Chiropractor, Dr. Alexander Jimenez looks at the way this common injury shows itself.
Table of Contents
Introduction
Iliotibial band syndrome (ITBS) between the knee is frequently diagnosed in sport injury clinics. ITBS presents having an incidence rate of around 22% in most lower extremity running-related injuries (1) also has been said to be the second most common complaint amongst distance runners (2). ITBS has been given the expression ‘runner’s knee’.
Trainers like endurance runners who perform flexion and extension combined with loading are subjected to this illness. ITBS presents during the first two or three miles in running with no mechanism of injury, which can make identifying the cause more interesting. With plenty of factors having been considered within the literature, changes are often purported to be a cause of ITBS. But some biomechanical factors have been researched and have been found to have little or no effect in the start of ITBS. Therefore this text’s point would be to examine the biomechanical changes which may induce an individual to the beginning of ITBS. The research published reviewed is largely based on a current systematic review that was published in Physical Therapy in Sport in 2014 (3).
Anatomy & Function
The iliotibial band (ITB) encapsulates the tensor fascia latae (TFL) presenting with both deep and superficial fibre attachments at the pelvis (4). In addition to attaching to the TFL, approximately three-quarters of the gluteus maximus tendon also conjoins with the ITB (4). The ITB courses along the lateral aspect of the hip and passes the greater trochanter. The ITB maintains an attachment on the posterior ridge of the femur whilst attaching itself to the fascia. The ITB has a fixed attachment at the lateral femoral condyle where it then divides into three segments with the first being the lateral patella (3). The remaining two segments cross the knee joint to insert at the head of fibula and most distally at the infrapatellar tubercle also known as Gerdy’s tubercle on the tibia (3). Figure 1 illustrates the location of the ITB.
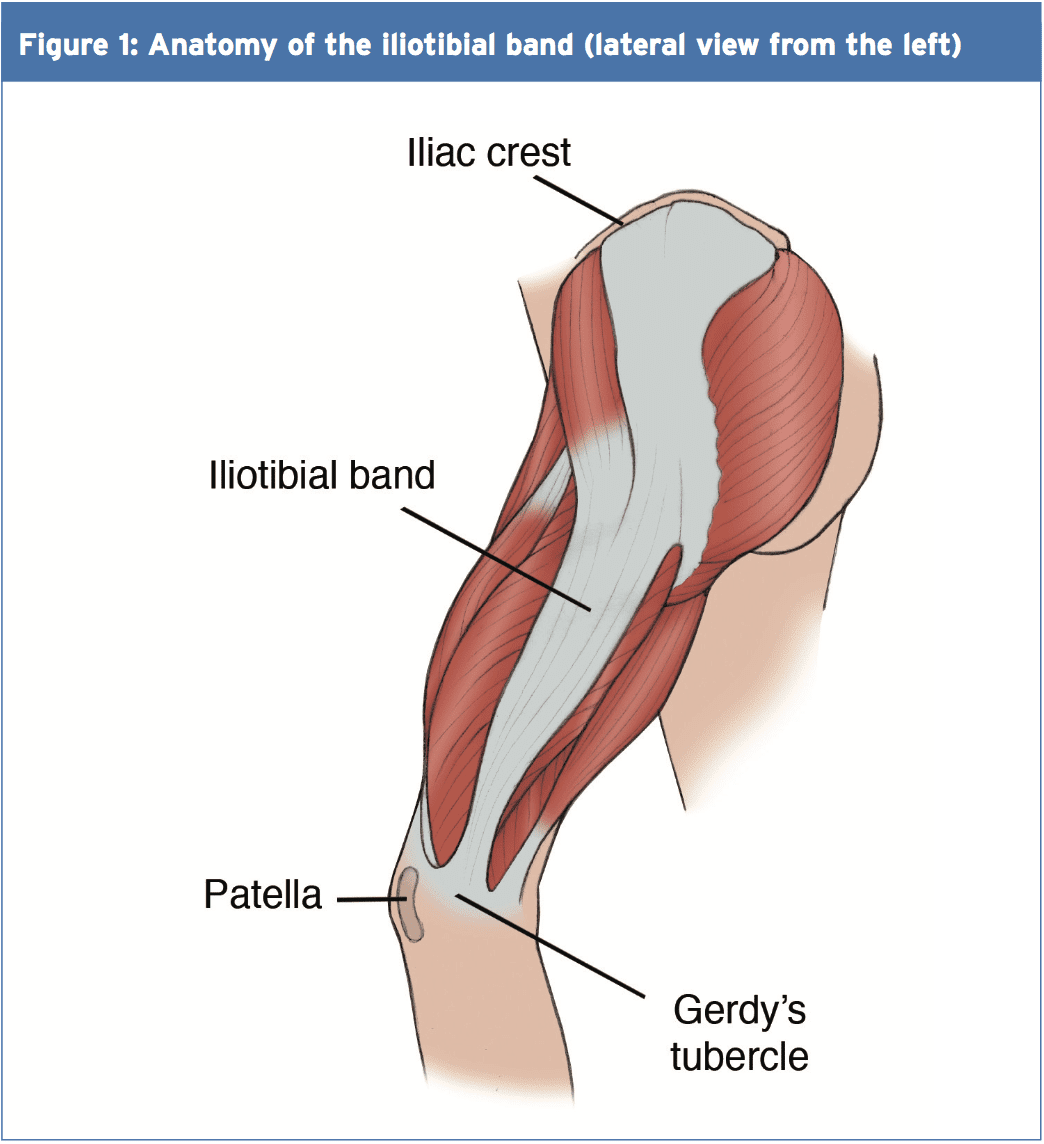 The ITB passively functions to resist hip adduction, hip internal rotation and internal rotation of the knee in accordance with its attachments at the pelvis, femur and tibia(3). The gluteus maximus functions, through its attachment, to increase stability through the hip and knee complex by increasing the tension of the ITB(4). It is possible to see, based on its attachments at both the knee and hip, how changes could bring about the onset of ITBS.
The ITB passively functions to resist hip adduction, hip internal rotation and internal rotation of the knee in accordance with its attachments at the pelvis, femur and tibia(3). The gluteus maximus functions, through its attachment, to increase stability through the hip and knee complex by increasing the tension of the ITB(4). It is possible to see, based on its attachments at both the knee and hip, how changes could bring about the onset of ITBS.
Studies have proposed that as the knee flexes and extends the ITB ‘slides or flicks’ over the lateral femoral condyle of the knee causing an irritation beneath. This notion was debated by Falvey and colleagues (5), who stated that it was highly unlikely that the ITB would flick or slide over the bone during knee flexion due to it not being a loose structure. But the authors did agree that the impact of compression on the richly innervated fat pad was pain’s cause but by strain of the ITB where pain presents crossing the lateral femoral condyle. Strain rate and strain magnitude were measured in a prospective study involving female runners (6). The results indicated that frequency of strain of the ITB at the lateral femoral condyle was greater that the strain magnitude. This implies that a runner might have the ability to run for a short period but then incur lateral knee pain because of the strain to the ITB.
MRI scans have ascertained the knee flexion angle of 30° elicited the greatest compression of the ITB at the point of heel strike, whereas others have said that maximal compression occurs between 20-30°(2,6). A knee flexion angle at the point of heel strike has been found to be significantly different with 20.6° in ITBS patients compared to 15.3° in the control(7). Downhill running produces a greater knee flexion angle at the point of heel strike eliciting a larger strain load to the ITB and therefore this is often a main precursor to ITBS (6). Although an elevated knee flexion angle at the point of heel strike has been considered to contribute to ITBS, it is essential to examine the lower extremity from the frontal and transverse planes too and not solely from the sagittal plane (2).
Rearfoot Eversion
It’s possible to envisage how rear foot eversion could contribute to ITBS causing internal rotation of the tibia resulting at the distal attachment in greater strain of the ITB. In contrast Ferber and colleagues (2) indicated that there was no significant difference in the peak eversion angle of the female subjects, who were previously diagnosed with ITBS but were now symptom free, compared to controls. In a similar study non-significant differences were found between the currently symptomatic ITBS patients and controls for rear foot eversion (8).
Louw & Deary(3) found that ITBS patients sometimes demonstrated decreased eversion angles, accompanied by decreased internal rotation of the knee, at the point of heel strike. Ferber and colleagues (2) noted an increased inversion moment in the ITBS group which was suggested to control and limit the eversion moment. By comparison, currently symptomatic ITBS patients demonstrated a substantial difference compared to a control group with twice the rear foot motion during running (9).
Knee Internal Rotation
Peak internal rotation angle of the knee was found to be significantly greater in the ITBS patients when compared with controls at the point of heel strike (2). This research was supported by other studies who also found a significant effect for increased internal rotation of the knee following a run of moderate intensity to physical exhaustion(7). With excessive rotation comes compression due to increased strain of the ITB at the attachment.
An explanation of increased internal rotation of the knee was attributed to excessive external rotation of the femur perhaps due to shortening of the piriformis, gemellus inferior and superior and the obutrator externus (8). The authors added that excessive rotation at the hip might result from muscular activity of the rotators that were hip being the medius, minimus and the tensor fascia latae. These studies(2,7) were retrospective in design in that they tested healthy runners with a history of ITB pain, whereas(8) was a prospective study of patients with ITBS at the point of testing.
Hip Adduction Angle & Hip Abductor Strength
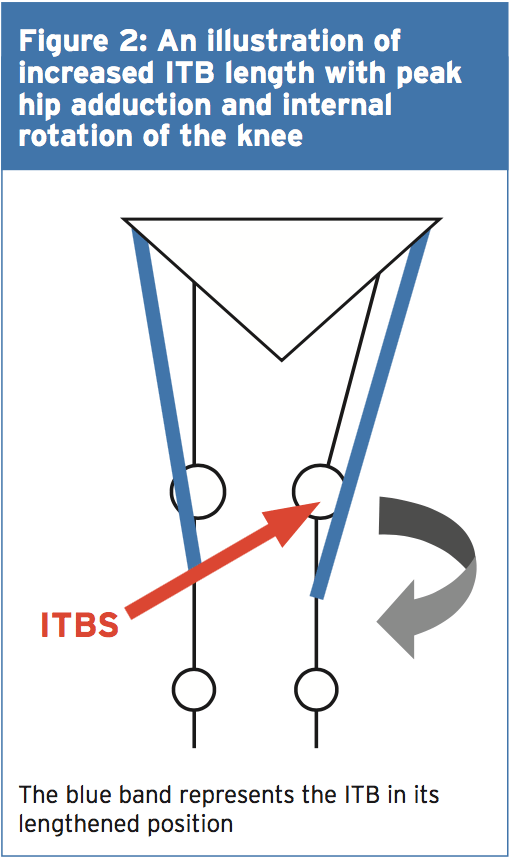
The hip adduction angle during the stance phase has been suggested to be greater. Ferber and colleagues(2) found that the peak hip adduction angle was significantly greater in the ITBS cohort and stated that with 95% confidence. Increased angle results in increased stress to the ITB and consequently increased compression at the lateral femoral condyle when combined with increased internal rotation of the tibia.
Figure 2 illustrates, when peak hip adduction and internal rotation combine, how this may result in increased the compression of the ITB at the lateral femoral condyle. Louw and Deary(3), however, stated that it remained inconclusive whether the peak hip adduction angle was a substantial element. Additional research is therefore required to support Ferber and colleagues'(2) initial findings as this study was a retrospective study carried out on healthy female runners with a history of ITBS.
 Hip Abductor Strength
Hip Abductor Strength
It’s been proposed that an increased peak hip adduction angle may coincide with hip abductor activity involving the gluteus medius in this group. During the stance phase of gait the gluteus medius functions to keep stability. Research has indicated that during stance the adduction forces can exceed three times an individual’s body weight(3). What’s more, it was stated that these forces were beyond the metabolic capacity of the gluteus medius to main pelvic stability during the stance phase using just this muscle alone(3).
Louw and Deary (3) were not able to identify a heightened hip abductor moment in the ITBS patients with increased peak hip adductor angles and suggested that it was more of an issue of timing as opposed to the size of the hip abductors. Louw and Deary (3) stated that the research is yet to examine trunk and pelvic movements in ITBS patients and it is plausible to suggest that biomechanical changes from higher up the kinetic chain has the potential to be a contributing element in ITBS etiology.
A research study of 24 (14 female, 10 male) patients with ITBS undertook a six-week rehabilitation programme to increase the strength of the hip abductors(10). Following six weeks of hip abductor strengthening to running 22 patients reported being pain-free and had returned. The female patients reported an average hip abductor torque increase of 34.9% and the male patients found 51.4% increase. However this study used a hand held dynamometer to measure isometric strength and therefore Fedricson (10) findings should be viewed with caution.
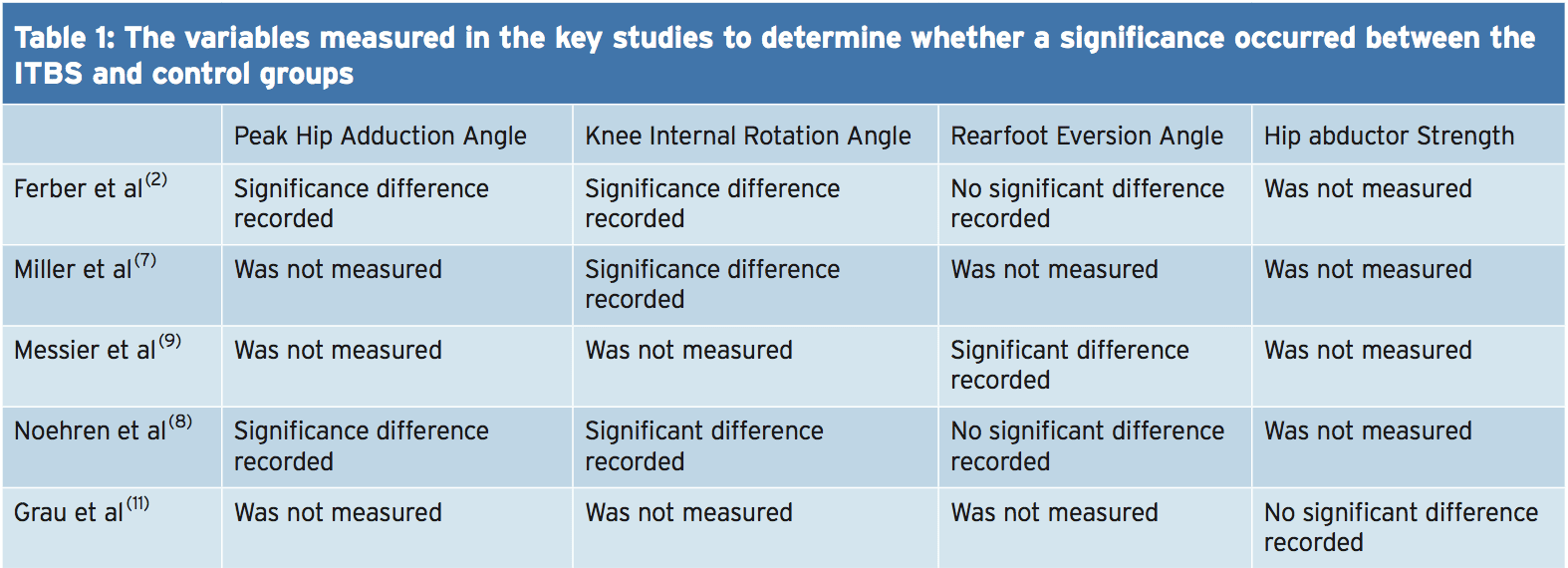
A more recent study assessed the hip abductor strength of currently symptomatic patients with healthy controls in a fixed position(11). The results indicated that no substantial differences occurred for static and dynamic hip abductor strength between the groups. Further research should look into the EMG and strength of the hip abductors in the role of managing ITBS. Table 1 shows of significance in the some of the variables of the studies used in this text.
 Rehabilitation programs, following periods of immobilization and during, should include gluteal exercises to provide stability to the leg that is involved. If active exercises for the gluteal muscles are provided in a manner that is secure and effective then this can influence the period of transition from non weight. It’s prudent based on the research provided to date to develop function although research is lacking in terms of quality and volume as to the biomechanical influences on the etiology of ITBS. This guarantees that once load bearing commences that the leg that is involved has the stability and control that is active to keep the beginning of load of the ITB.
Rehabilitation programs, following periods of immobilization and during, should include gluteal exercises to provide stability to the leg that is involved. If active exercises for the gluteal muscles are provided in a manner that is secure and effective then this can influence the period of transition from non weight. It’s prudent based on the research provided to date to develop function although research is lacking in terms of quality and volume as to the biomechanical influences on the etiology of ITBS. This guarantees that once load bearing commences that the leg that is involved has the stability and control that is active to keep the beginning of load of the ITB.
Summary
The recent review published by Louw and Deary(3) indicates that much of the research published within the literature depending on the etiology of ITBS is inconclusive. The level of research is relatively low and is based on retrospective trials. The research does indicate that knee biomechanics and abnormal hip is involved in the occurrence of ITBS. The authors ascertain that muscle strength is involved as is foot biomechanics that are abnormal. It is recommended that future research should measure kinematic movements of the hip and knee during downhill running as this is a complaint of ITBS onset.
 References
References
1.Clini J of Sports Med, May 2006,16, (3), 261-268
2.J of Sports Phys Therap, Feb, 2010, 40, 2, 52-58.
3.Phys Therap in Sport, 2014, 15, 64 e75.
4.Surgic and Radiologic Anatomy (Dec) 2004; 26, (6), 433 – 446
5.Scand J of Med & Sci in Sports, Aug 2010, 20 (4), 580-587.
6.Clini Biomech, 2008, 23, 1018-1025.
7.Gait Posture. 2007 Sep, 26 (3), 407-13
8.Clini Biomech, Nov 2007, 22 (9), 951-956.
9.Med Sci in Sport & Ex, 1995, 27, 951-960.
10.Clini J of Sports Med, 2000, 10:169–175.
11. Int J of Sports Med, Jul, 2008, 29 (7), 579-583.
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice.*
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


