Muscle cramp and muscle spasm: Three types of muscles make up the body.
- Cardiac muscle makes up the heart.
- Smooth muscle cells line the blood vessels, gastrointestinal tract, and organs.
- Skeletal muscles attach to the bones and are used for voluntary movements.
A muscle spasm happens when skeletal muscle contracts and does not go back to its relaxed state. Spasms are forceful and involuntary. A muscle spasm that sustains/continues is a muscle cramp. The leg muscles, especially the quadriceps/thigh, hamstrings/back of the thigh, and gastrocnemius/calves, are prone to cramping, but any skeletal muscle can cramp. Charley horse is another name for a muscle cramp.
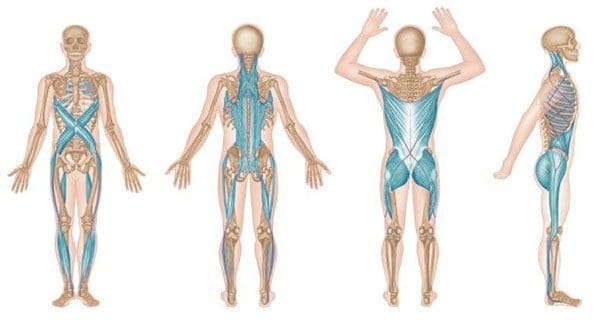
Table of Contents
Causes
There can be a variety of causes for muscle cramps. This includes:
- Physical exertion in hot weather
- Overexertion
- Dehydration
- Electrolyte imbalance
- Physical deconditioning
- Certain medications and supplements could contribute to muscle cramping.
Muscle Symptoms and Anxiety
Generalized anxiety disorder or GAD can include symptoms like:
- Muscle aches
- Muscle tension
- Muscle twitching
- Symptoms that usually accompany anxiety:
- Fatigue
- Sweating
- Nausea
- Shortness of breath
Most times, muscle cramps are not a cause for alarm. However, there are times when cramps could be indicating a more serious health issue like:
- Liver cirrhosis
- Atherosclerosis
- ALS
- Thyroid disorders
- Problems or issues with the spine or spinal nerves.
Signs and Symptoms
- They can range from mild discomfort to incapacitating throbbing pain.
- The muscle that is cramping could look distorted or look like a knot.
- Muscle twitching could present.
- The area of the cramp could be firm/sensitive to the touch.
- Some last just a few seconds.
- Others can last 15 minutes or more.
Medication Causation
Medications can cause cramps through differing mechanisms. These include:
- High blood pressure medications
- Insulin
- Birth control pills
- Cholesterol-lowering medications
- Certain types of asthma medications – beta-agonists
They can interfere with electrolyte levels, contribute to the breakdown of muscle tissue, and/or interfere with blood circulation. Any medication-related muscle cramping should be reported to a doctor.
Night Cramping
Night cramping, especially in the calves, is common and affects up to 60% of adults. Women are more prone to night-leg cramps than men. They are also common with age and a common contributor to insomnia. Muscle fatigue and nerve dysfunction are believed to be a factor. Management remedies include:
- Stretching
- Self-Massage
- Topical muscle pain ointments/creams
- Ice therapy
Remedies and Treatment
The majority of cramps resolve on their own within a few minutes without treatment.
- It is recommended that as soon as a cramp begins, stop the activity.
- Stretch and massage the area,
- Hydrate with water and, if necessary healthy sports drink to replenish sodium, vitamins, electrolytes, and more.
- Apply heat to help relax the muscle.
- Apply an ice pack.
- Nonsteroidal anti-inflammatory medications (NSAIDs) can help if the pain is substantial.
- Consult a doctor if cramps are severe or are recurring often.
Prevention
Strategies for reducing the risk include:
- To vary exercise routines
- Maintain proper hydration
- Maintain proper levels of electrolytes. Sodium and potassium are lost during physical activity, especially in the heat and with consistent sweating.
- Regular Stretching
- Warm-up with a quick jog or quick walk before stretching the body.
Body Composition
Insulin and the body
Insulin assists the transport and storage of energy glucose to cells, tissues, and organs. These include the body’s glucose storage like the skeletal muscles and liver. Once the blood sugar returns to a base level as the glucose is absorbed, the pancreas begins producing glucagon instead of insulin. Glucagon tells the liver to release the stored sugar, which typically happens between meals. What happens to the body when eating too much sugar and carbohydrates than the glucose-storing organs can handle?
Individuals with Type 1 diabetes have a pancreas that does not produce insulin. Type 1 diabetics need to control their glucose levels with lifelong insulin therapy.
With Type 2 diabetes, the pancreas ends up producing insulin through frequent outbursts. When this starts to happen more than normal, the cells eventually lessen their insulin sensitivity. The body becomes numb to the signaling that there is excess blood sugar in the body. This is what happens in individuals with insulin resistance or Type 2 diabetes. This type of diabetes can be managed or prevented with diet adjustments.
References
AAOS: “Muscle Cramps.” Jun. 2017.
American Academy of Orthopedic Surgeons: “Muscle Cramp.”
American Academy Physician: “AAN Recommendations on Symptomatic Treatment for Muscle Cramps.”
American Family Physician: “Nocturnal Leg Cramps.”
American Osteopathic Association: “Muscle Cramp – A Common Pain.”
Journal of the American Academy of Orthopedic Surgeons: “The Athlete With Muscular Cramps: Clinical Approach.”
National Cancer Institute: “Muscle Types.”
National Institute of Mental Health: “What Is Generalized Anxiety Disorder?”
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


