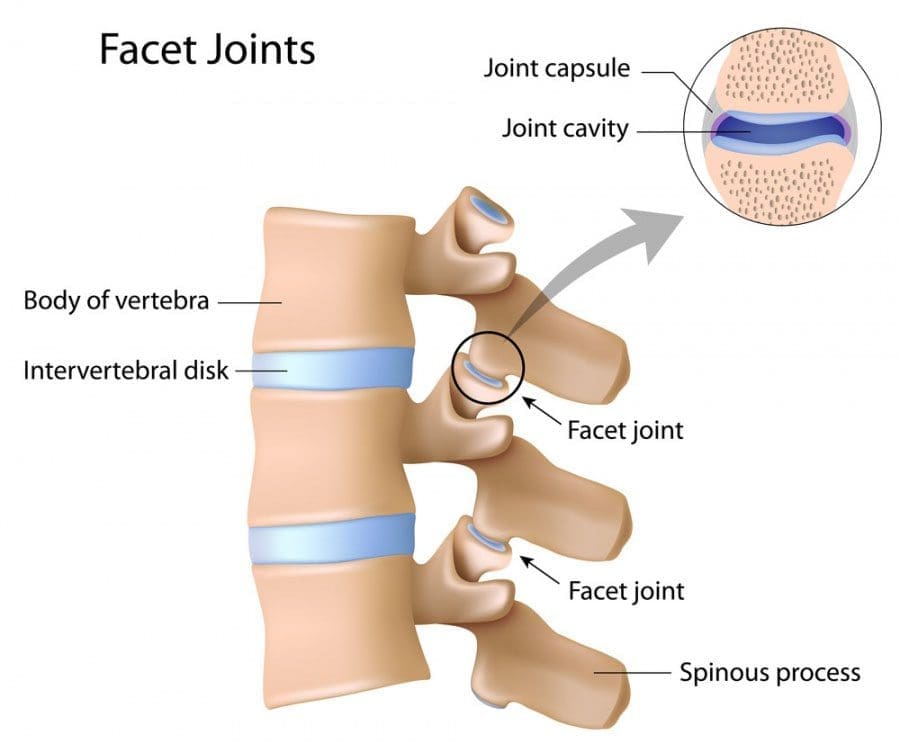
- Stop motion between two or more vertebrae
- Stabilize a spinal deformity
- Repair fractures of the spine

Table of Contents
Spinal Fusion Stimulates New Bone Growth
A bone graft does not heal or fuse the spine instantly. Rather a bone graft sets up a foundational frame for the individual’s body to generate and grow new bone. A bone graft stimulates new bone production. When this new bone begins to grow and solidify, that fusion takes place.
With these types of surgeries, instrumentation like screws and rods is typically used for the beginning stabilization. But the actual healing of the bone welds the vertebrae together, creating long-term stability.
A bone graft can be used for structural purposes for supporting the spine; usually, this is done in place of a disc or bone that was removed. Or it can be an onlay, which means that a mass of bone fragments will grow together to stabilize the spine bridging the joint.
There are two generalized bone graft types:
- Real bone
- Substituted bone graft
Real bone can come from the patient, an autograft, or the donor’s bone called an allograft.
The Individual’s Bone or Auto-graft
An auto-graft is bone taken or harvested from the individual’s body and transplanted to a specific area, in this case, the spine. An auto-graft is considered the gold standard because it is the individual’s own bone, which contains:
- Bone cells
- Proteins
- Calcified matrix
These all help to stimulate the healing of the fusion. There are advantages to an auto-graft, which include a higher probability of fusion success and a lower risk for disease transmission. The only real setback for individuals of an auto-graft is the post-operative pain that usually comes with the procedure when harvesting an individual’s bone. Bone can be harvested from one of the individuals:
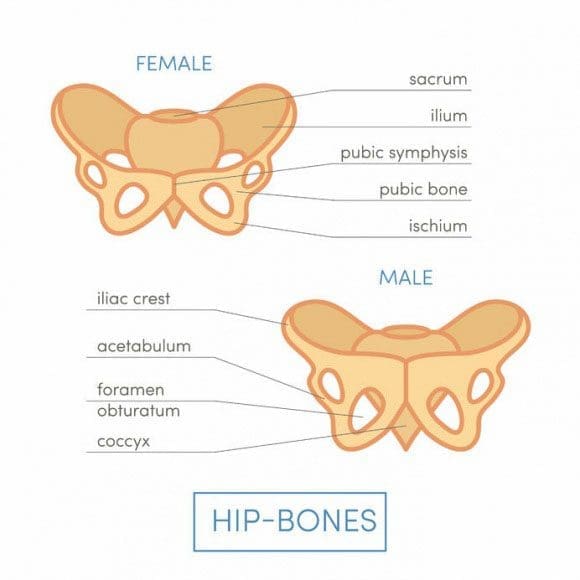
- Iliac crests
- Pelvic bones
- Ribs
- Spine
Bone graft harvesting creates a new set of risks. These include:
- Post-operative pain
- Nerve injury
- Surgical wound issues
Because of these risks and the possibility that the bone could be of poor quality, a surgeon could decide to use another type of bone graft. When this happens, a surgeon could go with what is known as a local auto-graft. This is bone harvested from the decompression itself.
These are the parts that are removed to decompress the nerves. They usually consist of bone spurs, lamina, and portions of the spinous process. These same bone pieces can be reused to assist with the fusion of the decompressed areas.
Donor Bone or Allograft
An allograft is a bone harvested from another person, usually from a tissue bank. Tissue banks harvest bone and other tissues from cadavers for medical purposes. An allograft is prepared by freezing or freeze-drying the bone or tissues. This helps limit the risk of graft rejection. Bone from an allograft does not have living bone cells and is less effective at fusion stimulation than an autograft. However, it still does work. Tissue banks:
- Screen all their donors
- Supervise bone recovery
- Test donations
- Sterilize donations
- Store for use
Look for tissue banks accredited by the American Association of Tissue Banks. US Food and Drug Administration has strict human cell and tissue processing regulations. These include rules about the eligibility of donors. These guidelines/protocols help reduce the risk of tissue contamination and the spread of disease.
Bone Graft Substitute
These substitutes are man-made or made from a modified version of a natural product. These alternatives are safe and can provide a solid foundation for the individual’s body to grow bone. Substitutes have similar properties to human bone, including a porous structure and proteins stimulating healing.
Demineralized Bone Matrix – DBM
A demineralized bone matrix is an allograft that has gone through a process where the mineral content has been removed. This demineralization helps reveal bone-forming proteins like collagen and growth factors hidden within the bone that can stimulate healing.
This procedure is often considered a bone graft extender. It is not considered a replacement. This is because its ability to fuse the human spine has not been proven. DBM can be combined with regular bone for more volume and is available in these forms:
- Chip
- Granule
- Gel
- Powder
- Putty
Ceramic-based Extenders
Ceramic-based extenders are mixed in combination with other sources of bone. This is because they consist of a calcium matrix for fusion, but there are no cells or proteins to stimulate the healing process. These include:
- Calcium phosphate
- Calcium sulfate
- Bioactive glass
Ceramic-based extenders do not present a risk for disease transfer but can cause inflammation. They are available in porous and mesh forms.
Morphogenetic Protein – BMP
Different bone morphogenetic proteins, or BMPs, stimulate new bone growth. These proteins are found in human bone; however, they are in trace amounts. They are then produced in larger amounts through genetic engineering.
This all depends on the type of spine surgery an individual undergoes. Bone morphogenetic protein could be considered an option for promoting new bone growth and healing fusion.
Treating Severe & Complex Sciatica Syndromes
Telemedicine Mobile App
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



